Mini versus ultra-mini percutaneousnephrolithotomy in a paediatric population
Dilip K.Mishr , Soni Bhtt , Sundrm Plnippn ,c,,Tlmnchi V.K.Reddy , Vinothkumr Rjenthirn ,Y.L.Sreerng , Mdhu S.Agrwl
a Department of Urology, Global Rainbow Hospital, Agra, Uttar Pradesh, India
b Department of Pediatrics, F H Medical College, Agra, Uttar Pradesh, India
c Department of Urology, Sengkang General Hospital, Singapore
KEYWORDS Percutaneous nephrolithotomy;Mini percutaneous nephrolithotomy;Ultra-mini percutaneous nephrolithotomy;Minimally invasive percutaneous nephrolithotomy;Paediatric percutaneous nephrolithotomy;Renal stone;Urolithiasis
Abstract Objective: To evaluate whether there would be a difference in outcome when the smaller ultra-mini 12 Fr sheath was used instead of the mini 16 Fr sheath for percutaneous nephrolithotomy (PCNL) in paediatric patients for stones less than 25 mm.Methods: This was a prospective cohort study of patients who underwent PCNL in our hospital in a 2-year period from July 2016 to June 2018 by a single surgeon.PCNL was performed in a prone position and tract was dilated to the respective size using single step dilatation.Laser was used to fragment the stone.Stone-free outcome was defined as absence of stone fragment at 3 months on kidney, ureter, and bladder X-ray.Results: There were 40 patients in each group.Mean stone size was comparable between the two groups (14.5 mm vs.15.0 mm).The procedure was completed faster in the 16 Fr group compared to 12 Fr group (24.5 min vs.34.6 min).Stone clearance was highly successful in both groups (97.5% vs.95.0%).There was no difference in complications between the two groups.The decrease in hemoglobin was minimal in both groups (0.2 g/dL vs.0.3 g/dL).Conclusion: We found that the success rates were similar in both mini PCNL and the smaller ultra-mini PCNL groups.No significant difference in bleeding was noted in our pilot study,however, operative time was longer in the ultra-mini group as compared to the mini sheath group.
1.Introduction
Paediatric urolithiasis has increased globally in the last few decades.There has been a change in the pattern of stone composition with an increase in the frequency of kidney stones and a decrease in bladder stones [1].Besides, there is more imaging that is performed leading to higher rates of stone detection [2].Children represent 2%-3% of the total population of stone-formers [3].Management of paediatric urolithiasis necessitates a multidisciplinary approach as the removal of the stone is just the first step.Percutaneous nephrolithotomy(PCNL)is the primary treatment option for paediatric staghorn and renal stones of size more than 2 cm as well as lower pole stones more than 1 cm.Besides,it remains a second option for smaller renal calculi as per European Association of Urology guidelines [4].PCNL has the most consistent and best stone clearance rates in renal stone management.However, it is associated with more complications.The most common and dreaded one is bleeding.The significant factors associated with haemorrhage during percutaneous renal surgery are larger sheath size, prolonged operative time,the caseload of the operating surgeon,greater stone burden, and multiple tracts [5,6].
Various techniques to reduce blood loss during PCNL have been described.These focus on reducing the tract size,and hence reducing the parenchymal and infundibular trauma.The most notable ones are mini PCNL where sheaths from 15 Fr to 20 Fr are deployed, ultra-mini PCNL where sheath sizes range from 11 Fr to 14 Fr, and micro PCNL which uses 4.8 Fr.Schilling et al.[7]have proposed a uniform terminology for PCNL based on the outer sheath size(XL ≥25 Fr;L 20 Fr to <25 Fr;M 15 Fr to <20 Fr;S 10 Fr to <15 Fr; XS 5 Fr to <10 Fr; and XXS <5 Fr).Significantly,less bleeding was observed in the mini PCNL population.The smaller sheath also made it easier to manoeuvre the sheath within the pelvicalyceal system.As a result,we have been routinely using mini PCNL sheaths of size 16 Fr for our adult patients.We aimed to evaluate whether there would be a difference in outcomes, particularly in terms of bleeding, hospitalisation stay, and stone clearance when the even smaller sheaths of 12 Fr(also known as ultra-mini)were used instead of the 16 Fr sheath (also known as mini)in the paediatric population.There have been comparisons of standard size PCNL and mini PCNL, however ours is the first study that compares mini PCNL with the smaller ultramini PCNL to our knowledge.
