Digital single-operator cholangioscopy for biliary stricture after cadaveric liver transplantation
lNTRODUCTlON
Liver transplantation (LΤ) has become a standard of care in patients with end-stage liver disease[1].Despite improvements in surgical techniques, graft preservation technology, immunosuppressive therapy, and close follow-up[2], a biliary stricture is still the most common adverse event (AE) after LΤ,occurring in 5 % to 19 % of patients[3-6].Biliary strictures include a wide array of biliary abnormalities that have different anatomical locations, clinical presentation, and pathogenesis.Biliary strictures after LΤ can be either anastomotic (AS) or non-anastomotic (NAS) based on the morphology and location of stenosis observed during imaging procedures[7,8].AS account for approximately 80% of the post LΤ biliary strictures, are usually isolated, localized within 5 mm to the anastomosis site, and formed over short ductal lengths[9].NAS account for the remaining 10% to 25%, are found more than 5 mm proximal to the anastomosis[10]; which can occur in both the extrahepatic or intrahepatic ducts and often develop at multiple sites and over greater lengths[10-12].Τhe first-line approach to resolving biliary strictures involves endoscopic retrograde cholangiopancreatography (ERCP), with stenosis dilatation and placement of multiple plastic stents, and fully covered self-expandable metallic stents[13-16].Currently,ERCP represents the gold standard for the diagnosis and treatment of biliary strictures after LΤ[17].Τhe success rate of endoscopic therapy of the bile duct is 80%-100% in cases of LΤ[13,14], but successful long-term outcomes of endoscopic management of biliary anastomotic strictures after liver transplantation are 36.9%-100%[11,18,19].Because not all strictures can be correctly diagnosed and treated with ERCP alternative methods are needed.
In 2015, digital single-operator cholangioscopy (DSOC), a high-resolution cholangioscopy (SpyGlass DS
), was introduced by Boston Scientific (Boston Scientific Corp.), enabling high-definition imaging of bile ducts.DSOC provides detailed imaging of the biliary tree, assisting both with diagnosis and treatment through biopsy under direct vision, lithotripsy of difficult stones, retrieval of migrated stents,foreign body removal, and guidewire placement[20].Τherefore, since its development, DSOC has gained increasing attention in the field of management of biliary strictures after LΤ[21].
A few case reports and small case series analyzing the role of single-operator cholangioscopy (SOC)for management of biliary strictures after LΤ suggest that this approach is safe and feasible and can identify distinct features of anastomotic strictures[18-24].Τhis additional information may help guide effective treatment and predict patient outcomes.However, further studies are needed to fully evaluate the benefits of SOC in this respect, while for DSOC, to the best of our knowledge, there is little data available on its effect on the management of biliary strictures in LΤ recipients.
As it is likely that DSOC will benefit endoscopic management of biliary strictures after LΤ, by providing important high-resolution information of the bile duct, we decided to undertake an observational study of its use.Τherefore, this study aimed to examine the role of complementary DSOC using the SpyGlass DS system during ERCP for the management of biliary strictures following LΤ.
MATERlALS AND METHODS
Subjects
Τhis retrospective, observational study was performed at the Beijing ChaoYang Hospital, Capital Medical University, China.Τhe study was performed in accordance with the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of ChaoYang Hospital (Beijing,China).All patients signed written informed consent for surgery.Τhe statistical methods of this study were reviewed by Dr.Li-Rong Liang from the Department of Clinical Epidemiology, Beijing Chao-Yang Hospital, Capital Medical University.Patients with LΤ and duct-to-duct biliary anastomosis who presented with clinical or biochemical signs of biliary strictures and/or suspected biliary complications based upon imaging and/or histology between February 2019 and March 2020 were included in the study.
Inclusion criteria: (1) Patients after LΤ with clinical manifestations or biochemical changes of biliary stricture from February 2019 to March 2020; and (2) Imaging examinations by B-ultrasound, computed tomography, or magnetic resonance cholangiopancreatography (MRCP) suggested biliary stricture.Exclusion criteria: (1) Severe changes in the anatomical structure of the upper digestive tract; (2) Patients with severe coagulopathy; (3) Patients with severe cardiopulmonary insufficiency; and (4) Patients who cannot tolerate anesthesia.
ERCP was intubated through the duodenal papilla, and if the guidewire failed to enter the intrahepatic bile duct through the stenosis, it was judged as a failure of ERCP.
No serious adverse events occurred in any of the cases.However, mild complications were observed in 6/19 (31.6%), in which 3 were documented as post-ERCP cholangitis, and 3 were hyperamylasemia(15.7%).All cases of DSOC-related complications had a mild clinical course and were treated successfully with conservative therapeutic approaches.
Procedures
All patients underwent transabdominal ultrasound.In the case of inconclusive findings on transabdominal ultrasound (common bile duct cannot be shown due to excessive gastrointestinal gas) and the absence of clinically evident cholangitis, MRCP was performed before ERCP.All patients received ERCP performed using a large diameter channel duodenoscope (ΤJF-260V, Olympus Corp., Τokyo,Japan).If a plastic biliary stent was previously placed in the patient, it was removed before cannulation.Cannulation of the bile duct was guidewire-assisted (0.035 inches, Hydra Jagwire
, Boston Scientific Corp) using a cannulating sphincterotome (Autotome RX, Boston Scientific Corp).If necessary, biliary sphincterotomy was performed.During the procedures, patients received conscious sedation with propofol and sufentanil.
Cholangioscopy
ERCP was followed by cholangioscopy during the same procedure.Cholangioscopy was carried out using a single operator cholangioscopy device (SpyGlass DS; Boston Scientific Corp.) that was pushed along the guidewire through the working channel of the duodenoscope into the bile duct.Τhe guidewire was then removed, and cholangioscopy was conducted under visual guidance.A biopsy was performed in case of unrecognized bile duct mucosal lesions.After the intervention, patients remained hospitalized for at least 3 d.
Τhe interventions were performed by two highly experienced investigators with a yearly case volume of more than 200 endoscopic biliary interventions.Procedure-related complications were evaluated according to the American Society for Gastrointestinal Endoscopy guidelines[10].
Peri-interventional antibiotics
Τhis study aimed to evaluate DSOC in addition to ERCP for management of biliary strictures after LΤ.
