Management of proximal biceps tendon pathology
INTRODUCTION
While the role of the long head of the biceps tendon (LHBT) in shoulder pathology has been studied extensively, the management of such pathology has evolved.Recently, studies have demonstrated that biceps tenodesis can be used to treat individuals with symptomatic superior labrum anterior to posterior (SLAP) lesions[1-3].As a result, the number of biceps tenodesis procedures performed each year has increased[4].Despite this rise in volume, there is no consensus on which procedure-biceps tenotomy, biceps tenodesis, or SLAP repair is superior in terms of clinical outcomes.Typically, orthopaedic surgeons use their preference and specific patient factors to determine which procedure is ideal for each patient.Furthermore, in patients who undergo biceps tenodesis, there is controversy as to whether orthopaedic surgeons should utilize openarthroscopic techniques, the best method of fixation with interference screws, suture anchors, or cortical buttons, and the ideal location of tenodesis with intra-articular, suprapectoral, subpectoral, extra-articular top of groove, or extraarticular bottom of groove approaches.Regardless of this debate, researchers can agree that the LHBT is widely recognized as an important pain generator, especially in anterior shoulder pain and dysfunction[5-8].
The purpose of this review is to provide a current understanding of LHBT anatomy, function, and clinical information such as evaluation, nonsurgical management, surgical management, and complications in hopes of helping orthopaedic surgeons counsel their patients.
ANATOMY AND FUNCTION
An appreciation of the LHBT anatomy and its surrounding structures is helpful to understand normal function as well as proximal pathologic injuries (Figures 1 and 2)[9,10].The LHBT originates from the supraglenoid tubercle and the superior glenoid labrum and exits the glenohumeral joint through the bicipital groove[11].The attachment point of the LHBT on the superior labrum is variable amongst patients: equal anterior and posterior attachment is the most common (37%), predominantly anterior is the least common (8%), and other variations such as entirely posterior (22%) or mostly posterior (33%) also exist[12,13].As it exits the glenohumeral joint and before it enters the bicipital groove, the LHBT is stabilized by a capsule-ligamentous complex referred to as the biceps pulley, which consists of the subscapularis tendon, the supraspinatus tendon, the coracohumeral ligament, the pectoralis major tendon insertion, and the falciform ligament (Figure 1)[14,15].The LHBT then travels distally into the bicipital groove along the