2.Patients and methods
This was an observational study with prospectively collected data of PCNL procedures done from July 2016 to June 2018.Institutional review board approval (2016-45)was obtained for the study.The study consists of two groups where alternate patients were selected either for PCNL with 16 Fr sheath or 12 Fr sheath.
The inclusion criteria consisted of paediatric patients(<18 years) with unilateral kidney stones measuring less than 25 mm, normal renal function, American Society of Anaesthesiologists score of 1 or 2, and patient preference for percutaneous stone removal.Patients with partial or complete staghorn stones, congenital anomalies, bleeding diathesis, or history of previous open surgery were excluded from the study.Preoperative patient histories,physical examinations, and routine laboratory tests,including urine analysis, urine culture, serum urea, serum creatinine, complete blood cell count, and coagulation tests were evaluated.Abdominal ultrasonography was done in all patients as the initial screening procedure, followed by low-dose computed tomography (CT).Patients who had positive urine cultures were treated with appropriate antibiotics preoperatively.The Storz minimally invasive PCNL(MIP) system (Karl Storz, Tuttlingen, Germany) utilizes a 7.5 Fr nephroscope which can be placed through operating sheaths of size 12 Fr.This has been termed MIP with small size (MIP S).We commonly use MIP with medium size(MIP M) which consists of a 12 Fr nephroscope that works with an access sheath of 16 Fr in our adult patients who undergo mini PCNL.
The basic technique of PCNL was followed in both groups.All procedures were done under general anaesthesia.A paediatric cystoscope was used to place a 5 Fr multi hole ureteric catheter in the pelvicalyceal system.The initial puncture was made with ultrasonography and fluoroscopic guidance in a prone position.An 18-gauge trocar tip two-part puncture needle (Cook Urological,Bloomington, IN, USA) was used for puncture through the flank and into the chosen calyx of the kidney.A hydrophilic nitinol(Terumo,Tokyo,Japan)guidewire of size 0.035 inch was passed through the needle and the tract was dilated by passing a Teflon dilator over the guidewire.Unlike in conventional PCNL, only a single-step dilatation was done followed by the insertion of access sheath of the desired size.The Storz MIP is a single step dilatation system which allows the sheath placement after single dilatation.It helps save time,radiation exposure,and also minimizes trauma to the renal parenchyma.Irrigation was with gravity alone with no pressurized system.
Stones were fragmented using Holmium:YAG laser(Lumenis, Yokneam, Israel) using a 500/365 μm end-firing optical fibre, using power up to 60 W (1-2 J/15-30 Hz).Stone fragments were washed out using the “vacuum cleaner” effect.There was spontaneous expulsion of stone fragments through the sheath under the influence of the turbulence produced by the irrigation fluid, as opposed to conventional PCNL, where each fragment either required manual extraction or utilisation of a suction device.Graspers were used very rarely in the patients who underwent PCNL using the MIP system.
After the procedure, clearance was confirmed by direct visualization of the collecting system, combined with fluoroscopy.All MIP procedures in our unit are routinely tubeless procedures unless there is excessive bleeding,perforation within the pelvicalyceal system, or infection.Hence we left only a ureteric catheter and Foley’s catheter indwelling overnight.No nephrostomy tube was placed in any patient.Double-J stent was used only in patients with oedema or obstruction at the pelviureteric junction or the upper ureter.The intraoperative assessment of pelviureteric junction was done by the operating surgeon to decide on the placement of the double-J stent.The stent was always placed antegrade in the prone position at the end of the PCNL.Intravenous paracetamol and diclofenacsuppository were used for analgesia in all patients postoperatively.Patients were discharged after both urethral and ureteric catheters were removed together,typically on the first postoperative day.If a double-J ureteral stent was inserted,it was removed 3-4 weeks after the procedure at the follow-up visit.Stents were removed with sedation or short general anaesthesia in all the children on a day-care basis.A metabolic evaluation was requested in all the children during follow-up, however, not all of them completed the workup.
