Irreversible electroporation versus radiofrequency ablation for malignant hepatic tumor: A prospective single-center double-arm trial
Boyu Liu, Dianxun Fu, Yong Fan, Zhe Wang, Xu Lang
Department of Radiology, Tianjin Medical University General Hospital, Anshan Road 154#, Heping District, Tianjin, 300052, China
Keywords:Irreversible electroporation Radiofrequency ablation Efficacy Intermediate-term survival Prospective trial
ABSTRACT
1. Introduction
Malignant liver tumors include both primary and secondary tumors.Ablation therapy is an effective standard treatment for unresectable hepatocellular carcinoma(HCC).Partial hepatectomy and ablation therapy achieve the same radical cure effect in the treatment of solitary and small HCCs (≤3 cm). Partial hepatectomy offers longer OS and PFS than RFA for patients with recurrent hepatocellular carcinoma (RHCC). Nevertheless no statistically significant difference was observed in these outcomes for a single RHCC ≤3 cm.1,2
For secondary tumors,partial hepatectomy and ablation therapy are used for isolated hepatic metastatic lesions when systemic therapy fails or are used as a local treatment combined with systemic therapy.The 5-year overall survival rate of colorectal cancer with isolated hepatic metastasis with partial hepatectomy or ablation therapy is approximately 20%,3which is an impressive figure for metastatic disease.
Widely used ablation therapies include radiofrequency ablation(RFA) and microwave ablation (MWA), and the limitation of ablation therapy is the heat sink effect. Thermal ablation of tumors adjacent to large vessels or bile ducts is affected by the cooling effect of the liquid flow in the lumen,leading to incomplete ablation.
Irreversible electroporation (IRE) is a non-thermal (energy-based)ablation technique that avoids the heat sink for tumors near the vessels or biliary tracts.4The electrodes apply high-frequency electrical pulses to both ends of the cell. The electric pulses irreversibly permeate the membranes,thereby inducing cell death.Irreversibly permeabilized cells are left in situ and are removed by the immune system.5Because the extracellular matrix component lacks the cell membrane structure, it theoretically does not cause damage. Although hyperthermic ablative changes have been observed in some studies, mathematical models for calculating the electrical potential and temperature field in tissues during electroporation prove that it is under control.5–7The safety and efficacy of IRE in malignant liver tumors have been proven;therefore,IRE can be used as a possible option for patients with liver tumors that are contraindicated for standard ablation.8–16The efficacy of IRE directly compared with that of RF,which is the most prevalent thermal ablation technique,has rich clinical value.A retrospective analysis of IRE/RF in a single-center propensity match comparison obtained equivalent results for 1-, 2-, 5-years local recurrence-free survival.8This study reports a prospective single-center,double-arm clinical trial of IRE/RF.
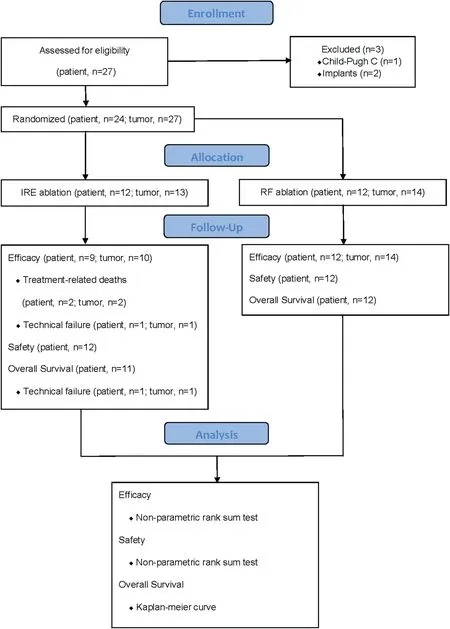
Fig. 1. Flow diagram.