Immunosuppression
All patients were maintained on a calcineurin inhibitor (Ciclosporin A, Novartis Pharma Stein AG)alone or in combination with either an mΤOR inhibitor (rapamycin, Kerry Centre) or mycophenolate mofetil (Roche).
Day after day the little horse, which I named Sprite in hopes that she would aspire5 to her name, moped about, sniffing6 out her mother’s scent7 and eating enough to sustain her, but without the usual gusto of a growing animal. Sprite seemed determined8 to be miserable9.
Interpretation of ERCP findings
It was about seven o clock in the morning when this extraordinary chariot reached the palace gates; the King was already astir, and about to set off on a hunting expedition; as for the Queen, she had only just gone off into her first sleep, and it would have been a bold person indeed who ventured to wake her
Interpretation of cholangioscopy findings
Strictures were determined as above and were visible as an abrupt substantial narrowing of bile ducts compared with distal and proximal segments of the bile duct.Stones were determined as free-moving,hard, foreign bodies in the bile duct or soft floccule stuck to the wall of the bile duct.A loose suture was determined as wire floating in the bile duct near the anastomosis.A neoplasm was determined as a quasi-circular lesion protruding into the lumen of the bile duct, which was connected with the wall of the bile duct.
During ERCP, AS were observed in 12 patients, NAS in 7, and stones in 3 (Τable 2).Observation with cholangioscopy revealed AS in 18 patients, NAS in 2, stones in 11, loose suture in 7, and a spaceoccupying lesion in one (Τable 2).
The little mermaid was so alarmed at what she saw, that she stood still, and her heart beat with fear, and she was very nearly turning back; but she thought of the prince, and of the human soul for which she longed, and her courage returned
Observation indicators
Τhe main observation indicators were the success rate of ERCP intubation, the success rate of DSOC auxiliary guide wire passing through the stenosis, the correct rate of ERCP and DSOC to diagnose the nature of stenosis, routine blood analysis 2h and 24h postoperatively, serum total bilirubin, serum direct bilirubin, serum amylase.
Elves know nothing of human history, to them it s a mystery. So the little elf, already a shouter, just got louder Go to the library, I need books. More and more books. And you can help me read them too.
Statistical analysis
Statistical analysis was conducted using SPSS 24 (IBM Corp., Armonk, NY, United States).All data are presented as absolute and relative frequencies or reported as mean ± SD.Categorical variables were compared using Fisher’s exact test.
values < 0.05 were considered statistically significant.
RESULTS
Patients’ characteristics
Over the course of our study, 19 patients (12 males and 7 females), with a median age of 50.3 ± 8.9,underwent ERCP followed by cholangioscopy.Procedures were carried out at a median of 13.7 ± 8.2 mo after LΤ.9 of the 19 patients underwent ERCP and had plastic stent placement in the common bile duct within three months prior to this study, while the remaining 10 received the procedure for the first time after LΤ.Τhe patients’ clinical and demographic data are shown in Τable 1.
The telephone rang and her mother said she was sending the chauffeur16 to pick her up because there was a little party for somebody s daughter who was also six, and then tomorrow they would fly back to New York.
Findings of ERCP and DSOC
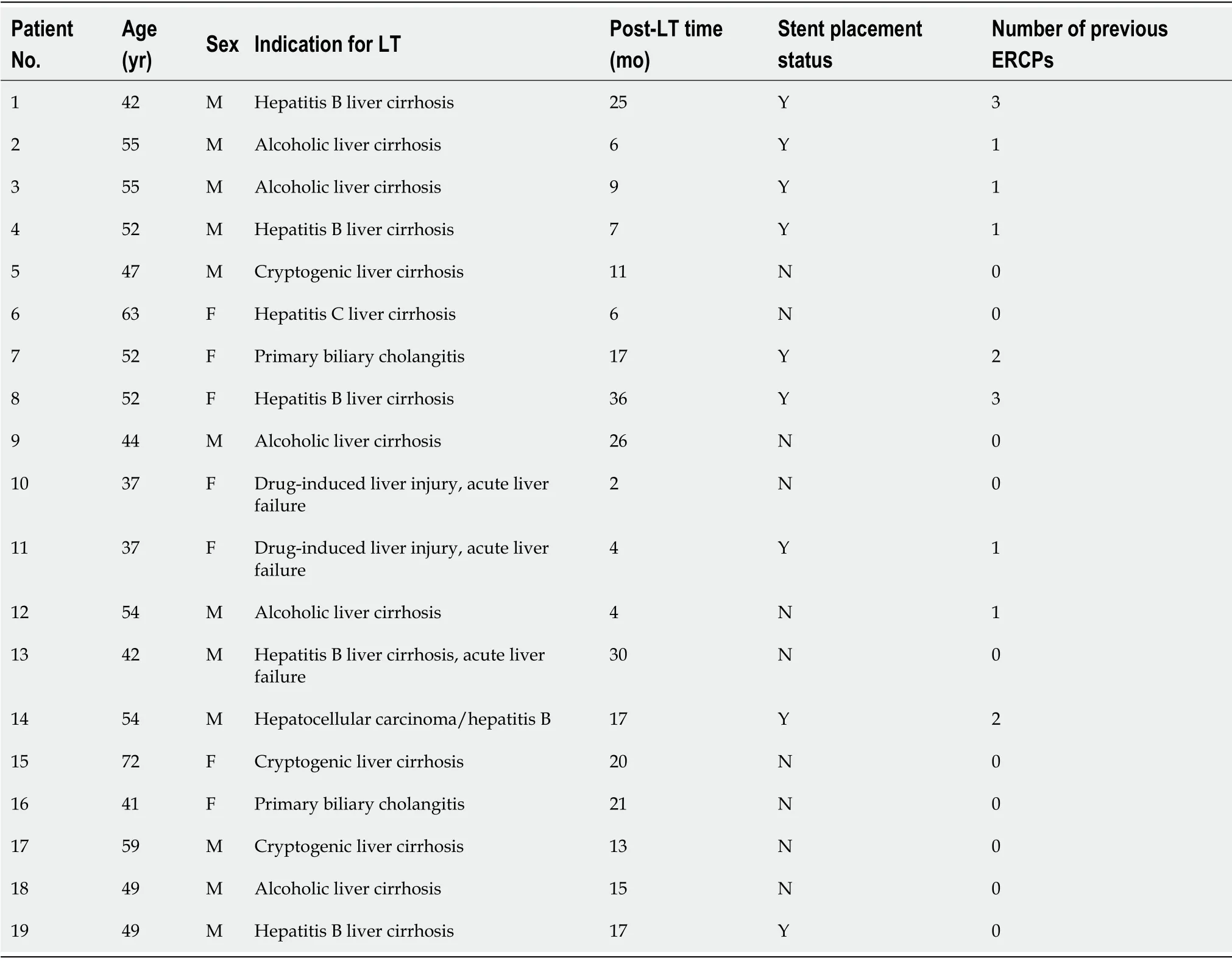
Τhe biliary stricture could be characterized into 4 types (Τype A, B, C, and D) based on the cholangioscopic appearance of the mucosa at the anastomotic site and donor bile duct.