We assessed the outcomes of operating time, stone clearance rates, complications, and hospital stay.Haemoglobin level was measured,and a kidney,ureter,and bladder(KUB)X-ray was done in all patients on postoperative Day 1.The patient was discharged from the hospital once the ureteric catheter was removed and the patient could void well.Complications were graded according to the Clavien grading of complications.Our stone clearance was defined as the absence of any stone fragment on the KUB X-ray.An ultrasound of the kidney was also done at 1 month after the surgery.A non-contrast CT scan was not preferred due to the concerns associated with excessive radiation.Patients with residual stones which was clinically significant >4 mm in size were counselled for adjunct procedures such as extracorporeal shockwave therapy, retrograde intrarenal surgery, or close observation.Further follow-up of all patients was done at 3 months postoperatively.
All continuous variables were tested for the normality using Shapiro-Wilk’s test.Normally distributed continuous variables were expressed as mean and standard deviation.Non normally distributed variables were represented by median and interquartile range.Categorical variables were represented by percentage.Comparison of normally distributed continuous variables were done by independent sample t-test.Mann-Whitney U test was adopted when the variables were not normally distributed.Comparison of categorical variables were done by either Chi-square test or Fisher’ Exact test based on the number of observations.Data entry was done in Microsoft Excel.Data analysis and validation were done by SPSS Statistics for Windows version 25.0 (IBM, Armonk, NY, USA).All p-values <0.05 were considered as statistically significant.
3.Results
There were a total of 80 patients in our study.The demographic variables of both groups are shown in Table 1.The cases were analysed according to the initial allocated group.There are no significant differences between the two groups in terms of age, gender, laterality, stone size,and stone location.Most stone formers were males.The majority of the stones were located in the renal pelvis and upper ureter.
Table 2 shows the intraoperative and postoperative outcomes.The access created for mini PCNL depends on the stone location.As such, the majority of the tracts were placed through the middle or upper calyx which would allow a direct approach to the stones located in the renal pelvis and upper ureter.Time taken for the procedure was significantly longer in the group who underwent PCNL using the MIP S system (34.6 min) compared tothe MIP M group (24.5 min).The evacuation of stone fragments through a smaller sheath requires a longer time to attain smaller fragments using the same energy.Five patients in the MIP S group required conversion to the larger sheath due to poor vision from bleeding.The drop in haemoglobin was minimal(0.3 g/dL vs.0.2 g/dL,p=0.83)and the bleeding complications were not different between the two groups.A higher number of patients had a fever in the smaller sheath group but this was not significantly different.
