Concurrent laparoscopic management of giant adrenal myelolipoma and contralateral renal cell carcinoma
Dear editor,
Myelolipomas are uncommon,benign tumors of the adrenal gland that can occasionally attain a large size.These tumors,very rarely,can occur along with renal cell carcinoma[1].We describe the first case of a giant right sided adrenal myelolipoma co-existent with a contralateral renal cell carcinoma, both of which could be operated laparoscopically in the same sitting.
A 54-year-old male presented with history of discomfort in the right hypochondrium for 1 month.He was hypertensive but had no other co-morbidity.The clinical examination and the routine blood investigations were within normal limits.Ultrasound examination revealed a mass in the left kidney and right adrenal gland.He was referred to us for further management.A contrast enhanced computed tomography (CT) scan was performed which revealed a 61 cm×74 cm×79 cm heterogeneously enhancing lesion in the inter-pole and lower pole of the left kidney,suggestive of a renal cell carcinoma.The left adrenal gland was not involved while the right adrenal gland showed a well circumscribed lesion of 12 cm×10 cm×8 cm in size with fat densities suggestive of a myelolipoma (Fig.1).The metastatic and endocrine work-up was normal.
A concurrent laparoscopic management of the left renal cell carcinoma and the right myelolipoma was planned with an attempt to preserve the left adrenal gland in order to prevent adrenal insufficiency.The patient, under general anaesthesia, was placed in the right lateral position.The standard ports for transperitoneal nephrectomy were made and using a combination of blunt and sharp dissection, the left kidney was mobilized.The renal artery was clipped and divided.The left renal vein was isolated and clipped distal to the left adrenal vein in order to maintain the drainage of the left adrenal.The left adrenal gland was separated from its attachments with the kidney and could be spared(Figs.2A and 2B).The kidney was placed in a bag and kept in the pelvis of the patient.The patient was then placed in the left lateral position and using the standard ports, the right adrenal myelolipoma was mobilized from the kidney and liver.The right adrenal vein was clipped and divided and the gland could be excised using blunt and sharp dissection (Figs.2C and 2D).The adrenal was also bagged and both the specimens were delivered by a lower abdominal Pfannenstiel incision(Figs.2E and 2F).The total duration of surgery was 160 min and the blood loss was less than 50 mL.The patient made an uneventful recovery and was discharged on the 4th postoperative day.Histopathological examination revealed a unifocal clear cell renal cell carcinoma of Fuhrman Grade 2 in the mid pole of left kidney without evidence of sinus invasion or peri-nephric extension (pT1b).The right adrenal showed cells with vacuolated cytoplasm and eccentric nucleus along with myeloid precursors, consistent with myelolipoma.
Myelolipomas constitute nearly 3%of all primary adrenal tumors [2].The patients are usually asymptomatic and the lesions are diagnosed incidentally.These tumors vary insize and can occasionally become very large when they are called giant myelolipomas.These tumors, especially the giant ones, can rupture and cause retroperitoneal haemorrhage.Surgical excision is advised if they are causing symptoms or if the size is more than 5 cm as the chances of spontaneous haemorrhage increase significantly in big tumors.In the present case, though the management of the left renal cell carcinoma was more important but since he had symptoms on the right side and also as the size of the adrenal lesion was >5 cm, a concurrent excision of the lesions was planned.Laparoscopy has become the gold standard for the management of adrenal tumors.As the experience and skills are increasing, adrenal tumors of any size can be successfully removed laparoscopically in presence of favourable tumour and patient related factors [3].

Figure 1 Contrast enhanced computed tomography scan images of patient demonstrating the left heterogeneously enhancing renal cell carcinoma (broken arrow) and the fat containing right adrenal myelolipoma (bold arrow).(A) The cross sectional image; (B) The coronal image.
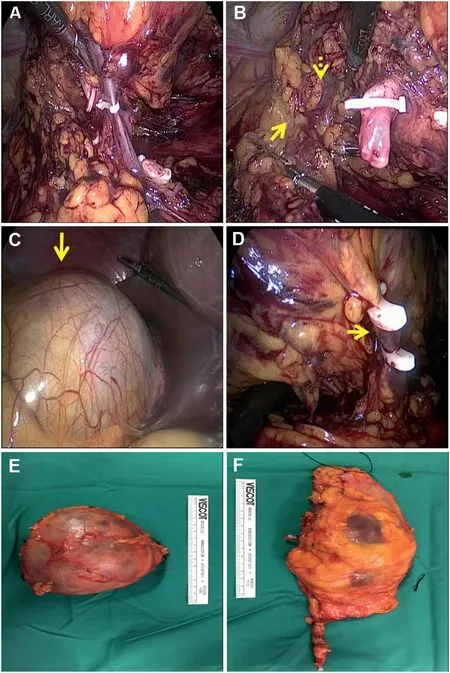
Figure 2 The surgical images of the right adrenal and the left kidney.(A)Intraoperative picture showing the hilum of the left kidney with clips on renal artery and vein; (B) The left adrenal (bold arrow) being separated from the upper pole cortex (broken arrow) of the kidney; (C) The right adrenal myelolipoma; (D) The right adrenal vein clipped; (E) The specimens of right adrenal myelolipoma; (F) The left kidney(without the adrenal).
Adrenal myelolipomas have rarely been reported to be concurrently present along with renal cell carcinoma.One of these reports has shown tumors to be present on the ipsilateral side[1].Only in few instances, contralateral coexistence of renal cell carcinoma with adrenal myelolipoma has been reported in the English literature.Hofmockel et al.[4]described a case of left sided renal cell carcinoma and a right adrenal myelolipoma of 11 cm in size.The authors performed an open nephrectomy followed by an open adrenalectomy after 2 months.Laparoscopy has been sparingly used in the setting of co-existent tumors due to complexity involved in the approach.Senthil et al.[2]described the first case of a concurrent laparoscopic excision of a left sided renal cell carcinoma with a 4 cm ipsilateral adrenal myelolipoma managed.Our case is peculiar as this is the first case in which contralateral carcinoma of kidney and giant adrenal myelolipoma were present which could be concurrently excised laparoscopically.The size of the right adrenal myelolipoma and the desirability to preserve the normal left adrenal to prevent adrenal insufficiency made this surgery still more challenging.
Author contributions
Study design: Tarun Jindal.
Data acquisition: Tarun Jindal, Pravin Pawar, Neeraj Subedi.
Data analysis: Tarun Jindal.
Drafting of manuscript: Tarun Jindal.
Critical revision of the manuscript: Pravin Pawar, Neeraj Subedi.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2022年1期
Asian Journal of Urology2022年1期
- Asian Journal of Urology的其它文章
- Chromophobe renal cell carcinoma: Novel molecular insights and clinicopathologic updates
- The role of preoperative dutasteride in reducing bleeding during transurethral resection of the prostate: A systematic review and meta-analysis of randomized controlled trials
- Efficacy and safety of desmopressin on frequency and urgency in female patients with overactive bladder and nocturia,current clinical features and outcomes: A systematic review
- The impact of the coronavirus disease 2019 pandemic on elective urological procedures in Australia
- Efficacy of a combination of dutasteride,tadalafil,and solifenacin in the treatment of previously unsuccessful patients
- Associations between IL-1RN variable number of tandem repeat, IL-1β(-511)and IL-1β (+3954) gene polymorphisms and urolithiasis in Uighur children of China