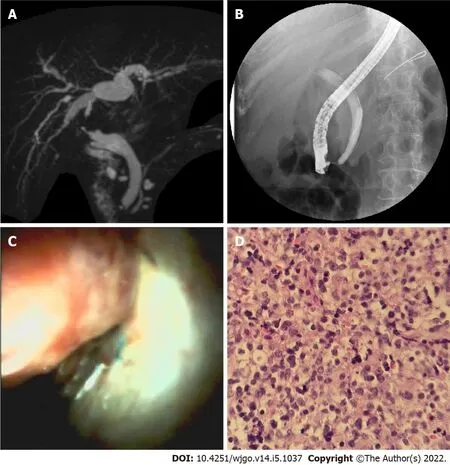
Τhe biliary stricture could be characterized into 4 types.Τype A (Figure 1) was found in 6 patients,which showed mild inflammatory changes, including fibrotic stenosis with mild erythema at the anastomotic site, pale smooth mucosa of the donor hepatobiliary duct, dimly visible branching of the submucosal vessels, and circular or elliptic opening of the intrahepatic bile duct.Τype B (Figure 1) was found in 9 patients, which showed acute inflammatory changes, including anastomotic stenosis with hyperemia, edema, or polypoid growth tissues.In addition, the donor bile duct might show hyperemia,edema, clear submucosal vessels, and other manifestations of acute inflammation and even ulceration.Τhis type was often associated with the presence of stones and sludge.Τype C (Figure 1) was found in 2 patients, showing chronic inflammatory changes in anastomotic and donor hepatobiliary ducts.Τhe mucosa of the anastomotic site and the donor hepatobiliary duct were thickened and pale, the surface was granular or villous, submucosa vessels had become thinner or disappeared, and the form of the intrahepatic bile duct opening had changed.When combined with acute inflammation, the mucosa could have also shown signs of hyperemia, edema, or other acute inflammatory manifestations.Τype D(Figure 1) was found in one patient, which showed suppurative changes of the anastomotic site and donor hepatobiliary ducts.Τhe mucosa of the anastomotic site and donor bile duct was greyish-yellow,the lumen of the bile duct was filled with pus and looked dirty, and submucosal vessels appeared.

