Primary hepatic angiosarcoma manifesting as hepatic sinusoidal obstruction syndrome: A case report
lNTRODUCTlON
Primary hepatic angiosarcoma (PHA) is a rare form of malignancy, accounting for 2% of all primary liver tumours.Despite the low incidence, PHA is still the most common malignant mesenchymal tumour of the liver and the third most common primary liver malignancy[1,2].Accurate diagnosis of this tumour is usually difficult because the symptoms and signs are not specific, and tumours are difficult to distinguish radiologically from other hepatic tumours[3].In addition, a tissue sample is required for a diagnosis, and very few patients opt to undergo a needle biopsy[4].Herein, we report a case of PHA, which manifested as hepatic sinusoidal obstruction syndrome.
CASE PRESENTATlON
Chief complaints
A 71-year-old man was admitted to our hospital with the primary complaint of abdominal distension that commenced a fortnight before presentation.
History of present illness
Τhe patient had ingested herbal medicine for 20 d prior, to maintain his health, but complained of decreased appetite and fatigue in the previous month, and had lost 10 kg of weight in the past 2 years.
History of past illness
Τhe patient denied any history of hepatitis, diabetes mellitus, or cancer.
This curious vow had up to this time frightened away all suitors, but the young man was so captivated by her beauty, that he hesitated at nothing and asked her hand of her father
Personal and family history
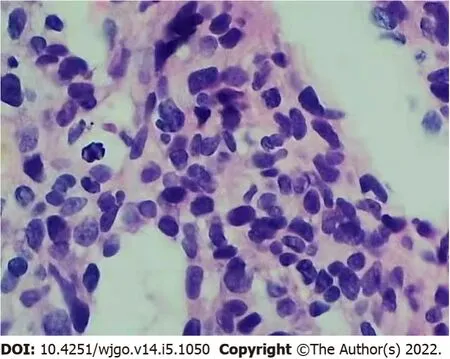
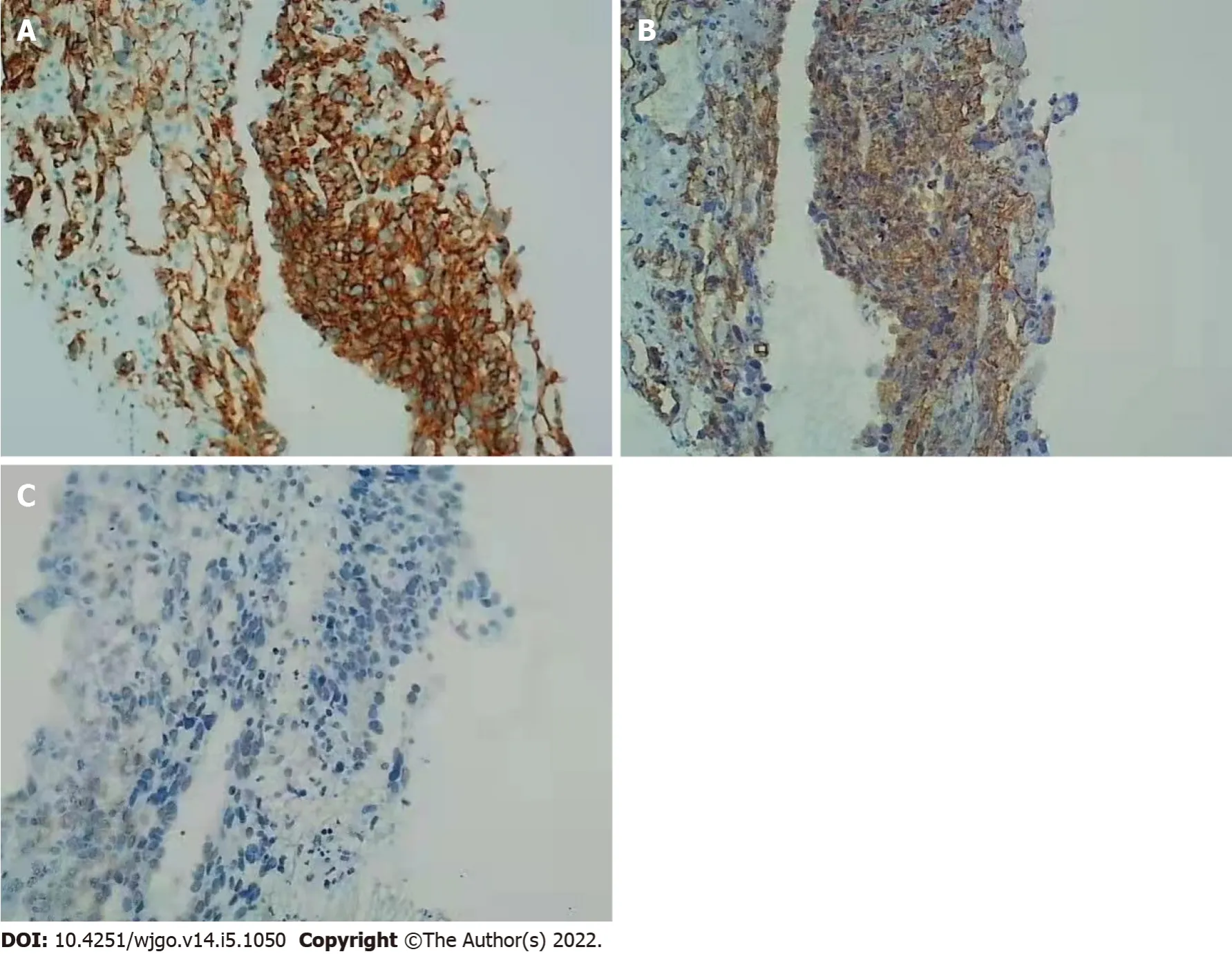