2. Materials and methods
2.1. Study design
This prospective double-arm clinical trial of IRE/RF was approved by the institutional review board of the General Hospital of Tianjin Medical University.This study included 24 patients with malignant liver tumors between November 2018 and September 2019. The patients and their families signed relevant agreements to voluntarily participate in the randomized controlled clinical trial of IRE/RF for the treatment of liver tumors.All patients and their families were informed of the operational risks and complications and then signed informed consent forms.Patients were randomly divided into the IRE and RF groups(Fig.1).
All patients with liver metastases underwent resection of the primary lesion regardless of postoperative recurrence in situ. All tumors were confirmed by pathological diagnosis using surgical specimens or percutaneous liver puncture biopsy (Table 1). All preprocedural imaging studies(CT/MRI)and laboratory baseline examinations were performed within a week. The procedure was performed under CT guidance usingpreoperative and intraoperative images of the target tumors to plan the needle puncture path.An enhanced CT scan was performed immediately after the surgery to evaluate the ablation effect. Patients were followed up with 1-week and 1-month enhanced CT for complication assessment,and 3-month enhanced CT for technical success evaluation.
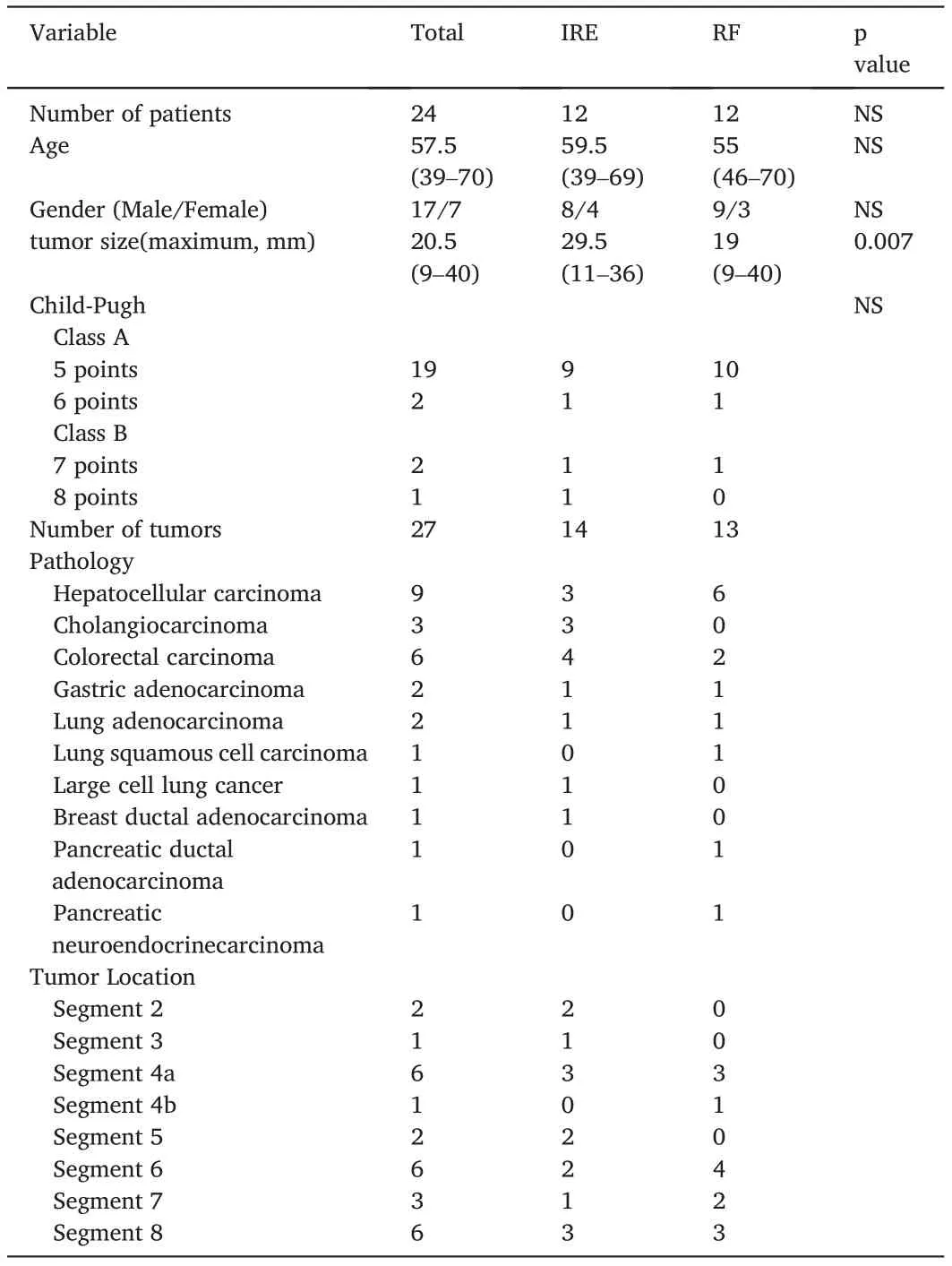
Table 1 Patient characteristics.