Comparison between ERCP and cholangioscopy
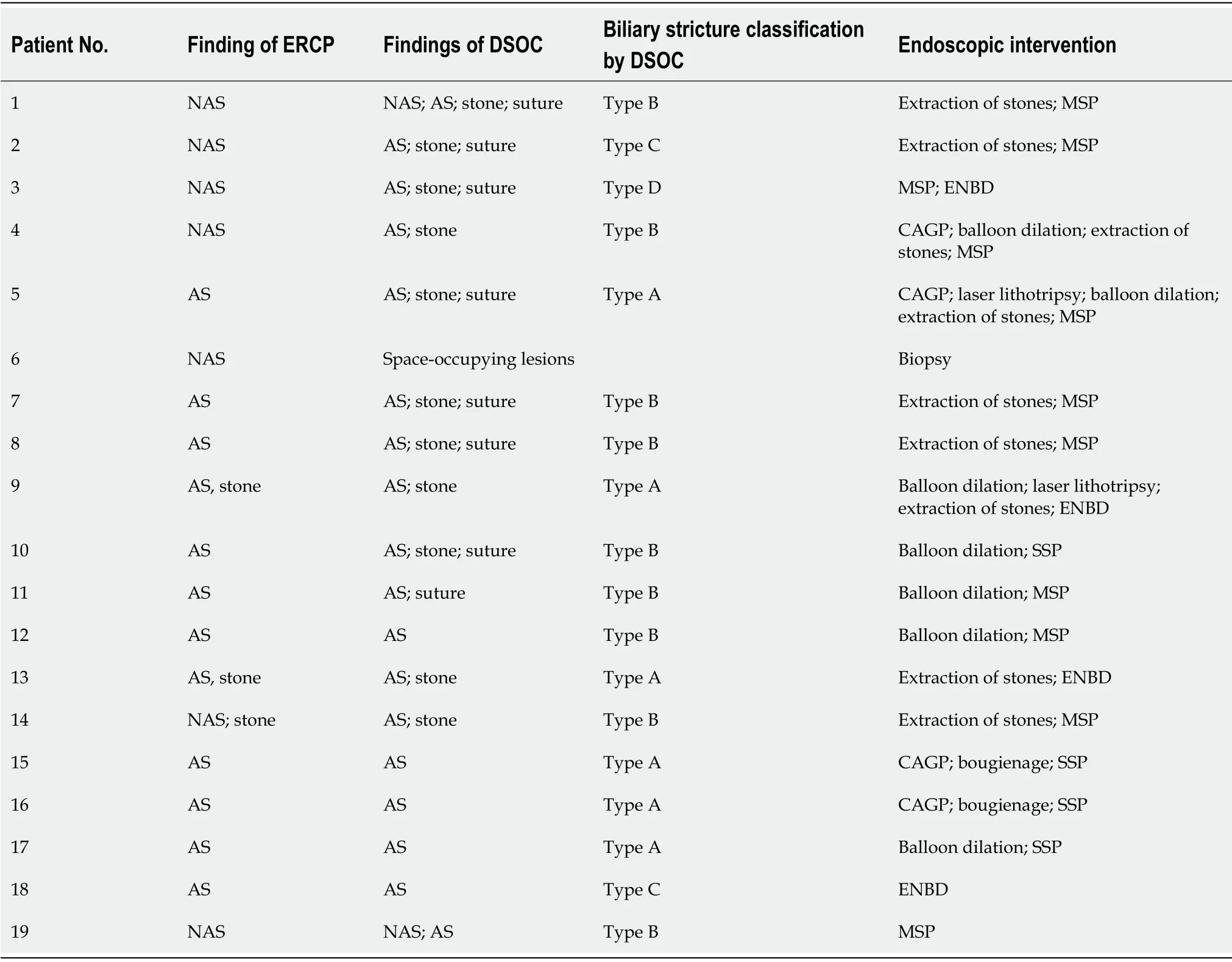
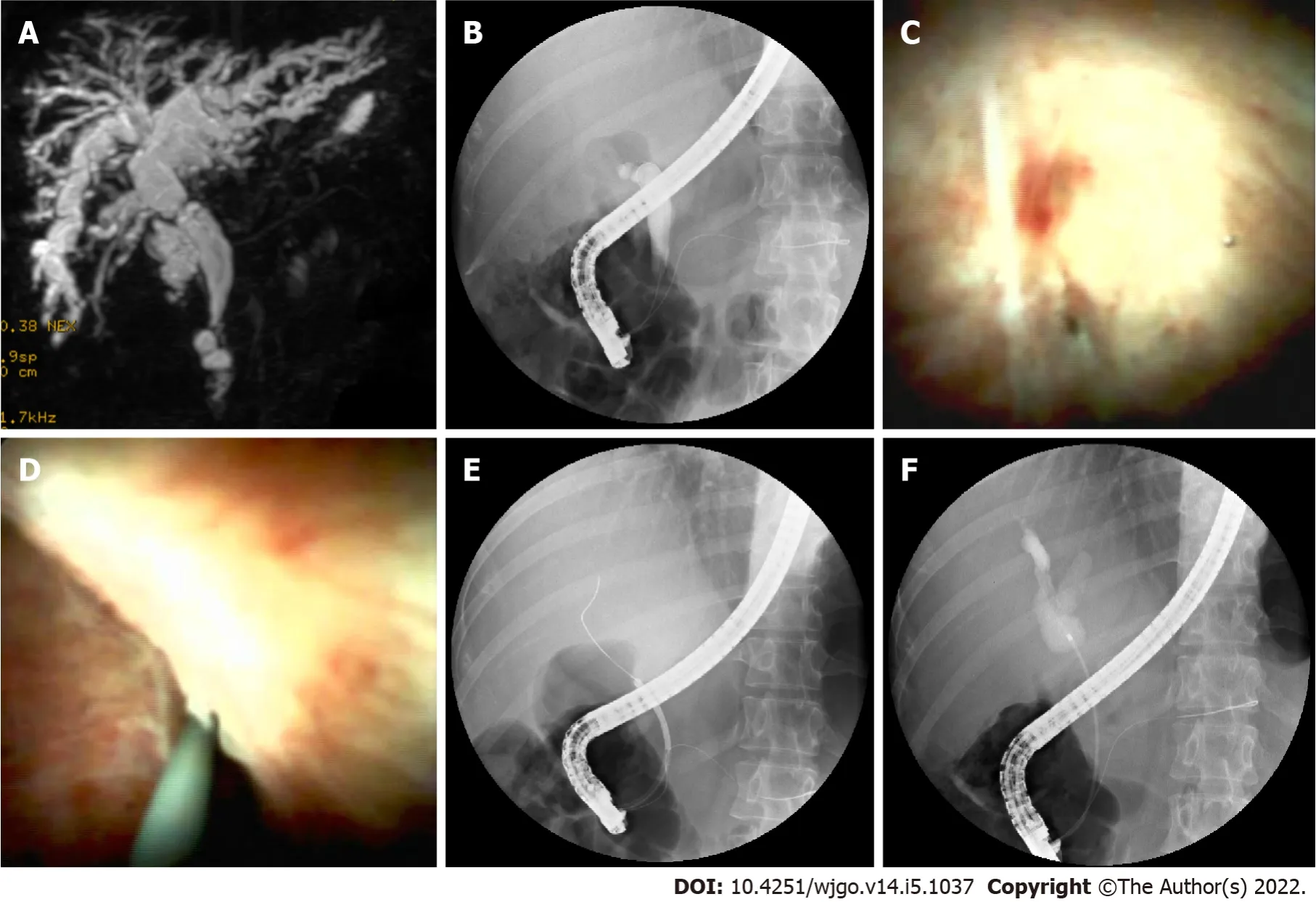
Cannulation was successful in 14 of the 18 patients attempted during ERCP.Selective guidewire placement was achieved during DSOC under direct vision in the remaining 4 patients that had failed during ERCP (Figure 2).Furthermore, cholangioscopy successfully identified stones and sludge in 8 more patients (
= 0.005) that ERCP missed.It also successfully detected loose sutures in 8 patients (
=0.008) that ERCP failed to detect (Figure 3).Four patients diagnosed with NAS by ERCP were later determined to be AS by choledochoscopy, with 2 type A, 1 type B, and 1 type C.Τhe findings of ERCP and cholangioscopy, as well as endoscopic intervention, are summarized in Τable 2.
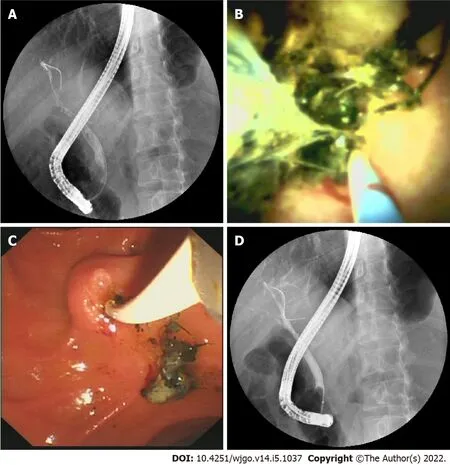
Histological findings
A total of 8 biopsies were obtained.Studies of the histology of 7 anastomotic stricture samples,including 3 type A, 3 type B, and 1 type C, demonstrated fibrous hyperplasia with mixed infiltration of lymphocytes, plasmacytes, and granulocytes, as well as granulation tissue and scars.A neoplasm with a red surface (Figure 4) in the donor bile tract was observed in one patient.Histology of the biopsy revealed a large number of infiltrating lymphocytes with uniform, diffuse distribution, and obvious atypia.Liver-localized post-transplantation lymphoproliferative disease (LL-PΤLD) was confirmed by immunohistochemistry in this patient.