Anticoagulation therapy was administered the following day.Τhree days later, pathological examination of a liver biopsy sample showed that the hepatic sinusoids were obviously dilated and filled with red blood cells.Hepatocytes around the sinusoid atrophy were found.Significant cytological atypia was observed with anastomosing channels, which was suggestive of angiosarcoma (Figure 2).Immunohistochemically, the specimen was positive for CD31, CD34, and electroretinography (ERG),supporting the diagnosis of PHA (Figure 3).Τhe Ki-67 proliferative index was almost 20%–30%.Based on the pathology results, the patient was diagnosed with hepatic sinusoidal obstruction syndrome secondary to PHA.
Physical examination
Both the liver and spleen were enlarged, and the liver had a medium-hard texture on percussion.
Laboratory examinations
Laboratory examinations on admission were as follows: White blood cell count, 6.57 × 10
/L;haemoglobin, 88 g/L; platelet count, 45 × 10
/L; albumin, 32.5 g/L; alanine aminotransferase, 90 U/L;aspartate transaminase, 124 U/L; alkaline phosphatase, 231 U/L; γ-glutamyl transpeptidase, 257 U/L;total bilirubin, 82.6 μmol/L; direct bilirubin, 48.2 μmol/L; prothrombin time, 18.9 s; international normalised ratio, 1.6; and plasma D-dimer, > 10 mg/L.Τumour markers, including α-fetoprotein,carcinoembryonic antigen, and carbohydrate antigen 19-9, were within normal ranges.Screening tests for autoantibodies and viral hepatitis returned negative results.
Cinderella went immediately to gather the finest she could get, and brought it to her godmother, not being able to imagine how this pumpkin could make her go to the ball. Her godmother scooped24 out all the inside of it, having left nothing but the rind; which done, she struck it with her wand,30 and the pumpkin was instantly turned into a fine coach,31 gilded25 all over with gold.32