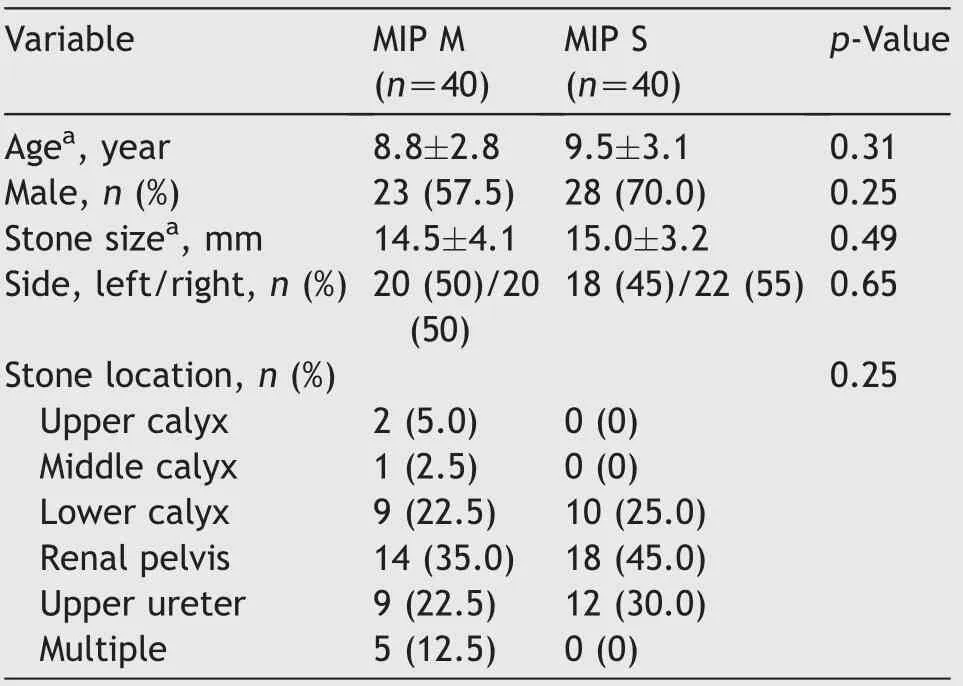
Table 1 Patient demographics.

Table 2 Intraoperative and postoperative parameters.
The postoperative drainage was not different between the two groups.All patients had a tubeless procedure.Most of the patients had a ureteric catheter for drainage whilst athird of them in each group underwent stenting.The hospital stay was significantly longer by 6.6 h in the patients with the smaller sheath but this was certainly not a clinically important difference when assessing in terms of the number of days spent in the hospital.Stone clearance was achieved in over 95% of patients in both groups.Those patients who had residual stones, elected for observation as their stone fragments were clinically insignificant.
4.Discussion
Paediatric stone disease is rising in incidence, mostly associated with metabolic abnormalities.The main objective in the management of a child with a stone disease is to achieve complete clearance and preserve renal function whilst minimizing complications and radiation exposure.With the advent of newer technology,the management has shifted from open surgical approaches to that of the minimally invasive endoscopic techniques.Miniaturization of technology with its smaller access sheaths, nephroscopes,instruments, and accessories has formed the crux of this evolution.Even though paediatric patients are high-risk stone formers, many patients with non-obstructing and asymptomatic stones are offered active surveillance for the fear of parenchymal damage from surgical intervention.This has been overcome partly with the minimally invasive and endoscopic procedures.The various options available in the management of calculi are shockwave lithotripsy,retrograde intrarenal surgery,and PCNL.Open surgeries are not performed for stone clearance unless associated with anatomical abnormalities that also require surgical correction.
The role of PCNL in the management of paediatric stone disease was first shown by Woodside and colleagues in 1985 with 100%stone removal in one session using standard adult instruments [8].However, PCNL is associated with complications like bleeding requiring transfusions, organ injuries,and pneumothorax.Most of the complications are related to the larger tract size (24 Fr-30 Fr) [6].The other concern was the potential renal damage due to PCNL in young children whose organs are still developing [9].The use of miniaturized instruments has increased the practice of PCNL in children as it may potentially limit the complications.A smaller tract may result in a smaller risk of bleeding and pelvicalyceal perforation but a higher risk of postoperative colic from the passage of small stone fragments [10].