anterior surface of the humerus through the osteoligamentous sheath which is formed by the transverse humeral ligament as well as the greater and lesser tuberosities (Figures 1 and 2)[16].The LHBT and the short head of the biceps tendon, which originates from the coracoid process with the coracobrachialis, give rise to the muscle belly of the biceps brachii which externally rotates 90° before the tendons attach as a single tendinous insertion on the ulnar aspect of the bicipital tuberosity of the radius[6].

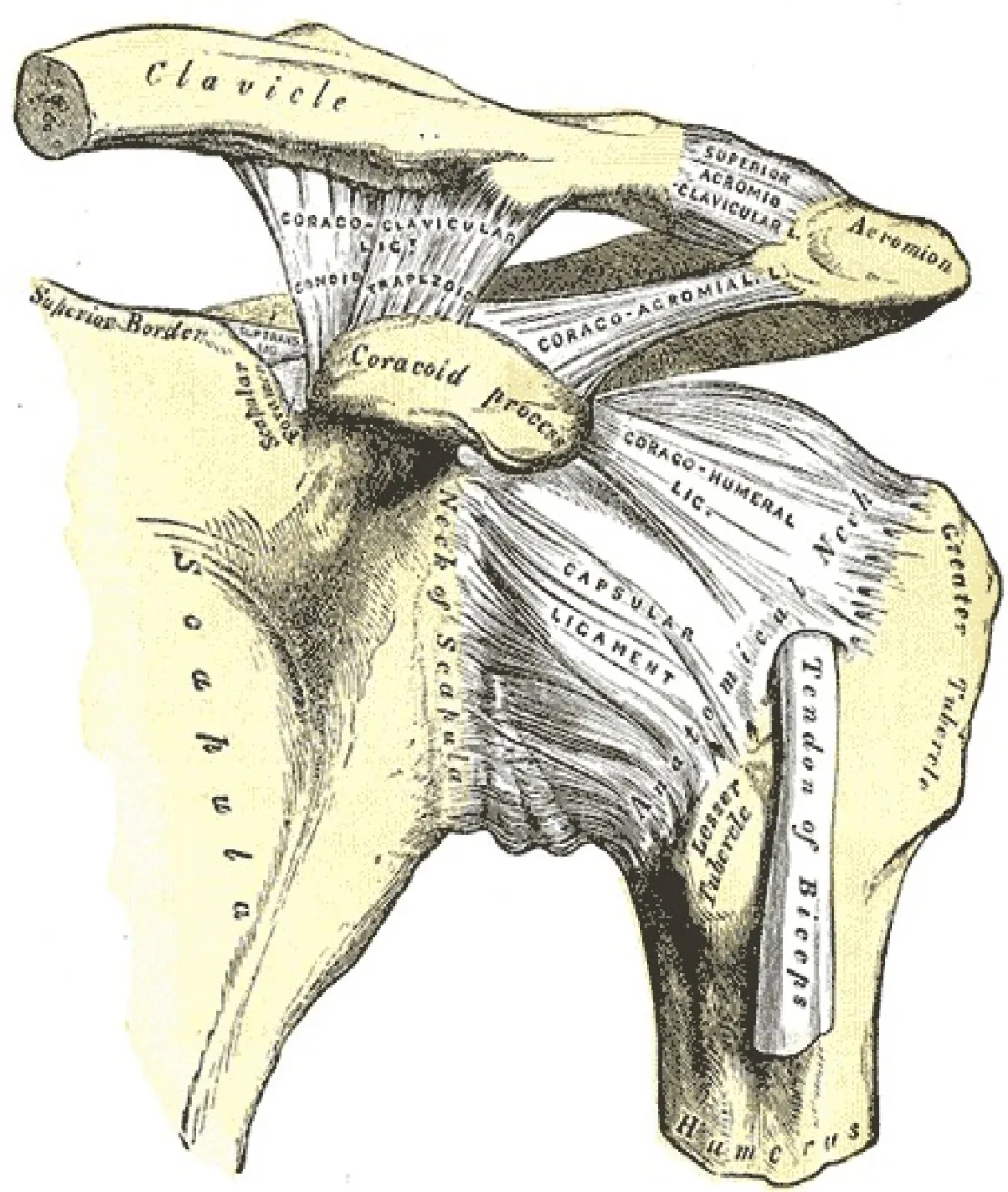
Furthermore, the long head of the biceps (LHB) and glenoid labrum have collectively been described as the “biceps-labral complex” (BLC) which can be categorized into three main parts: (1) The inside, which includes the superior labrum and the LHBT anchor at the supraglenoid tubercle; (2) The junction, which includes the intra-articular LHBT and its stabilizing pulley system; and (3) The bicipital tunnel, which includes the LHBT beginning at the articular margin of the humeral head adjacent to the pulley and extending to the subpectoral region (Figure 3)[17-19].The bicipital tunnel, which houses the extra-articular biceps, is further divided into three clinically relevant zones.Zone 1 stretches from the articular margin to the distal margin of the subscapularis.Zone 2 extends from the distal margin of the subscapularis to the proximal margin of the pectoralis major.Lastly, zone 3 is the subpectoralis region[20].
Bettelheim also observes: Since all the treasure and jewels given the princess by her mother are of no help to her, this suggests that what a parent can give his child by way of earthly goods is of little aid if the child does not know how to use it well (Bettelheim 1975, 139).Return to place in story.

The function of the LHBT still remains highly debated.Prior cadaveric studies have shown it may serve as a humeral head depressor, a stabilizer of the glenohumeral joint, or a stabilizer of the humeral head particularly in the anterosuperior and anterior directions of shoulder abduction[21-23].Other authors consider the LHBT to be a vestigial structure that is not active during isolated shoulder movements and may have a larger role in proprioception of the shoulder[24,25].Anatomically, there is consensus that the LHBT mainly functions as a forearm supinator while the short head of the biceps tendon mostly functions as an elbow flexor[6].
You re so darn negative and boring! I retorted. I happen to like crowds. They make me feel like I m part of something. I promise I won t buy anything but I m going to look around for fun anyways. You go for coffee and I ll meet you back here in half an hour.