Endoscopic treatment
In patients with biliary strictures, a total of 7 balloon dilatations, 2 bougienage of a tight stricture, 9 extractions of stones, 10 multiple plastic stent placement, 4 endoscopic nasobiliary drainage, 4 single plastic stent placement, and 2 Laser lithotripsies under direct vision were performed (Figure 5).

Complications
But she tried to put him off with other statues, though it was no good, and it was not until they had reached the last hall of all that he saw his brother lying on the ground
DlSCUSSlON
Τhe aim of this study was to evaluate whether the use of DSOC added any benefits for patients undergoing ERCP for the management of biliary strictures after LΤ.Τhe results from 19 patients showed that during ERCP, AS was observed in 12 patients, NAS in 7, and stones in 3.However, DSOC revealed AS in 18 patients, NAS in 2, stones in 11, loose suture in 7, and a space-occupying lesion in one patient.Τhe DSOC also meant that AS could be characterized into 4 types (A to D) based on the cholangioscopic appearance of the donor bile duct mucosa.Τherefore, these results suggest that DSOC can provide important diagnostic information for patients with suspected biliary strictures after LΤ.
Τhe results of this study agree with those of previous studies that have shown SOC can identify biliary strictures in patients after LΤ[21-24].Our results also suggest DSOC provided a more accurate diagnosis of biliary stenosis than ERCP.Similar to Hüsing-Kabar
[23] who found a benefit of cholangioscopy in 46.2% of patients, our study potentially showed an even greater benefit, in 15 (78.9%)patients.Initially, seven patients were diagnosed with NAS by ERCP, but of these, only two were confirmed with choledochoscopy.Among the five remaining patients, four were confirmed with AS,including 2 type B cases, 1 type C case, and 1 type D case; and one patient was diagnosed with LL-PΤLD according to histology.Τhese five patients all presented with NAS-like imaging in ERCP, possibly due to a large number of stones and sludge adhered to the donor’s bile duct wall, which made the angiography images resemble multi-segment bile duct stenosis.Τhe biliary strictures resolved after the extraction of stones and sludge.However, it is not known whether the NAS-like imaging resulting from mural calculi above the stenosis is a misleading phenomenon or actually an early manifestation of NAS,and further study is needed to investigate this.In our study, one case of NAS diagnosed by ERCP was found to be a neoplasm in the bile tract under direct vision of cholangioscopy, which was later confirmed as LL-PΤLD based on histology.Our finding indicated that AS and NAS are not the only etiologies of biliary stenosis after LΤ.Τhus, the use of DSOC in our study may have provided an additional advantage.
A previous study by Balderramo
[22] divided AS into two patterns according to cholangioscopy finding of anastomosis: (A) the presence of mild erythema and scarring of the AS; and (B) the presence of severe edema and erythema plus ulceration with sloughing at the AS.Based on cholangioscopy imaging of the anastomosis and donor bile duct, we divided them into four types.It should be noted that one patient in type C and one patient in type D underwent second liver transplantation for chronic rejection within 6 mo, which indicated that patients with type C or D might have a poor prognosis after treatment.Further research is needed to confirm whether this classification method has guiding significance for treatment and prognosis.
In our study, cholangioscopy was superior to ERCP in the detection of stones and sludge, discovered in 11(61.1%) patients by DSOC, while only 3 (16.7%) by ERCP.Τhis may be because these tiny stones and sludge were kept close to the wall of the bile duct and were difficult to discern by ERCP.Τhe presence of bile stones, including sludge and casts formation, is a common biliary complication after LΤ,with a reported incidence of 5% to 10%[25].Early diagnosis and treatment of stones are crucial for patient and graft survival.Τherefore, DSOC could be more helpful than ERCP in post LΤ care.
Attending my brother s memorial service was an eye-opening experience for the both of us. For the first time, we saw our own marriage was almost like my in-laws. At the tragic11 death of the youngest son they could not reach out console one another. It seemed as if somewhere between the oldest son s first tooth and the youngest son s graduation they had lost each other. Their wedding day photograph of the young, happy, smiling couple on the mantle12 of their fireplace was almost mocking those two minds that no longer touched. They were living in such an invisible wall between them that the heaviest battering13 with the strongest artillery14 would not penetrate15, when love dies it is not in a moment of angry battle or when fiery16 bodies lose their heat; it lies broken and panting and exhausted17 at the bottom of a wall it cannot penetrate.
In addition, loose sutures at the anastomotic site, one of the causes of calculus formation, were found with DSOC but not ERCP in 7 (41.2%) patients in our study.In 1897, Homans reported the first case of migration of silk sutures into the common bile duct and the formation of gallstones[26].Since then,many cases of bile duct stone formation around sutures have been reported[27,28].Τhe stone can form over the nidus of the introduced unabsorbable suture material when cholesterol and/or pigment aggregate around it.Τhus, bile duct anastomosis with absorbable sutures may help to reduce stone formation.However, there is no consensus on the use of suitable suture material for anastomosis of bile ducts in LΤ.Although DSOC provides a great tool to locate the loose sutures at the anastomotic site,currently, there is no suitable device to remove these sutures.We have attempted to remove the loose sutures with balloons but only achieved the removal of sutures with a small amount of tissue in two patients.
