以腰腿痛为主要表现的PHPT病人8例临床分析
曹振鲁 殷楚强 王志超 刘宸境 张修塨 王亭

[摘要]目的探讨以腰腿痛首诊的原发性甲状旁腺功能亢进症(PHPT)病人的临床特征,提高临床医生对该病认识,减少其误诊误治。方法分析以腰腿痛就诊的8例PHPT病人的临床表现及诊疗过程。结果8例病人主要症状为腰背部或下肢疼痛;4例病人表现为腰痛伴肢体乏力,3例病人表现为腰痛伴下肢疼痛,1例病人表现为腰背部疼痛合并下肢疼痛。初诊误诊为原发性骨质疏松椎体压缩性骨折3例,腰椎间盘突出症3例,腰椎椎管狭窄症2例。结论PHPT可以腰腿痛为首发表现就诊于脊柱外科,诊断椎体骨折、腰椎间盘突出症、腰椎椎管狭窄症应警惕PHPT的存在。
[关键词]甲状旁腺功能亢进,原发性;腰腿痛;诊断,鉴别;误诊
[中图分类号]R582.1[文献标志码]B[文章编号]2096-5532(2022)02-0302-04
doi:10.11712/jms.2096-5532.2022.58.077[开放科学(资源服务)标识码(OSID)]
[网络出版]https://kns.cnki.net/kcms/detail/37.1517.r.20220416.2315.002.html;2022-04-2007:30:59
PRIMARY HYPERPARATHYROIDISM WITH WAIST AND LEG PAIN AS THE MAIN MANIFESTATION: A CLINICAL ANALYSIS OF EIGHT CASES CAO Zhenlu, YIN Chuqiang, WANG Zhichao, LIU Chenjing, ZHANG Xiugong, WANG Ting (Department Spine, The Affiliated Hospital of Qingdao University, Qingdao 266003, China)
[ABSTRACT]ObjectiveTo investigate the clinical features of patients with primary hyperparathyroidism (PHPT) with waist and leg pain at initial diagnosis, to improve the awareness of this disease among clinicians, and to reduce misdiagnosis and mistreatment. MethodsEight patients with PHPT who attended the hospital due to waist and leg pain were analyzed in terms of clinical manifestation and diagnosis. ResultsAll eight patients had the main symptom of pain in lower back or lower limbs, among whom four had waist pain and limb weakness, three had waist pain and pain in lower limbs, and one had lower back pain and pain in lower limbs. As for misdiagnosis at initial diagnosis, three patients were misdiagnosed as primary osteoporotic vertebral compression fractures, three were misdiagnosed as lumbar disc herniation, and two were misdiagnosed as lumbar spinal stenosis. ConclusionPatients with PHPT may attend department of spinal surgery due to the initial manifestation of waist and leg pain, and the presence of PHPT should be considered for the diagnosis of vertebral fracture, lumbar disc herniation, and lumbar spinal stenosis.