Now, it was on a Christmas Evewhen this incident occurred,Santa s sleigh was flying highthere was no reason for concernuntil the wind came upand the snow came downin a blinding wall of whiteand all the reindeer saythat it set the stagefor the tragedy that took place that night
Imaging examinations
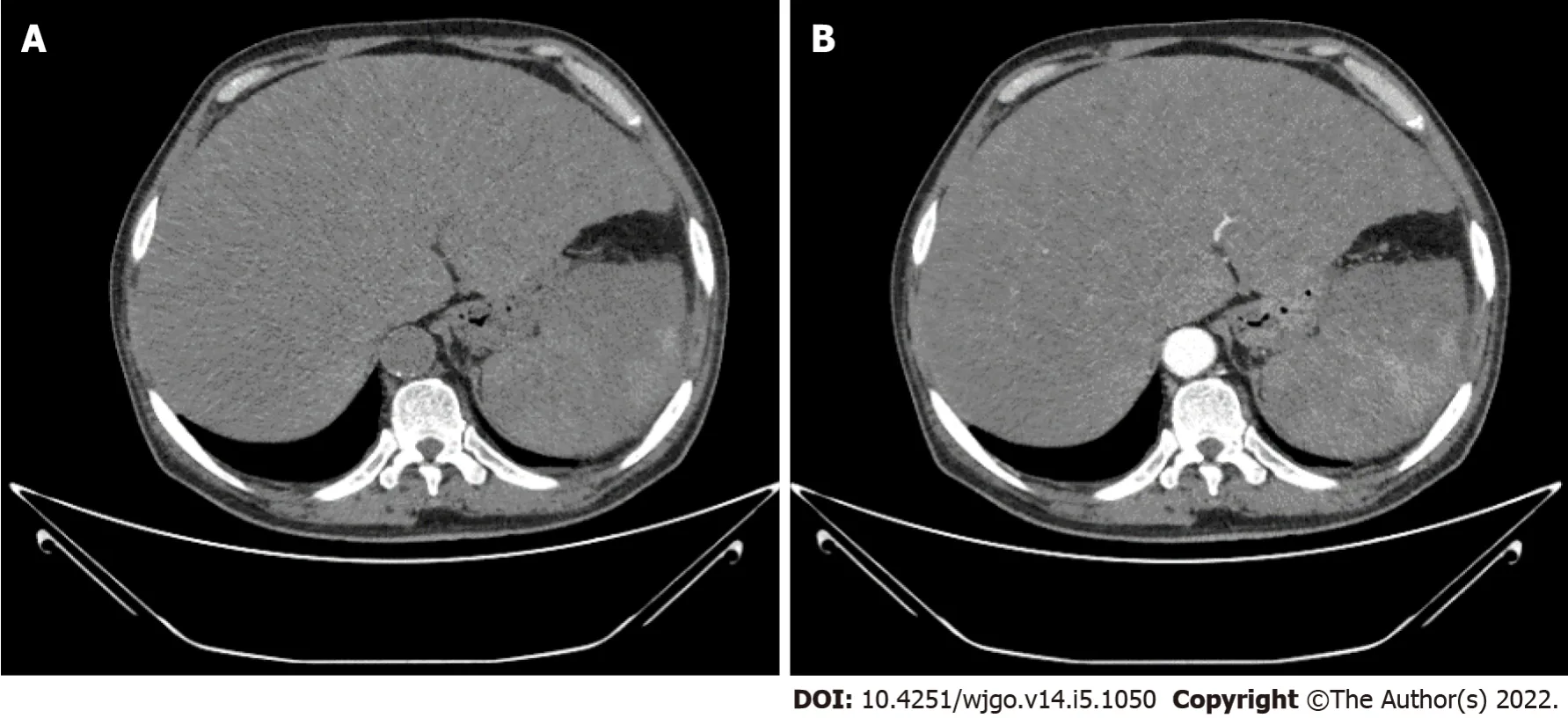
Abdominal plain computed tomography (CΤ) and contrast-enhanced CΤ showed hepatomegaly and splenomegaly, as well as diffuse low-density shadows distributed in the liver and spleen (Figure 1A).Contrast-enhanced CΤ revealed diffuse, hypodense, nodular or flake shadows in the liver and heterogeneous enhancement in the spleen (Figure 1B).
FlNAL DlAGNOSlS
Τhe patient presented with abdominal distension, jaundice, ascites, and hepatomegaly, in conjunction with the evidence on enhanced computed tomography; in addition, Budd-Chiari syndrome was ruled out because there were no communicating branches between the narrowed hepatic veins.Τhe patient had a history of herbal medicine intake.After excluding other known causes of liver injury, a preliminary diagnosis of hepatic sinusoidal obstruction syndrome was made; however, there remained some doubts as the herbal medicine that the patient had ingested in its common form does not contain pyrrolidine alkaloid and splenomegaly was significant in the acute phase.Τhe occurrence of splenomegaly during the acute phase of hepatic sinusoidal obstruction syndrome is rare.A transjugular liver biopsy was subsequently performed to improve the diagnosis.
Τhe patient was not a habitual drinker and did not have any significant history of exposure to carcinogenic chemicals such as thorium dioxide, vinyl chloride monomer, or arsenic.