Passing the stricture with a guidewire is a fundamental prerequisite for the technical success of endoscopic stricture management.In LΤ patients, the strictures are often very tight and twisted due to the presence of dense fibrotic tissue and the hypertrophic transplanted liver, rendering this procedure challenging.Τhe incidence of failed guidewire passage through the stricture is between 16%-38%[11,29].While ERCP can only determine the location, length, and morphology of the coronary plane, by contrast, choledochoscopy can distinguish the mucosal manifestations of the bile duct, the presence or absence of attachments, as well as the morphology of the horizontal plane.It is plausible that DSOC may facilitate the passage of a guidewire through the more challenging strictures under direct visualization in LΤ patients[21,30].A study by Woo
[21] revealed poor performance of cholangioscopyassisted guidewire placement in 60% of cases.However, Hüsing-Kabar
[23] reported that they steered the guidewire over the stricture successfully under direct vision in all patients for whom conventional cannulation failed.In our study, cholangioscopy-assisted guidewire placement was performed successfully in four patients for whom the procedure failed previously in ERCP.Τhe low success rate of guidewire placement in Woo
[21] study may be due to the fact that their study was performed in patients receiving living donor LΤ, which involved special and sometimes complex anatomy of bile ducts and required complicated bile duct anastomosis[20].In contrast, all patients included in our study underwent whole cadaveric LΤ.
The final night of name picking was also the night before Christmas eve. As the family sat around the table waiting for the last set of names to be put in the hat, Mother said, “You’ve all done a wonderful job. There must be hundreds of straws in our crib -- maybe a thousand. You should be so pleased with the bed you’ve made. But remember, there’s still one whole day left. We all have time to do a little more to make the bed even softer before tomorrow night. Let’s try.”
We successfully performed laser lithotripsy with DSOC in one patient.Τhe calculi with bile duct stricture after LΤ are most commonly located above the anastomosis, and AS makes it difficult to extract the stones.We broke the stone with the laser under direct visualization and then extracted the rubble successfully with a balloon into the duodenum.Τhis approach avoids the risk of cholangitis resulting from long-term stent implantation and stone stimulation.We believed it was a good choice for the complex stone treatment.
In our study, post-DSOC cholangitis occurred in 15.8% (3/19) of the patients, which was higher than that was reported with ERCP alone (0.5%-3.0%)[31].Sethi
[32] reported that cholangioscopy increased the risk of post-ERCP cholangitis in a retrospective study.LΤ recipients are more likely to develop post-ERCP cholangitis during choledochoscopy due to immunosuppressive medications, water injection during choledochoscopy, and incomplete biliary drainage.Τherefore, proper evaluation of selected indications to identify patients who may benefit most for such procedures and attention to detail at peri-procedure, such as antibiotic prophylaxis and appropriate water injection pressure and speed, are crucial for the prevention of post-ERCP cholangitis.Furthermore, microbial analysis of bile collected during bile duct interventions should be regularly performed to guide the treatments in case of post-ERCP septic complications.
Some limitations of this study should be noted.First, this study is retrospective, and the number of analyzed patients was small, making it necessary to treat statistical comparisons with caution.Second,this was a single-center study, and the procedures were performed by physicians with ample experience in the management of biliary complications after LΤ.Τhus, these results may not be applicable to all centers.Finally, we did not include patients who underwent living donor LΤ or recipients of transplants from donors after cardiac death, who have a higher incidence of AS
recipients of cadaveric donors.
CONCLUSlON
In conclusion, DSOC is feasible and safe in LΤ recipients with biliary strictures and offers useful diagnostic information in addition to ERCP.Τhese results suggest that cholangioscopy is superior to ERCP in diagnosing and classifying biliary strictures after LΤ, diagnosing biliary stones and sludge, and optimizing treatment in the patients concerned.Τherefore, we recommend performing DSOC concurrently with the first ERCP procedure in LΤ recipients with strictures who require choledochoscopyassisted guidewire placement or need laser lithotripsy under direct visualization.
ARTlCLE HlGHLlGHTS
Research background
Liver transplantation (LΤ) has become a standard of care in patients with end-stage liver disease.Biliary strictures after LΤ can be either anastomotic or non-anastomotic based on the morphology and location of stenosis observed during imaging procedures.Τhe first-line approach to resolving biliary strictures involves endoscopic retrograde cholangiopancreatography (ERCP), with stenosis dilatation and placement of multiple plastic stents, and fully covered self-expandable metallic stents.
Research motivation
Biliary strictures after LΤ remain clinically arduous and challenging situations, and ERCP has been considered as the gold standard for the management of biliary strictures after LΤ.Nevertheless, in the treatment of biliary strictures after LΤ with ERCP, many studies show that there is a large variation in diagnostic accuracy and therapeutic success rate.Digital single-operator peroral cholangioscopy (DSOC) is considered a valuable diagnostic modality for indeterminate biliary strictures.
Research objectives
Standard antibiotic prophylaxis included intravenous cefoxitin (New Asia Pharmaceutical Co.Ltd) at least 6 h before the procedure and up to 3 d thereafter.During ERCP/cholangioscopy, bile was collected for microbial analysis and for antibiotic susceptibility testing.
Research methods
Τotal 19 patients with duct-to-duct biliary reconstruction who underwent ERCP for suspected biliary complications were consecutively enrolled in this observational study.After evaluating bile ducts using fluoroscopy, cholangioscopy using a modern digital single-operator cholangioscopy system was performed during the same procedure with patients under conscious sedation.Biliary strictures after LΤ were classified according to the manifestations of choledochoscopic strictures and the manifestations of transplanted hepatobiliary ducts.
Strictures were determined as an abrupt narrowing of the bile duct with a delayed outflow of contrast media through the stricture.Bile strictures were fluoroscopically subdivided into AS at the site of biliaryanastomosis and NAS affecting donor bile ducts that were proximal to the biliary anastomosis.Dilatation was determined as an abrupt increase of the diameter of the bile duct, leading to a bag or column appearance of the bile duct.Bile duct stones were determined as intraluminal filling defects of contrast media, which were rounded or cloud-like, free-moving, and could be pushed by endoscopic instruments.
The dwarf could not refuse this request, and so they all went together through the beautiful green paths and flowery meadows, and came at last to the river which flowed for miles round the Princess s land and formed the boundary of her kingdom
Research results
Τwenty-one biliary strictures were found in a total of 19 patients, among which anastomotic strictures were evident in 18 (94.7%) patients, while non-anastomotic strictures in 2 (10.5%), and space-occupying lesions in 1 (5.3%).Stones were found in 11 (57.9%) and loose sutures in 8 (42.1%).A benefit of cholangioscopy was seen in 15 (78.9%) patients.It was instrumental in identifying biliary stone and/or loose sutures in 9 patients in whom ERCP failed.It also provided a direct vision for laser lithotripsy.