2.2. Randomization procedure
This trial was conducted using stratified area-group randomization.Randomized codes were generated according to the ratio of the control and test groups.Each patient chose a random envelope marked with the group accepted by the subject.
2.3. Inclusion criteria
Patients were included if (1) aged 18–70 years, male or female; (2)diagnosis of HCC or other cancers with hepatic metastasis via CT scan or dynamic contrast-enhanced MRI; (3) tumor size ≤4 cm (4) presence of 1≤tumor≤3; (5) Eastern Cooperative Oncology Group (ECOG) score of 0–2;(6)life expectancy of at least 6 months;(7)Prior Informed Consent Form;and(8)Child-Pugh A/B.
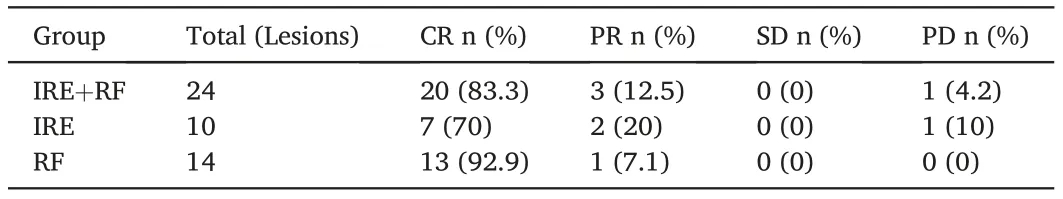
Table 2 Local ablation control evaluation by mRECIST.
2.4. Exclusion criteria
Patients were excluded if they had(1)severe infectious diseases such as bacteremia and toxemia; (2) had severe coagulation dysfunction; (3)had serious heart, brain, lung, and other diseases; (4) had any active implanted device (e.g., pacemakers or defibrillators, electronic devices,and metal parts); (5) had a history of epilepsy; (6) had arrhythmia; (7)had an acute myocardial infarction within six months;(8)were pregnant and lactating or women of child-bearing potential who were not using an acceptable method of contraception;(9)have received treatment with an investigational agent/procedure within 30 days;and(10)had any other factor that the researchers believed were not suitable for inclusion in the study.
2.5. Ablation procedure
IRE procedures were performed under general anesthesia using nondepolarizing muscle relaxants, cardiac synchronization devices, and monitoring. The ablation device was a nano-knife system (AngioDynamics, Latham, New York) and was operated in accordance with the manufacturer’s guidelines.According to this suggestion,a test pulse was applied to verify the current validity and assess the voltage risk.4,15According to the targeting strategy, an IRE session occurs between every pair of electrode needles. The IRE session parameters were as follows:electric field,1500 V/cm needle distance;pulse length,90 μs;pulses per cycle, 70; and active tip length, 1 cm. The planned treatment zone was designed with a 5–10-mm margin around the index tumor margin, and targeting was performed under operative CT guidance. To prevent the risk of channel transmission, we pulled the cover back before insertion and pullout. The successful ablation zone was deduced by immediate post-procedure enhanced CT and the current graphs for an overall upward trend for each probe pair and for a slightly angled upward cluster plateau.4
The RF procedures were performed under general anesthesia and ECG monitoring. The ablation device was comprised of a radiofrequency generator and electrode needles(Medsphere,Shanghai,China).Ablation standards and guiding methods followed the IRE.