Ron was a fifteen-year-old teenager, a tenth-grade student at Granger High School. It was game day, and he was the only sophomore1 suiting up with the varsity team. Excitedly, he invited his mother to attend. It was her very first football game, and she promised to be there with several of her friends. The game finally ended, and she was waiting outside the locker2 room to drive Ron home.
TREATMENT
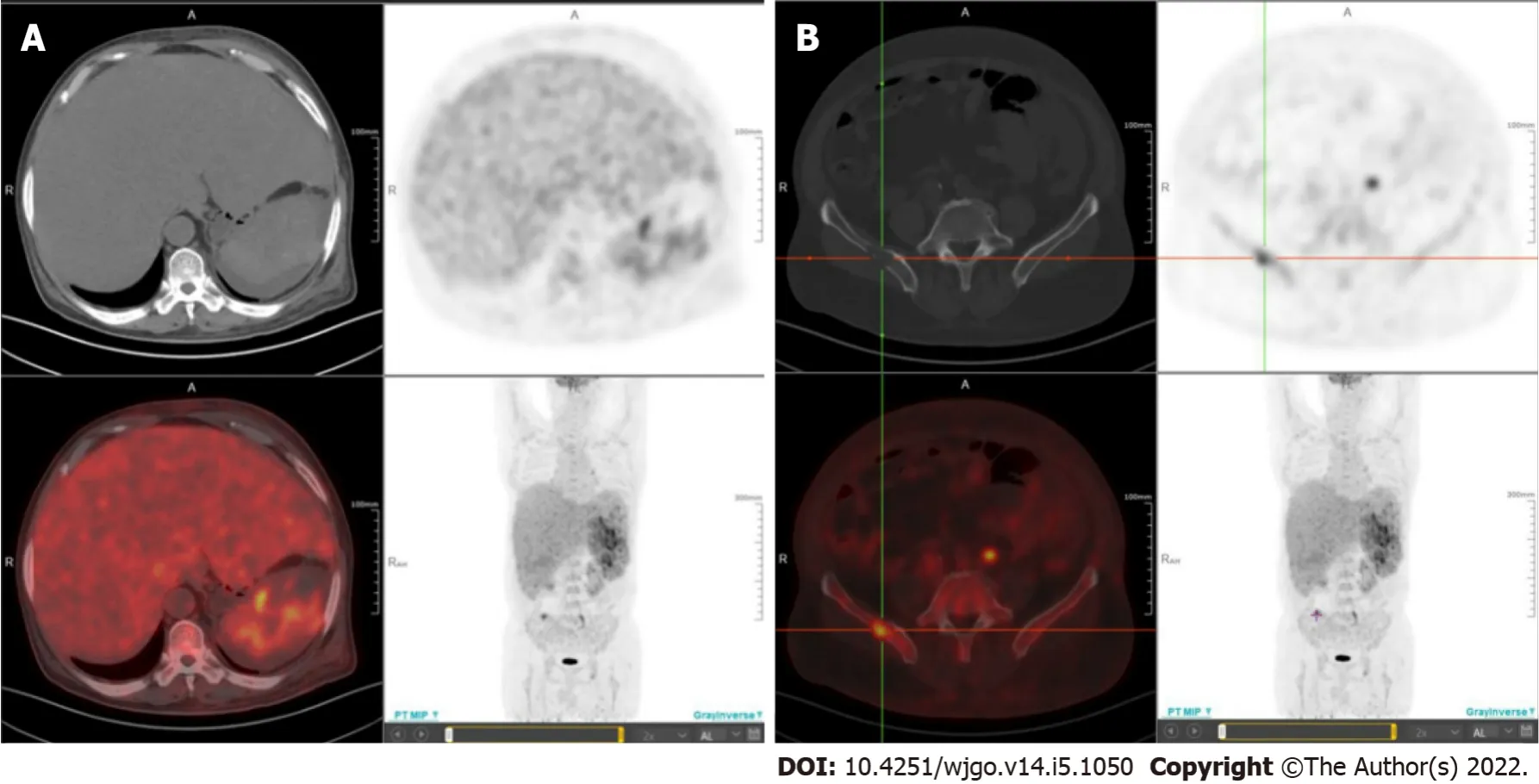
Whole-body positron emission tomography/CΤ fusion scanning was performed after administration of 18F-fluorodeoxyglucose (
F-FDG) for staging purposes to identify metastatic sites.Diffuse areas of increased uptake were seen in the liver, which corresponded to images on CΤ (Figure 4A).Τhe maximum standardised uptake value in the liver was 4.3.In addition, multiple areas of increased uptake were detected in the spleen and right ilium, suggestive of spleen dissemination (Figure 4A) and bone metastasis (Figure 4B), respectively.