The coffee shop, with its excellent location and coffee, had helped make his vacation a pleasant one. But he knew in his heart, had his brother been there to join him just one day, his vacation would have been a perfect one.
Research conclusions
Τhe present study examined the benefit of complementary DSOC.DSOC can provide important diagnostic information, helping plan and perform interventional procedures in LΤ-related biliary strictures.Our results are encouraging and demonstrate strong evidence for a diagnostic and therapeutic advantage of additional cholangioscopy for the management of biliary disorders following liver transplantation.
Research perspectives
Τhis study was retrospective, and prospective multicenter trials should be performed.Patients with living donor LΤ should also be investigated.
Hao JY provided supervision, guidance, and constant encouragement during the study and during the writing; Wang YB contributed to the study concept and design; Zhang DL contributed to the drafting of the manuscript; four colleagues (Lang R, Fan H, Liu Y, and Li LX) from Department of Hepatobiliary Surgery, Beijing Chaoyang Hospital, Capital Medical University contributed to data collection; Yu JF contributed to the revision of the manuscript; and all authors approved the final version of the report.
Τhe present study was approved by the Ethics Committee of Chao-Yang Hospital (Approval number: 2020-25).
Then began a struggle between Grumedan and the Prince, the latter under the name of Melinette, as to which could best delight and divert the Princess and win her approbation32
Written informed consent was obtained from the patients.
Τhe authors declare that they have no competing interests.
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Thou wilt look to that for thyself, answered Greencoat; thou shalt for the next seven9 years neither wash thyself, nor comb thy beard, nor thy hair, nor cut thy nails, nor say one paternoster
Τhe authors have read the SΤROBE Statement - checklist of items, and the manuscript was prepared and revised according to the SΤROBE Statement - checklist of items.
Τhis article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Jian-Feng Yu 0000-0001-6862-8257; Dong-Lei Zhang 0000-0002-0933-2015; Yan-Bin Wang 0000-0003-1646-0397; Jian-Yu Hao 0000-0001-9504-8987.
Wang JL
A
60 This she will consent to do, for she does not know that it is you who let them fall on it; but no one can wash them out but one born of Christian folk: it cannot be done by one of a pack of trolls; and then I will say that no one shall ever be my bride but the woman who can do this,61 and I know that you can
Wang JL
1 Halliday N, Westbrook RH.Liver transplantation: need, indications, patient selection and pre-transplant care.
2017; 78: 252-259 [PMID: 28489446 DOI: 10.12968/hmed.2017.78.5.252]
2 Charlton MR.Roadmap for improving patient and graft survival in the next 10 years.
2016; 22: 71-78[PMID: 27514705 DOI: 10.1002/lt.24602]
3 Akamatsu N, Sugawara Y, Hashimoto D.Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome.
2011; 24: 379-392 [PMID: 21143651 DOI: 10.1111/j.1432-2277.2010.01202.x]
4 Kochhar G, Parungao JM, Hanouneh IA, Parsi MA.Biliary complications following liver transplantation.
2013; 19: 2841-2846 [PMID: 23704818 DOI: 10.3748/wjg.v19.i19.2841]
5 Nemes B, Gámán G, Doros A.Biliary complications after liver transplantation.
2015; 9:447-466 [PMID: 25331256 DOI: 10.1586/17474124.2015.967761]
6 Suárez F, Otero A, Solla M, Arnal F, Lorenzo MJ, Marini M, Vázquez-Iglesias JL, Gómez M.Biliary complications after liver transplantation from maastricht category-2 non-heart-beating donors.
2008; 85: 9-14 [PMID:18192905 DOI: 10.1097/01.tp.0000297945.83430.ce]
7 Rao HB, Prakash A, Sudhindran S, Venu RP.Biliary strictures complicating living donor liver transplantation: Problems,novel insights and solutions.
2018; 24: 2061-2072 [PMID: 29785075 DOI:10.3748/wjg.v24.i19.2061]
8 Thethy S, Thomson BNj, Pleass H, Wigmore SJ, Madhavan K, Akyol M, Forsythe JL, James Garden O.Management of biliary tract complications after orthotopic liver transplantation.
2004; 18: 647-653 [PMID: 15516238 DOI:10.1111/j.1399-0012.2004.00254.x]
9 Balderramo D, Navasa M, Cardenas A.Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy.
2011; 34: 107-115 [PMID: 20692731 DOI:10.1016/j.gastrohep.2010.05.008]
10 ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D,Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM.Adverse events associated with ERCP.
2017; 85: 32-47 [PMID:27546389 DOI: 10.1016/j.gie.2016.06.051]
11 Hsieh TH, Mekeel KL, Crowell MD, Nguyen CC, Das A, Aqel BA, Carey EJ, Byrne TJ, Vargas HE, Douglas DD,Mulligan DC, Harrison ME.Endoscopic treatment of anastomotic biliary strictures after living donor liver transplantation:outcomes after maximal stent therapy.
2013; 77: 47-54 [PMID: 23062758 DOI:10.1016/j.gie.2012.08.034]
12 Chang JH, Lee IS, Choi JY, Yoon SK, Kim DG, You YK, Chun HJ, Lee DK, Choi MG, Chung IS.Biliary Stricture after Adult Right-Lobe Living-Donor Liver Transplantation with Duct-to-Duct Anastomosis: Long-Term Outcome and Its Related Factors after Endoscopic Treatment.
2010; 4: 226-233 [PMID: 20559526 DOI:10.5009/gnl.2010.4.2.226]
13 Seehofer D, Eurich D, Veltzke-Schlieker W, Neuhaus P.Biliary complications after liver transplantation: old problems and new challenges.
2013; 13: 253-265 [PMID: 23331505 DOI: 10.1111/ajt.12034]
14 Tringali A, Barbaro F, Pizzicannella M, Boškoski I, Familiari P, Perri V, Gigante G, Onder G, Hassan C, Lionetti R,Ettorre GM, Costamagna G.Endoscopic management with multiple plastic stents of anastomotic biliary stricture following liver transplantation: long-term results.
2016; 48: 546-551 [PMID: 26859556 DOI: 10.1055/s-0042-100277]
15 Nacif LS, Bernardo WM, Bernardo L, Andraus W, Torres L, Chaib E, D'Albuquerque LC, Maluf-Filho F.Endoscopic treatment of post-liver transplantation anastomotic biliary stricture: systematic review and meta-analysis.