2.6. Patient follow-up
Patients were censored at the time of death or the last follow-up prior to the end of data collection,whichever occurred first.
3. Statistics
Baseline, efficacy (mRECIST), and complication (Clavien-Dindo) results were verified using a nonparametric rank-sum test. Related factor analysis was conducted using ordinal/multiple logistic regression analysis.Survival rates were calculated using the Kaplan–Meier method and compared using a log-rank test. Statistical significance was set at P <0.05. Statistical analyses were performed using SPSS version 25 (IBM Corp.).
4. Results
A total of 24 patients with 27 lesions were included in the study,and 21 patients with 24 lesions were evaluated at 90 days. Twenty-three patients completed the follow-up process before the study. Two patients failed to complete the follow-up owing to procedure-related deaths. One patient was excluded from the trial due to technical failure, and only complication data were included in the study for this patient.
4.1. Efficacy
Local ablation control evaluation at 90 days was reported usingmRECIST.18The RF group showed a higher CR rate than the IRE group(92.9% vs. 70%), and there were no PD lesions in the RF group. Nevertheless,there was no statistical difference between the IRE and RF groups in terms of efficacy (p = 0.48) (Table 2). Ordinal logistic regression analysis showed that tumor size(maximum)was associated with ablation grade(p=0.038),whereas independent group analysis showed that the association was not significant(IRE,p=0.159;RF,p=0.982).Ordinal logistic regression analysis with unordered categorical variables,such as pathology, tumor location (liver segment), and nearby vessels, showed no statistical difference between the IRE and RF groups(every dependent variable p >0.05),and subgroup analysis showed similar results.

Table 3 Complication assessment with Clavien-Dindo classification.
4.2. Complications
Adverse events were reported using the Clavien-Dindo classification19(Table 3). The overall complication rate was 58.3% (7/12), and there was no statistical difference between the IRE and RF groups in terms of complication rate(p=0.887).The RF group had a higher rate of grade II complications than the IRE group (50% vs. 25%, respectively).Recorded grade II complications included transaminase, bilirubin, ascites, hemogram, and portal vein complications with drug treatment.Major complications (grades IV-b and V) occurred in the IRE group.Subcapsular hematoma,a procedure-related complication,was observed in the RF group. The complications were analyzed using regression analysis which included related factors.The Child-Pugh score showed a trend towards significance(p=0.051)and may predict the complication distribution in the IRE group (p = 0.034). In the subgroup analysis,nearby vessels showed a trend towards significance (p = 0.052) in the IRE group.
4.3. Intermediate-term survival
Twenty-three patients completed the follow-up period prior to the study endpoint. Thirteen patients survived for 24 months after surgery(Fig. 2). Average overall survival was 18.17 months (95% CI 15.00-21.26) and was 17.55 months in the IRE group (95% CI 12.48-22.613)and 18.75 months in the RF group (95% CI 15.13-22.366). The logrank (Mantel-Cox) test showed no statistical difference in OS between the IRE and RF groups(P= 0.959).
5. Discussion
IRE ablation has been proven to be safe,effective,and less damaging to the vessels and bile ducts around the lesion than thermal ablation.8–10,12–17,20–23IRE is considered an alternative ablation treatment for unresectable hepatocellular carcinoma or malignant liver tumors,where thermal ablation is unsuitable.