[KEY WORDS]hyperparathyroidism, primary; lumbago leg pain; diagnosis, differential; diagnostic errors
原發性甲状旁腺功能亢进症(PHPT)较少见,其临床表现不典型,临床医师对其认识不足,极易误诊漏诊。既往文献报道该病的误诊率高于50%,未及时诊断会给病人造成不必要的痛苦及经济负担,甚至威胁病人生命。2015年1月—2020年1月,青岛大学附属医院诊治8例以腰腿痛为主要表现的PHPT病人,本文对其临床资料报告如下。
1临床资料
1.1一般资料
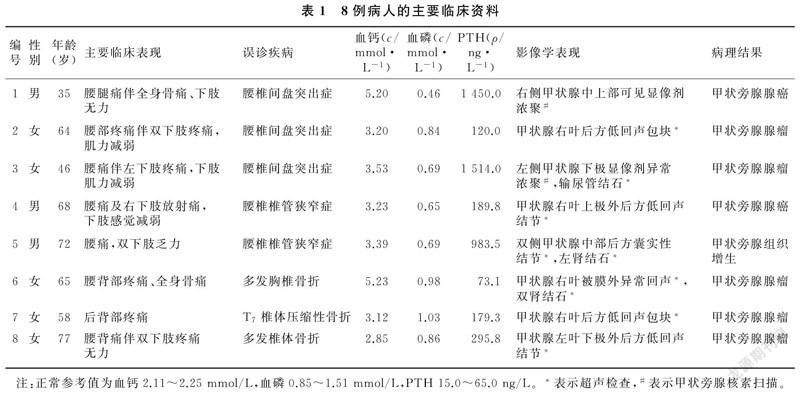
以腰腿痛为主要表现的PHPT病人8例, 男3例,女5例;年龄35~77岁。PHPT诊断参考《原发性甲状旁腺功能亢进诊疗指南》标准[1],并且病人临床资料齐全。8例病人主要症状有腰背部疼痛、下肢疼痛、肢体无力行走困难,这些症状单独或同时出现。其中4例出现腰痛伴肢体乏力及活动受限,3例出现腰痛伴下肢疼痛,1例出现腰背部疼痛合并下肢疼痛及肢体无力行走困难。2例病人病程中出现全身骨痛、乏力、倦怠、淡漠、厌食等表现。阳性体征主要包括感觉异常、肌力减退、反射减弱或消失,其中2例病人出现下肢感觉减退,5例肌力减退,3例膝踝反射减弱或消失。见表1。
1.2实验室和辅助检查
本文8例PHPT病人治疗前血钙、甲状旁腺素(PTH)均升高,5例病人血磷低于参考值。7例病人行甲状腺超声检查,阳性6例,阳性者占85.6%;6例行甲状旁腺融合显像,阳性6例,阳性者占100%;4例行骨密度检查,全部达到骨质疏松诊断标准(T值≤-2.5),T值分别为-2.6、-3.3、-4.1、-5.3;1例Z 值降至-2.3,另外3例均低于-2.0。 8例病人均行脊柱MR或者CT检查,均发现影像学异常,5例表现为腰椎椎管狭窄或腰椎间盘突出(图1A、B)。2例考虑椎体骨折病人均行胸腰椎MRI检查,1例提示多发椎体骨折(图1C、D),1例为单发椎体骨折。见表1。
1.3诊疗过程及预后
初诊时误诊为原发性骨质疏松椎体压缩性骨折3例,腰椎间盘突出症3例,腰椎椎管狭窄症2例。3例因高钙血症引起医生注意,2例因脊柱微创手术(经皮穿刺椎体后凸成形术)后反复发生椎体骨折并出现全身乏力症状引起注意,2例因脊柱手术(腰椎后路减压植骨融合内固定术)干预后腰腿痛、下肢乏力症状不缓解被发现,1例因并发肾结石被诊断。本组8例病人中有7例行手术治疗切除甲状旁腺病灶,1例行病灶穿刺术活检;术后病理检查证实5例为甲状旁腺腺瘤,1例为甲状旁腺增生,2例为甲状旁腺癌。随访10个月~4年,术后病人PTH及血清钙水平均恢复正常,未行甲状旁腺手术的1例病人出现肾衰竭表现,1例甲状旁腺癌病人于术后第2年出现肺转移,其余病人腰腿痛、骨痛等临床症状均明显减轻。
2讨论
2.1PHPT疾病概述
PHPT系甲状旁腺组织原发病变导致的一组临床症候群[1]。该病表现不典型,病人多出现骨骼、肾脏损害的临床表现,在我国PHPT病人临床表现以骨骼损害多见,表现为全身骨痛、背痛、关节痛,以及骨密度减低[2]。绝经后妇女最常见的表现是出现高钙血症和PTH水平升高。PHPT病理以单个甲状旁腺腺瘤最常见(80%~90%),少数为甲状旁腺增生或甲状旁腺癌[3]。PHPT并不像以前认为的那样罕见,其发病率有被严重低估的可能。在美国,目前PHPT是仅次于糖尿病和甲状腺疾病的第三大常见内分泌疾病,男女患病率之比约为1∶3,分别为8.5/10 000和23/10 000。PHPT可发生于任何年龄,绝经后女性较多见。人口学研究表明,PHPT的发生率以非裔美国人群最高,其次是白人、亚洲人和西班牙人[4]。PHPT的病因目前仍不明确,可能与原癌基因的活化与抑癌基因的失活,以及颈部照射史及锂剂的使用有关[5-6]。在中国,由于该病少见且临床表现不典型极易误诊,国内相关研究显示其误诊率约为70%[7]。有症状的PHPT可能是不常规进行生化筛查试验的国家中最显著的疾病形式[5]。近年来,随着常规生化筛查和颈部超声的应用,我国无症状PHPT病人占比不断增加,应引起重视[8]。