The overall stone clearance rate was 96.3% in the 80 patients which were confirmed on postoperative KUB X-ray.The stone retrieval is accomplished by the vacuum cleaner effect described by Nicklas et al.[11]eliminating the tedious stone removal using forceps.This effect involves trapping multiple fragments in a low-pressure bubble in front of the sheath.Following this, the nephroscope is advanced and withdrawn repeatedly out of the sheath which results in fragment retrieval.Multiple stones may be removed in the irrigation stream as the nephroscope is withdrawn, achieving rapid clearance of the fragmented stones [11].Our overall mean operative time was 29.5 min which is comparable to other studies where mini PCNL was performed[10].Moreover,with the presence of the instrument in the channel,reduced irrigation flow would result in poorer vision prolonging the stone fragmentation and retrieval.The mini PCNL tract created by smaller dilators reduces the trauma to the kidney and hence lesser bleeding is usually seen.On the contrary, the smaller size of MIP S did not further reduce bleeding compared to the MIP M tract.The overall mean haemoglobin drop was only 0.24g/dL inour studybut wedid not noteanydifference when the smaller sheaths of 12 Fr were used as compared to the larger sheaths of MIP M (16 Fr).All things considered, the reduced bleeding,improved vision,and the vacuum cleaner effect shortened the operative time of mini PCNL.Given the small size of the kidney and the more compact collecting system of the paediatric population,it was logical to use the smallest and least traumatic instruments with the least number of punctures.This,in turn,reduces the likelihood of major complications including bleeding [12].There was no need for transfusion in our study.The other concern in paediatricPCNListheexposuretoradiation,whichwasminimized by using ultrasound guidance when obtaining access to the pelvicalyceal system and by utilizing the single-step dilatation of the MIP system under pulsed fluoroscopy.
Five patients in the smaller tract MIP S group required conversion to a larger tract of 16 Fr intraoperatively which allowed better irrigation and hence clearer vision.Without the dilatation to a larger tract, the operation would have taken a significantly longer duration due to bleeding which obscured the stone fragments.There was no such requirement in the MIP M group to convert to an even larger tract.The longer duration of surgery with its longer irrigation time resulted in higher intra renal pressure which is predictive of increased rates of febrile urinary tract infections (UTIs).Smaller tracts also caused higher intra renal pressures which resulted in pyelovenous backflow and higher chances of febrile UTI.This was independent to the duration of surgery [13].
The tubeless procedures have shown to reduce the morbidity of the PCNL.It is well known that the nephrostomy tube is associated with increased pain as well as prolonged urinary leakage after the removal of the tube.If the procedure was uncomplicated with minimal bleeding and no residual fragment seen intraoperatively, a tubeless procedure was carried out.None of our patients required a nephrostomy.There were 56 patients in our study who underwent a totally tubeless procedure with only a ureteric catheter left overnight while 24 children required double-J stent based on the procedural findings of either oedema around the pelviureteric junction or the upper ureter.Tubeless procedures also translated to the lesser postoperative pain, shorter length of stay, and ultimately greater patient satisfaction [14].
There were no major complications in our study, like pneumothorax or organ injuries.Celik et al.[15] have shown that the dilatation of percutaneous tract with smaller calibre instruments and using smaller sized rigid nephroscope can reduce the morbidity rates in PCNL.The other main advantage of using the MIP system was the easy accessibility to other parts of the pelvicalyceal system,unlike standard PCNL.We were able to avoid the second puncture in all our patients even when the stone migrated.This manoeuvre ability without producing torque or trauma to the kidney facilitated the assessment of stone clearance on nephroscopy.Together with the fluoroscopic view, we were able to ensure stone clearance in almost all patients during the surgery.
Dede et al.[16]reported on the use of ultra-mini PCNL in children.They utilized a 9.5 Fr paediatric cystoscope through a 12 Fr access sheath.Complete clearance was achieved in 87%of the patients.There was minimal bleeding(haemoglobin drop of 0.9 mg/dL) with none requiring a blood transfusion.They concluded that smaller sheaths cause little damage to the renal parenchyma, however, it did not compromise the efficacy of stone clearance [16].There has been a study comparing super-mini PCNL (SMP),which uses a 12 Fr/14 Fr sheath and a 7 Fr nephroscope,and mini PCNL, which uses 18 Fr sheath and an 8.0 Fr/9.8 Fr ureteroscope [17].They found no difference in the operative time and stone-free rates but SMP was superior in two aspects.The patients who underwent SMP had higher rates of tubeless procedure, shorter stay in hospital, and lower rates of complication.Despite the smaller sheath size, the benefits have been attributed to the design of the SMP system which allows for suction along the sheath[17].Other comparative studies have shown that ultra-mini PCNL is as effective as micro PCNL and standard PCNL with no differences in stone free rates and hospitalisation stay [18,19].Additionally, a randomised trial done in adult patients by Yavuz and colleagues [20] showed that a larger tract PCNL resulted in a longer stay in hospital and lengthier recovery to normal activity with a small increase in stone free rates.