Several clinical studies have compared the efficacy of IRE/thermal ablation with short-/long-term follow-up.8,15Freeman et al. reported a retrospective study that showed a similar local recurrence rate between IRE and RF groups(10/25 vs.27/96,p=0.25).The local recurrence-free survival rates at 1,2-and 5-years were not statistically different between IRE and RFA (80.4%, 69.1%, and 44.9% versus 84.8%, 71.3%, and 52.1%, p = 0.63). The OS at 24 months in our study showed a similar trend and was not statistically different (p = 0.959) (Fig. 2). Bhutiani et al. reported a prospective multi-institutional double-arm treatment registry between IRE and MWA. Both the groups exhibited a 90-day success rate of 100%. IRE ablation resulted in a 180-day success rate of 97% compared with 100% for MWA (p = 0.37). The 90-day CR rate in our study was 92.9%(RF)vs.63.6%(IRE),and the outcome distribution according to the mRECIST was not statistically significant(p= 0.065).

Fig. 2. Kaplan–Meier estimated overall survival of enrolled patients in IRE/RF group.
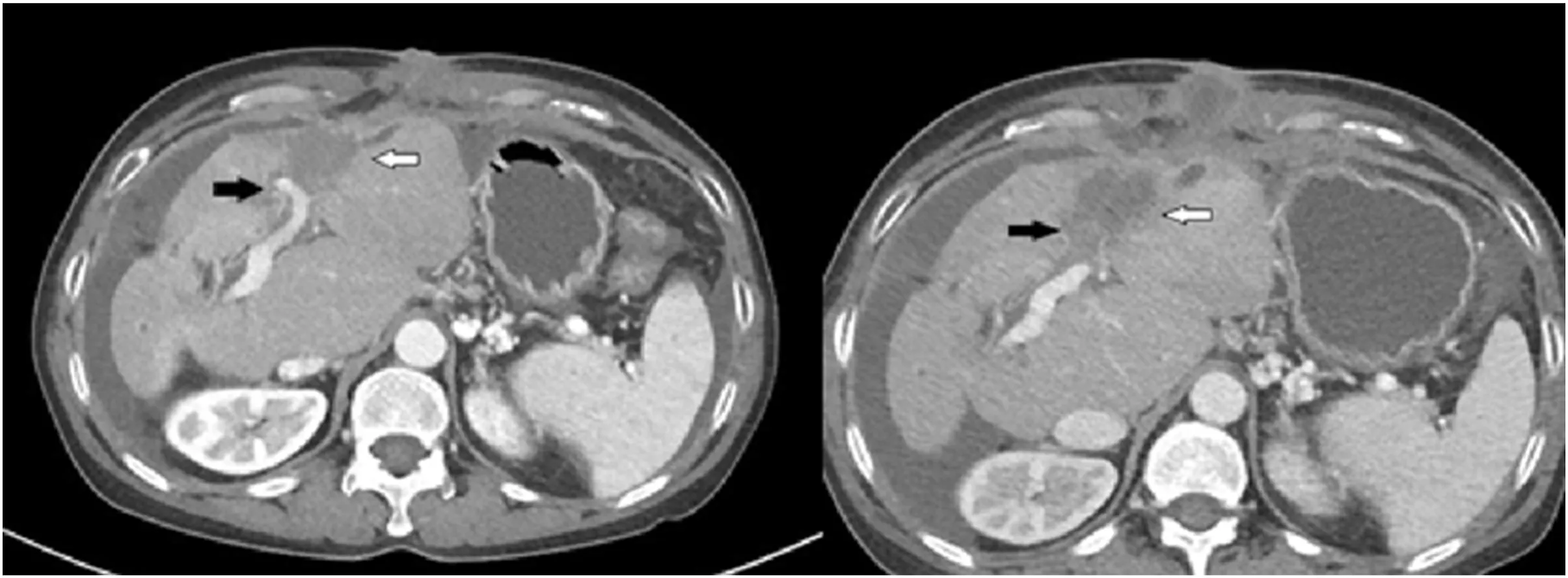
Fig. 3. The white arrow indicates the lesion and the black arrow indicates the left portal vein branch. Occlusion of left portal vein occurred after ablation (Right)compared with before IRE ablation (Left).