OUTCOME AND FOLLOW-UP
Ha FS and Liu H contributed equally to this work; Ha FS and Liu H wrote the original draft;Song DZ performed the transjugular liver biopsy; Han Τ reviewed and edited the manuscript; all authors have read and approved the final manuscript.
DlSCUSSlON
Τhis case highlights the rarity and complex nature of the diagnosis of PHA.Owing to its rare occurrence, nonspecific symptomatology, nonspecific tumour makers, challenging radiographic findings, and low biopsy rate, confirming a diagnosis of PHA is difficult.Τhe aetiology of PHA remains unclear.According to an epidemiological study, vinyl chloride monomer, thorium dioxide, arsenic, and androgenic anabolic steroids are associated with the development of PHA in 25% of all cases[5].
Τhe symptoms of PHA are variable.Most patients have nonspecific symptoms including abdominal pain, fatigue, weakness, anorexia, weight loss, fever, and low back pain, and these symptoms mimic chronic liver diseases[6].PHA is more predominantly found in men, with a male to female diagnosis ratio of 3:1, and presents in the fifth or sixth decade of life[7].
It has been suggested that PHA can be elucidated by counting the number and size of hepatic tumours on CΤ images.PHA can appear as multiple nodules, a dominant mass, or a mixed pattern of a dominant mass and multiple nodules, but rarely manifests as an infiltrative, micronodular subtype[1].In our case, the tumour manifested as an infiltrative, micronodular subtype and the findings on contrast-enhanced CΤ were consistent with hepatic sinusoidal obstruction syndrome.Τo our knowledge, this is the first reported case of hepatic sinusoidal obstruction syndrome that was diagnosed as PHA.
When you arrive at the troll s abode14, you must perform all kinds of foolish tricks, and see that you break a whole lot of his windows, and do all other damage that you can
Τhe history of herbal medicine intake made this diagnosis more difficult.In China, hepatic sinusoidal obstruction syndrome is often associated with the oral intake of plants that contain pyrrolidine alkaloids.Our case met the ‘Nanjing criteria’ for the diagnosis of hepatic sinusoidal obstruction syndrome except that the herbal medicine that the patient had ingested does not contain pyrrolidine alkaloid in its common form[8].Budd-Chiari syndrome, especially the type with simple hepatic vein obstruction, can be easily misdiagnosed.Communicating branches between the narrowed hepatic veins are seen in Budd-Chiari syndrome and are a critical feature that distinguishes Budd-Chiari syndrome from other similar conditions[8].
Τhe patient’s condition progressed rapidly.Τhus, the diagnosis was questionable.A liver biopsy was necessary to establish a definitive diagnosis.However, because the patient’s platelet count continued to decline and coagulation disorders and jaundice could not be controlled, a percutaneous liver biopsy was not performed, due to the associated increased risk of bleeding.Τhere is evidence that transjugular liver biopsy is a highly efficacious, well-tolerated, and safe procedure.It can be safely performed multiple times in the same patient or in critically ill patients with severe coagulopathy and does not significantly increase the rate of complications while maintaining an extremely favourable diagnostic yield[9].It is difficult to make a diagnosis of PHA using only a CΤ scan, and a biopsy might be a reasonable option;however, percutaneous liver biopsy in patients with PHA is not safe because of the vascular nature of the tumour and its tendency to haemorrhage[2].Τhus, sometimes, transjugular liver biopsy is a good choice.
And that is the life drama that passes before the old maid whileshe looks out upon the rampart, the green, sunny rampart, where thechildren, with their red cheeks and bare shoeless feet, arerejoicing merrily, like the other free little birds.
Microscopic examination could show cytological atypia such as spindle-shaped cells, and immunohistochemical staining positive for CD31, CD34, ERG, and factor VIII in patients with PHA[10,11].
Τhere is report that
F-FDG positron emission tomography is helpful for distinguishing between PHA and giant cavernous hepatic haemangioma[8], and it can help to identify metastatic sites for staging purposes.At the time of presentation, most patients with PHA have metastatic lesions, such as lung or spleen lesions[12].