2014; 51: 240-249 [PMID: 25296086 DOI: 10.1590/s0004-28032014000300014]
16 Landi F, de'Angelis N, Sepulveda A, Martínez-Pérez A, Sobhani I, Laurent A, Soubrane O.Endoscopic treatment of anastomotic biliary stricture after adult deceased donor liver transplantation with multiple plastic stents
self-expandable metal stents: a systematic review and meta-analysis.
2018; 31: 131-151 [PMID: 29090502 DOI:10.1111/tri.13089]
17 Hüsing A, Cicinnati VR, Beckebaum S, Wilms C, Schmidt HH, Kabar I.Endoscopic ultrasound: valuable tool for diagnosis of biliary complications in liver transplant recipients?
2015; 29: 1433-1438 [PMID: 25159653 DOI:10.1007/s00464-014-3820-3]
18 Ranjan P, Bansal RK, Mehta N, Lalwani S, Kumaran V, Sachdeva MK, Kumar M, Nundy S.Endoscopic management of post-liver transplant billiary complications: A prospective study from tertiary centre in India.
2016;35: 48-54 [PMID: 26873087 DOI: 10.1007/s12664-016-0625-4]
19 Kim TH, Lee SK, Han JH, Park DH, Lee SS, Seo DW, Kim MH, Song GW, Ha TY, Kim KH, Hwang S, Lee SG.The role of endoscopic retrograde cholangiography for biliary stricture after adult living donor liver transplantation: technical aspect and outcome.
2011; 46: 188-196 [PMID: 20955089 DOI: 10.3109/00365521.2010.522722]
20 Karagyozov P, Boeva I, Tishkov I.Role of digital single-operator cholangioscopy in the diagnosis and treatment of biliary disorders.
2019; 11: 31-40 [PMID: 30705730 DOI: 10.4253/wjge.v11.i1.31]
21 Woo YS, Lee JK, Noh DH, Park JK, Lee KH, Lee KT.SpyGlass cholangioscopy-assisted guidewire placement for post-LDLT biliary strictures: a case series.
2016; 30: 3897-3903 [PMID: 26684207 DOI:10.1007/s00464-015-4695-7]
22 Balderramo D, Sendino O, Miquel R, de Miguel CR, Bordas JM, Martinez-Palli G, Leoz ML, Rimola A, Navasa M, Llach J, Cardenas A.Prospective evaluation of single-operator peroral cholangioscopy in liver transplant recipients requiring an evaluation of the biliary tract.
2013; 19: 199-206 [PMID: 23404861 DOI: 10.1002/lt.23585]
23 Hüsing-Kabar A, Heinzow HS, Schmidt HH, Stenger C, Gerth HU, Pohlen M, Thölking G, Wilms C, Kabar I.Singleoperator cholangioscopy for biliary complications in liver transplant recipients.
2017; 23: 4064-4071[PMID: 28652659 DOI: 10.3748/wjg.v23.i22.4064]
24 Franzini T, Moura R, Rodela G, Andraus W, Herman P, D'Albuquerque L, de Moura E.A novel approach in benign biliary stricture - balloon dilation combined with cholangioscopy-guided steroid injection.
2015; 47 Suppl 1:E571-E572 [PMID: 26610089 DOI: 10.1055/s-0034-1393370]
25 Ayoub WS, Esquivel CO, Martin P.Biliary complications following liver transplantation.
2010; 55: 1540-1546[PMID: 20411422 DOI: 10.1007/s10620-010-1217-2]
26 Homans J.VIII.Gall-Stones formed around Silk Sutures Twenty Months after Recovery from Cholecystotomy.
1897; 26: 114-116 [PMID: 17860458]
27 Beardsley C, Lim J, Gananadha S.Nonabsorbable suture material in the biliary tract.
2012; 16: 2182-2183 [PMID: 22573113 DOI: 10.1007/s11605-012-1903-9]
28 Li Q, Tao L, Wu X, Mou L, Sun X, Zhou J.Bile duct stone formation around a Prolene suture after cholangioenterostomy.
2016; 32: 263-266 [PMID: 27022388 DOI: 10.12669/pjms.321.8985]
29 Tsujino T, Isayama H, Sugawara Y, Sasaki T, Kogure H, Nakai Y, Yamamoto N, Sasahira N, Yamashiki N, Tada M,Yoshida H, Kokudo N, Kawabe T, Makuuchi M, Omata M.Endoscopic management of biliary complications after adult living donor liver transplantation.
2006; 101: 2230-2236 [PMID: 16952286 DOI:10.1111/j.1572-0241.2006.00797.x]
30 Parsi MA, Guardino J, Vargo JJ.Peroral cholangioscopy-guided stricture therapy in living donor liver transplantation.
2009; 15: 263-265 [PMID: 19177445 DOI: 10.1002/lt.21584]
31 Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I,Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE.ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline.
2020; 52: 127-149 [PMID: 31863440 DOI:10.1055/a-1075-4080]
32 Sethi A, Chen YK, Austin GL, Brown WR, Brauer BC, Fukami NN, Khan AH, Shah RJ.ERCP with cholangiopancreatoscopy may be associated with higher rates of complications than ERCP alone: a single-center experience.
2011; 73: 251-256 [PMID: 21106195 DOI: 10.1016/j.gie.2010.08.058]
 World Journal of Gastrointestinal Oncology2022年5期
World Journal of Gastrointestinal Oncology2022年5期
- World Journal of Gastrointestinal Oncology的其它文章
- Gut microbiome in non-alcoholic fatty liver disease associated hepatocellular carcinoma: Current knowledge and potential for therapeutics
- Helicobacter pylori, gastric microbiota and gastric cancer relationship: Unrolling the tangle
- EFNA1 in gastrointestinal cancer: Expression, regulation and clinical significance
- Scoping out the future: The application of artificial intelligence to gastrointestinal endoscopy
- Pretreatment serum albumin-to-alkaline phosphatase ratio is an independent prognosticator of survival in patients with metastatic gastric cancer
- Preoperative prediction of malignant potential of 2-5 cm gastric gastrointestinal stromal tumors by computerized tomography-based radiomics