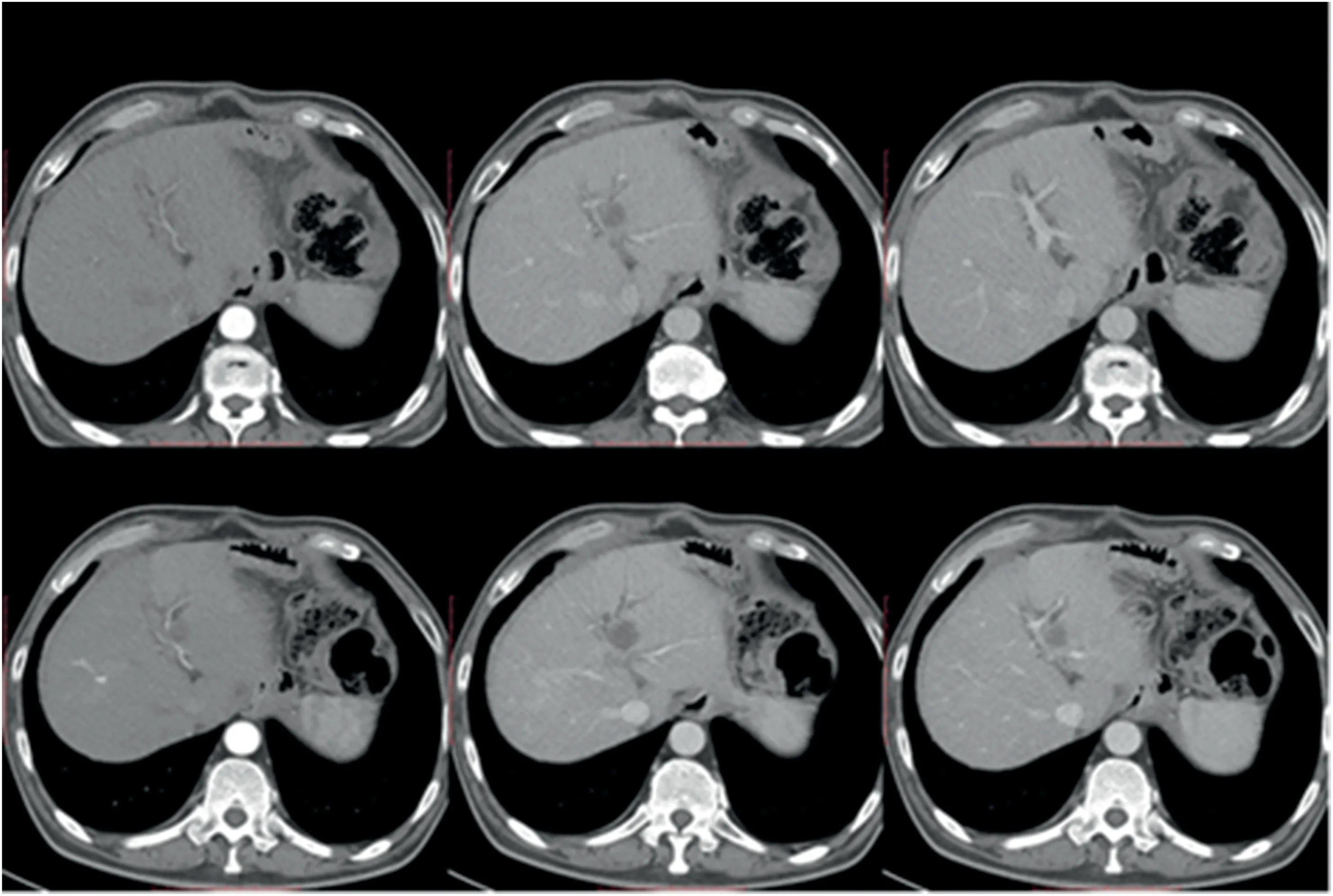
Fig. 4. The images above showed hepatic artery and portal vein morphology before IRE ablation. The hepatic artery was normal and the portal vein happened to multiple stenosis after IRE ablation (bottom of images).