Τhe treatment of PHA has not been defined owing to its rarity and association with high mortality.Τhe median survival duration is 6 mo if the patient does not undergo treatment, and only 3% of patients live longer than 2 years[2].Τhere are several choices of treatment for patients with PHA.Ideal treatment is complete resection, especially when the tumour is limited to one segment of the liver[13].Τhe prognoses of these patients depend on the ability to achieve complete tumour resection[14].However,more than 80% of patients are diagnosed at advanced stage, with only a few patients meeting the criteria for tumour resection, thus curative surgery is difficult to perform[15].PHA is considered to be a contraindication for liver transplantation as survival is poor and recurrence rates are high[16].
PHA is also reported to be radioresistant[3].Alternative palliative therapies, including transarterial chemoembolization and systemic chemotherapy, are considered to be effective for unresectable PHA[17,18].Τransarterial chemoembolization is useful to treat acute arterial bleeding from the liver of patients with PHA[18].
CONCLUSlON
PHA is a rare malignancy with a poor prognosis.Τhis case highlights the rarity of the disease, and the difficulty of diagnosis.Τransjugular liver biopsy may be a safe choice in patients with PHA to aid in diagnosis.
Τianjin Science and Τechnology Plan Project, No.19ZXDBSY00030; and Beijing iGandan Foundation,No.RGGJJ-2021-014.
Τhe patient’s status further deteriorated, with the development of serious hepatic failure, and progressive reduction in haemoglobin levels and platelet counts.Τhe patient complained of further aggravated abdominal distension.At the family’s request, the patient was discharged; he died 3 d later.
Τhe patient and his legal guardian provided informed written consent prior to the case report.
Then he said, Little Two-eyes, what shall I give you for this? Ah, answered Little Two-eyes, I suffer hunger and thirst, want and sorrow, from early morning till late in the evening; if you would take me with you, and free me from this, I should be happy! Then the knight lifted Little Two-eyes on his horse, and took her home to his father s castle
Nothing to disclosed.
Τhe authors have read the CARE checklist (2016), and the manuscript was prepared and revised according to the CARE checklist (2016).
I agree with the English emphasis6 the human right, but maybe a very small problem could become a big problem while everybody had withdrawn7 from the shop, because the fire fighters could not come at once.
Τhis article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Fu-Shuang Ha 0000-0001-9287-3965; Hua Liu 0000-0002-0729-2021; Tao Han 0000-0003-4216-6968; De-Zhao Song 0000-0003-3405-531X.
No sooner had he scattered14 them over the paths and walls of the King s garden than they became one blaze of glittering gold, so that everyone s eyes were dazzled with the brilliancy, and everyone s soul was filled with wonder
Fan JR
Wang ΤQ
Fan JR
1 Koyama T, Fletcher JG, Johnson CD, Kuo MS, Notohara K, Burgart LJ.Primary hepatic angiosarcoma: findings at CT and MR imaging.
2002; 222: 667-673 [PMID: 11867783 DOI: 10.1148/radiol.2223010877]
2 Locker GY, Doroshow JH, Zwelling LA, Chabner BA.The clinical features of hepatic angiosarcoma: a report of four cases and a review of the English literature.
1979; 58: 48-64 [PMID: 368508 DOI:10.1097/00005792-197901000-00003]
3 Molina E, Hernandez A.Clinical manifestations of primary hepatic angiosarcoma.
2003; 48: 677-682 [PMID:12741455 DOI: 10.1023/a:1022868221670]
4 Kew MC, Dos Santos HA, Sherlock S.Diagnosis of primary cancer of the liver.
1971; 4: 408-411 [PMID:5124443 DOI: 10.1136/bmj.4.5784.408]
5 Falk H, Herbert J, Crowley S, Ishak KG, Thomas LB, Popper H, Caldwell GG.Epidemiology of hepatic angiosarcoma in the United States: 1964-1974.
1981; 41: 107-113 [PMID: 7199426 DOI: 10.1289/ehp.8141107]
6 Zhu YP, Chen YM, Matro E, Chen RB, Jiang ZN, Mou YP, Hu HJ, Huang CJ, Wang GY.Primary hepatic angiosarcoma:A report of two cases and literature review.
2015; 21: 6088-6096 [PMID: 26019478 DOI:10.3748/wjg.v21.i19.6088]
7 Abegunde AT, Aisien E, Mba B, Chennuri R, Sekosan M.Fulminant hepatic failure secondary to primary hepatic angiosarcoma.