2.2PHPT诊断及与相关疾病鉴别
高PTH血症(血PTH高出正常值2倍)[9]、超声等影像学检查发现甲状旁腺增大是PHPT诊断的重要依据,高钙血症、低磷血症是重要参考依据[1]。本研究中7例病人血PTH水平高出正常参考值2倍。单纯原发性骨质疏松的病人,血钙一般正常或偏低,血磷正常,血PTH正常。而单纯腰椎间盘突出症或腰椎椎管狭窄症的病人,上述生化指标多为正常。
PHPT病人常因骨质疏松导致椎体骨折,应与原发性骨质疏松椎体骨折进行鉴别。本研究中有3例病人因未及时诊断PHPT,多次发生椎体骨折。骨密度T值≤-2.5为骨质疏松症诊断的标准[10]。 本文4例行骨密度检查的病人均达到骨质疏松诊断标准。骨质疏松症分为原发性骨质疏松症和继发性骨质疏松症,由PHPT导致的骨质疏松症为继发性骨质疏松。单纯原发性骨质疏松症于绝经后女性中多见,如无并发症,病人通常不出现症状;而由PHPT导致的骨质疏松症病人可出现全身骨痛、腰腿痛、关节疼痛和无力等,部分病人还会出现神经精神症状,如焦虑、抑郁、记忆力减退、烦躁不安、注意力不集中和睡眠障碍等。本文2例病人病程中出現了倦怠、淡漠、厌食等神经精神症状。影像学方面,PHPT导致的骨质疏松症病人骨膜下骨吸收为出现最早和特异性最高的X线征象[11-12];若病人病程较长,除表现为普遍骨质疏松症,还可表现为局限性骨破坏吸收伴骨性纤维组织增生、囊肿形成(因囊肿内含有棕色液体被称为棕色瘤),最常累及面部骨骼、锁骨、肋骨、骨盆和股骨,脊柱受累不常见 [13]。骨密度测定Z值对发现PHPT也有一定的意义,Z值负值越小则PHPT导致骨质疏松症的可能性越大,当Z值<-2.0时,这种意义更加明显 [14]。本文4例行骨密度检查的病人中,1例Z 值降为-2.3。另外,由PHPT导致的椎体骨折常累及多个椎体,程度较严重 [15]。本文3例骨质疏松椎体骨折病人中,2例因未及时诊断PHPT而发生严重的多发椎体压缩性骨折。
PHPT骨骼系统表现有全身骨痛、腰背痛、下肢疼痛等症状,易与腰椎椎管狭窄症、腰椎间盘突出症混淆。腰椎椎管狭窄症、腰椎间盘突出症多根据病人症状、体征,结合影像学检查进行诊断。临床工作中部分医生不注重病人的症状及查体,过多关注影像学检查资料,导致疾病的误诊。腰椎间盘突出症导致的疼痛多沿单侧下肢神经分布区域发生,与受累神经根有密切的对应关系 [16];而PHPT导致的疼痛与神经分布区域无明确对应关系。腰椎间盘突出症病人后期出现的肌无力以及反射减弱也与神经支配有关,而PHPT病人则多出现近端肌肉肌力减弱,并且部分病人出现反射亢进 [2]。然而,当病人因PHPT导致腰腿痛或肢体无力而同时伴有腰椎间盘突出或者腰椎管狭窄时,则易误诊。需要强调的是,腰椎间盘突出和腰椎椎管狭窄仅是一种影像学表现,只有伴随相应临床表现才能诊断为腰椎间盘突出症或者腰椎椎管狭窄症 [17]。
2.3需警惕PHPT的发生
文献报道有15%~40% 的 PHPT 病人可发生泌尿系结石[1,18]。本研究中3例病人出现泌尿系结石。若病人目前存在或既往出现泌尿系结石,则PHPT的可能性更大。此外,以下病人应注意排查PHPT:①骨质疏松伴多发椎体骨折或反复发生椎体骨折的病人;②腰椎影像学异常不能完全解释病人腰腿痛及肢体无力症状;③发现血钙异常升高且不能用其他原因解释的病人。
2.4PHPT治療与预后
对于有临床症状的PHPT病人,排除手术禁忌证后行手术治疗[19-20],术后病人生化检查结果异常得以纠正,骨质疏松得到改善,发生骨折风险降低 [21-22]。PHPT及时诊断后进行手术干预,效果一般较好,术后病人腰痛及下肢疼痛无力症状会得到缓解,考虑与甲状腺切除术后PTH以及血钙水平恢复正常有关。对于合并腰椎间盘突出的病人,可先行PHPT治疗,若症状缓解不明显则考虑行腰椎间盘突出症的进一步治疗。无症状的PHPT病人是否需要手术尚存在争议,手术是否会降低椎体骨折发病率仍不清楚[23]。因各种原因未行手术治疗的病人,应该每年检测血清钙、血清肌酐、估计肾小球滤过率及骨密度等 [5,24]。
综上所述,PHPT病人可以腰腿痛为首发症状就诊于脊柱外科,临床医生对该类病人诊治时应警惕PHPT的存在并及时干预。
[参考文献]
[1]中华医学会骨质疏松和骨矿盐疾病分会,中华医学会内分泌分会代谢性骨病学组. 原发性甲状旁腺功能亢进症诊疗指南[J]. 中华骨质疏松和骨矿盐疾病杂志, 2014,7(3):187-198.