Bulvik et al. indicated the flow of blood in the vessels after IRE ablation in 12-month-old mice through Evans blue staining, and there was no blood supply in the RF area.20Although IRE theoretically does not damage the extracellular matrix components, mild histopathological changes in adjacent vessel walls,such as vasculitis and mild endothelial damage, have been detected in animal studies.6,7,24Dollinger et al.17retrospectively identified 43 patients with 84 hepatic lesions near venous structures after IRE treatment.Vascular changes were found in 19 of the 191 vessels (9.9%), including portal vein thrombosis (n = 2), complete portal vein thrombosis (n = 3), lumen narrowing (n = 14). Narayanan et al.25proposed a greater vulnerability of portal veins to IRE-induced vessel damage due to the special flow dynamics within these vessels.Portal vein thrombosis was detected in our study after IRE(Fig.3,Fig.4),and two patients experienced serious complications (Grades Ⅳ-b and Grades Ⅴ).The nearby vessels showed a trend towards significance(p=0.052)in the IRE group.Prophylactic anticoagulation is an option worthy of reference for lesions near venous structures.
One patient was excluded from the trial due to technical failure. All procedures were designed to be performed under CT guidance,but it was difficult to determine the location of the target tumor on plain CT in this patient. Enhanced CT guidance was attempted, but postoperative magnetic resonance imaging showed that the procedure was unsuccessful.
This study was a prospective,double-arm clinical trial of IRE/RF.All patients meeting the enrollment conditions were randomly divided into IRE or RF groups,but system bias still occurred.In the IRE group,90.9%(10/11)of tumors were >2 cm,and in the RF group,75%(9/12)of tumors were<2 cm.The maximum tumor size(maximum)in the RF group was significantly greater than that in the IRE group (p = 0.007). Kalra et al.10reported a retrospective study of consecutive IRE procedures and found that the maximum tumor diameter was significantly associated with LPFS(local progression free survival)(p =0.045).For this reason,we believe that the RF group had a superiority bias in the efficacy evaluation. At the same time, owing to the relatively small number of patients enrolled in the single-center group, it was difficult to make corrections.
Regrettably, owing to the impact of the COVID-19 epidemic, the follow-up of patients in the later stages was inhibited. Only basic information could be obtained for remote patients through telephone followups. The incomplete contents of this section are not listed here. Further work on re-tracking the records and providing detailed long-term data analysis will be conducted as long as the epidemic passes.
In conclusion, IRE ablation reveals similar efficacy and safety in a short-term follow-up and similar OS in mid-term survival with RF ablation for the treatment of malignant hepatic tumors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
 Journal of Interventional Medicine2022年2期
Journal of Interventional Medicine2022年2期
- Journal of Interventional Medicine的其它文章
- Advances in the interventional therapy of hepatocellular carcinoma originating from the caudate lobe
- The underlying molecular mechanism of intratumoral radiofrequency hyperthermia-enhanced chemotherapy of pancreatic cancer
- The apoptotic effect of ozone therapy on mitochondrial activity of highly metastatic breast cancer cell line MDA-MB-231 using in vitro approaches
- Preparation and investigation of a novel iodine-based visible polyvinyl alcohol embolization material
- Intrahepatic flow diversion prior to segmental Yttrium-90 radioembolization for challenging tumor vasculature
- Safety and efficacy of transcatheter arterial embolization for management of refractory hematuria of prostatic origin