Our study has its limitations.Though the sample size in the pilot study was small, this was a prospective cohort study with a follow-up of all patients at 3 months.The small sample size limits our findings in terms of infection and conversion to larger tract.Also,the overall mean stone size was small (14.8 mm).Larger stones were not included in this initial study as it was conducted in the early part of our experience with the smaller access sheaths.In addition,Guys stone score was not performed as majority of the stones (>80%) were single and either in the renal pelvis or in the lower calyx.We did not measure the pain scores in this population which may have shed further light on the postoperative pain experienced in the two groups.However, we believed that the hospital stay would allow us to infer that the pain was minimal at the time of discharge.KUB X-ray was performed postoperatively in our patients to assess for residual fragments.We acknowledge that the radiolucent stones may be missed in our follow-up imaging,however,due to cost limitations,we were unable to obtain ultrasound for all patients.Though the study is from a single-centre, all the PCNL surgeries were performed by a single surgeon with extensive experience in percutaneous renal surgery.Therefore, the fluoroscopy time was not measured as the differences would have been minimal in our series where the operating surgeon preferentially uses ultrasound guidance for renal access.Further studies,particularly randomized trials, are needed to corroborate the results we obtained.
5.Conclusion
We conclude that the mini and ultra-mini PCNL using the MIP system are effective and safe instruments in the management of paediatric stone diseases.The ultra-mini PCNL(MIP S) has a smaller diameter sheath that results in lesser trauma to the kidney in comparison to the mini PCNL(MIP M).However, the drop in haemoglobin was the same between the two groups.The stone clearance was equally effective although the operative time was longer when using the ultra-mini PCNL (MIP S).At present, mini PCNL(MIP M) can achieve excellent stone free rates for small to moderate stone burden in a shorter operative time.This can be confirmed in future prospective randomized controlled trial where PCNL is offered for all stone sizes.
Author contributions
Study concept and design: Dilip K.Mishra, Madhu S.Agrawal.
Data acquisition: Talamanchi V.K.Reddy, Vinothkumar Rajenthiran, Y.L.Sreeranga.
Data analysis: Sundaram Palaniappan, Talamanchi V.K.Reddy, Vinothkumar Rajenthiran, Y.L.Sreeranga.
Drafting of manuscript: Dilip K.Mishra, Sonia Bhatt, Sundaram Palaniappan.
Critical revision of the manuscript: Dilip K.Mishra, Sonia Bhatt, Sundaram Palaniappan, Madhu S.Agrawal.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2022年1期
Asian Journal of Urology2022年1期
- Asian Journal of Urology的其它文章
- Chromophobe renal cell carcinoma: Novel molecular insights and clinicopathologic updates
- The role of preoperative dutasteride in reducing bleeding during transurethral resection of the prostate: A systematic review and meta-analysis of randomized controlled trials
- Efficacy and safety of desmopressin on frequency and urgency in female patients with overactive bladder and nocturia,current clinical features and outcomes: A systematic review
- The impact of the coronavirus disease 2019 pandemic on elective urological procedures in Australia
- Efficacy of a combination of dutasteride,tadalafil,and solifenacin in the treatment of previously unsuccessful patients
- Associations between IL-1RN variable number of tandem repeat, IL-1β(-511)and IL-1β (+3954) gene polymorphisms and urolithiasis in Uighur children of China