[2]PAPPU R, JABBOUR S A, REGINATO A M, et al. Musculoskeletal manifestations of primary hyperparathyroidism[J]. Clinical Rheumatology, 2016,35(12):3081-3087.
[3]MACHADO N N, WILHELM S M. Diagnosis and evaluation of primary hyperparathyroidism[J]. The Surgical Clinics of North America, 2019,99(4):649-666.
[4]RAO S D. Epidemiology of parathyroid disorders[J]. Best Practice & Research Clinical Endocrinology & Metabolism, 2018,32(6):773-780.
[5]BILEZIKIAN J P, CUSANO N E, KHAN A A, et al. Primary hyperparathyroidism[J]. Nature Reviews Disease Primers, 2016,2:16033.
[6]DILLENBERGER S, BARTSCH D K, MAURER E, et al. Single centre experience in patients with primary hyperparathyroidism: sporadic, lithium-associated and in multiple endocrine neoplasia[J]. and, 2020,128(10):693-698.
[7]丁金勇,任东成,任之强,等. 原发性甲状旁腺功能亢进症28例误诊剖析[J]. 临床误诊误治, 2019,32(2):5-9.
[8]ZHAO L, LIU J M, HE X Y, et al. The changing clinical patterns of primary hyperparathyroidism in Chinese patients: data from 2000 to 2010 in a single clinical center[J]. The Journal of Clinical Endocrinology and Metabolism, 2013,98(2):721-728.
[9]徐少明,王平,郑毅雄,等. 原发性甲状旁腺功能亢进症的临床特点及治疗[J]. 中华医学杂志, 2001,81(23):1453-1455.
[10]JOHNSTON C B, DAGAR M. Osteoporosis in older adults[J]. The Medical Clinics of North America, 2020,104(5):873-884.
[11]王韬,倪建平. 原发性甲状旁腺功能亢进症的运动系统表现(附8例报告)[J]. 疑难病杂志, 2008,7(1):46.
[12]PYRAM R, MAHAJAN G, GLIWA A. Primary hyperparathyroidism: skeletal and non-skeletal effects, diagnosis and management[J]. Maturitas, 2011,70(3):246-255.
[13]AGNIHOTRI M, KOTHARI K, NAIK L. Ω Brown tumor of hyperparathyroidism[J]. Diagnostic Cytopathology, 2017,45(1):43-44.
[14]朱晓颖,朱汉民. 临床诊断中骨密度测定的若干问题[J]. 中国骨质疏松杂志, 2013,19(12):1315-1317,1322.
[15]CHOI M K, KIM S M. Nontraumatic multiple vertebral compression fractures induced by primary hyperparathyroidism: a case report and literature review[J]. World Neurosurgery, 2017,108:992.e5-992.e9.
[16]中华医学会骨科学分会脊柱外科学组,中华医学会骨科学分会骨科康复学组. 腰椎间盘突出症诊疗指南[J]. 中华骨科杂志, 2020,40(8):477-487.
[17]BENZAKOUR T, IGOUMENOU V, MAVROGENIS A F, et al. Current concepts for lumbar disc herniation[J]. International Orthopaedics, 2019,43(4):841-851.
[18]SAPONARO F, CETANI F, MAZONI L, et al. Hypercal-ciuria: its value as a predictive risk factor for nephrolithiasis in asymptomatic primary hyperparathyroidism[J]? Journal of Endocrinological Investigation, 2020,43(5):677-682.
[19]NILSSON I L. Primary hyperparathyroidism: should surgery be performed on all patients? Current evidence and residual uncertainties[J]. Journal of Internal Medicine, 2019,285(2):149-164.
[20]MAJCEN M, HOCEVAR M. Surgical options in treating patients with primary hyperparathyroidism[J]. Radiology and Oncology, 2020,54(1):22-32.
[21]UDN P, CHAN A, DUH Q Y, et al. Primary hyperparathyroidism in younger and older patients: symptoms and outcome of surgery[J]. World Journal of Surgery, 1992,16(4):791-797;discussion798.
[22]HUANG D K R, CHOU F F, CHI S Y, et al. Surgical ma-nagement of primary hyperparathyroidism: a single-center experience[J]. Asian Journal of Surgery, 2018,41(4):377-383.
[23]ZHANG L, LIU X M, LI H W. Long-term skeletal outcomes of primary hyperparathyroidism patients after treatment with parathyroidectomy: a systematic review and meta-analysis[J]. Hormone and Metabolic Research=Hormon-Und Stoffwechselforschung=Hormones et Metabolisme, 2018,50(3):242-249.
[24]OBERGER MARQUES J V, MOREIRA C A. Primary hyperparathyroidism[J]. Best Practice & Research Clinical Rheumatology, 2020,34(3):101514.
(本文編辑黄建乡)