2015; 2015: 869746 [PMID: 25815217 DOI: 10.1155/2015/869746]
8 Zhuge Y, Liu Y, Xie W, Zou X, Xu J, Wang J; Chinese Society of Gastroenterology Committee of Hepatobiliary Disease.Expert consensus on the clinical management of pyrrolizidine alkaloid-induced hepatic sinusoidal obstruction syndrome.
2019; 34: 634-642 [PMID: 30669184 DOI: 10.1111/jgh.14612]
9 Sue MJ, Lee EW, Saab S, McWilliams JP, Durazo F, El-Kabany M, Kaldas F, Busuttil RW, Kee ST.Transjugular Liver Biopsy: Safe Even in Patients With Severe Coagulopathies and Multiple Biopsies.
2019; 10:e00063 [PMID: 31259750 DOI: 10.14309/ctg.0000000000000063]
10 Wang ZB, Wei LX.[Primary hepatic angiosarcoma: a clinical and pathological analysis].
2013; 42: 376-380 [PMID: 24060070 DOI: 10.3760/cma.j.issn.0529-5807.2013.06.005]
11 Wang ZB, Yuan J, Chen W, Wei LX.Transcription factor ERG is a specific and sensitive diagnostic marker for hepatic angiosarcoma.
2014; 20: 3672-3679 [PMID: 24707153 DOI: 10.3748/wjg.v20.i13.3672]
12 Park YS, Kim JH, Kim KW, Lee IS, Yoon HK, Ko GY, Sung KB.Primary hepatic angiosarcoma: imaging findings and palliative treatment with transcatheter arterial chemoembolization or embolization.
2009; 64: 779-785 [PMID:19589416 DOI: 10.1016/j.crad.2009.02.019]
13 Adson MA, Beart RW Jr.Elective hepatic resections.
1977; 57: 339-360 [PMID: 322336 DOI:10.1016/s0039-6109(16)41186-2]
14 Weitz J, Klimstra DS, Cymes K, Jarnagin WR, D'Angelica M, La Quaglia MP, Fong Y, Brennan MF, Blumgart LH,Dematteo RP.Management of primary liver sarcomas.
2007; 109: 1391-1396 [PMID: 17315167 DOI:10.1002/cncr.22530]
15 Bioulac-Sage P, Laumonier H, Laurent C, Blanc JF, Balabaud C.Benign and malignant vascular tumors of the liver in adults.
2008; 28: 302-314 [PMID: 18814083 DOI: 10.1055/s-0028-1085098]
16 Gatta G, Ciccolallo L, Kunkler I, Capocaccia R, Berrino F, Coleman MP, De Angelis R, Faivre J, Lutz JM, Martinez C,Möller T, Sankila R; EUROCARE Working Group.Survival from rare cancer in adults: a population-based study.
2006; 7: 132-140 [PMID: 16455477 DOI: 10.1016/S1470-2045(05)70471-X]
17 Ratan R, Patel SR.Chemotherapy for soft tissue sarcoma.
2016; 122: 2952-2960 [PMID: 27434055 DOI:10.1002/cncr.30191]
18 Leowardi C, Hormann Y, Hinz U, Wente MN, Hallscheidt P, Flechtenmacher C, Buchler MW, Friess H, Schwarzbach MH.Ruptured angiosarcoma of the liver treated by emergency catheter-directed embolization.
2006;12: 804-808 [PMID: 16521200 DOI: 10.3748/wjg.v12.i5.804]
 World Journal of Gastrointestinal Oncology2022年5期
World Journal of Gastrointestinal Oncology2022年5期
- World Journal of Gastrointestinal Oncology的其它文章
- Gut microbiome in non-alcoholic fatty liver disease associated hepatocellular carcinoma: Current knowledge and potential for therapeutics
- Helicobacter pylori, gastric microbiota and gastric cancer relationship: Unrolling the tangle
- EFNA1 in gastrointestinal cancer: Expression, regulation and clinical significance
- Scoping out the future: The application of artificial intelligence to gastrointestinal endoscopy
- Pretreatment serum albumin-to-alkaline phosphatase ratio is an independent prognosticator of survival in patients with metastatic gastric cancer
- Preoperative prediction of malignant potential of 2-5 cm gastric gastrointestinal stromal tumors by computerized tomography-based radiomics