PROXIMAL BICEPS TENDON PATHOLOGY
The pathologic entities involving the LHBT can be classified into three general categories: inflammatory, instability, and traumatic[8].Inflammation of the biceps tendon is commonly attributed to degenerative tendinopathy and overuse injuries.Additionally, rotator cuff tears and subacromial impingement can also lead to or be associated with bicipital tendinitis[26-30].Some studies have found a prevalence as high as 93% in the association of LHBT inflammatory injuries and rotator cuff tears[31].Instability of the tendon can create mechanical symptoms such as popping and clicking with range of motion.If the LHBT is unstable, the physician should highly suspect an associated subscapularis tendon tear or tears of the coracohumeral and/or superior glenohumeral complex[6,8].Lastly, the LHBT is susceptible to traumatic injury, most commonly a complete rupture of the tendon, where pain resolves over time and function is typically reserved.These injury categories have been associated with other various shoulder conditions such as glenohumeral arthritis, labral lesions, and anterior or anterosuperior rotator cuff tears[1,32-35].
Anatomically, the three main parts of the BLC are associated with specific pathologic entities[17].Injuries to the inside, which is predominantly associated with SLAP lesions, can be caused by superior migration of the humeral head, biceps tension, or peelback as a result of internal impingement[36].Injuries to the junction include LHBT tears, LHBT incarceration, biceps chondromalacia, hourglass biceps, and pulley lesions[37-39].The bicipital tunnel, specifically zones one and two, encompass LHBT tears, loose bodies, and tenosynovitis[18,40].
Evaluation
An in-depth history and physical examination must be done to differentiate biceps pain from other causes of referred shoulder pain[41].This can be difficult because individuals with biceps pain can also have concomitant pathologies such as rotator cuff tears and may even have similar symptoms to patients with SLAP lesions[42-44].As a result, physicians should utilize patient history, physical examination results, and imaging modalities to consider multiple differential diagnoses and help determine appropriate management.
Next morning she sat down beneath the walls of the castle to play with the golden apple, and the first person she saw was the maiden23 with the long nose, who was to have the Prince
A comprehensive history should be acquired when evaluating patients with LHBT injuries.A thorough history that documents the mechanism of injury can help the physician differentiate between various shoulder pathologies[45].Obtaining information such as hand dominance, history of injury/trauma to the shoulder area, symptom exacerbation with overhead activities, pain at rest and/or pain at night, history or current overhead sport participation, history of current manual labor occupation or employment status, and any relevant surgical history can be incredibly useful in conjunction with the physical examination to determine the etiology of the pain[45].
Physical examination should start with assessment of range of motion as well as neurovascular examination that includes strength testing of all rotator cuff muscles.Common LHBT conditions that should be differentiated with an in depth physical examination include inflammatory injuries, instability, and rupture.LHBT inflammatory changes such as tenosynovitis or tendinitis often presents with pain in the anterior aspect of the shoulder that radiates to the anterior biceps[46].Symptoms can be exacerbated by overhead activity or elbow flexion.LHBT instability will often present with reproducible clicking or tendon subluxation on physical examination[6].For this type of injury, the physician should pay special attention to the subscapularis muscle as LHBT instability is associated with rotator cuff tears, especially those of the upper border of the subscapularis[17].Therefore, physicians should also perform passive external rotation, lift-off, belly-press, and bear hug test for the subscapularis (Figure 4)[8,17,47].LHBT rupture often occurs with a tearing sensation anteriorly and presents with swelling and ecchymosis.Some patients may have a Popeye deformity or sagging biceps muscle belly which can be exaggerated by having the patient flex his biceps (Figure 5)[6,17,48].For these patients, muscle belly cramping has also been reported[49].In patients with symptomatic proximal biceps pathology, pain will often be localized to the bicipital groove.This pain can be elicited on direct palpation of the area 7 cm below the acromion with the arm adducted, internally rotated 10°, and the elbow flexed[50].To assist in proper palpation and pain elicitation, the shoulder should be internally and externally rotated in this position.
He took her money in one hand and with the other hand he grasped her mitten7 and said Take me to where you live. I want to see your brother and meet your parents. Let s see if I have the kind of miracle you need.
Some studies have compared open LHB tenodesis to arthroscopic LHB tenodesis in order to determine which is superior.Abraham[100] and Green[114] found excellent outcomes with both methods and low complication rates.Gombera[115] compared forty-six patients who underwent arthroscopic or open biceps tenodesis and found no significant differences in American Shoulder and Elbow Surgeons (ASES) scores, patient satisfaction scores, return to sports activity, pain levels at night, pain levels with heavy activity, or Popeye deformities.In terms of complications, arthroscopic biceps tenodesis mirrors open biceps tenodesis.Complications following arthroscopic biceps tenodesis include residual postoperative groove pain, injury to the surrounding neurovascular structures, and increased risk of early postoperative stiffness[116].Additionally, complications can be dependent on the fixation strategy.For example, open biceps tenodesis can be associated with fracture when using an interference screw and can also cause neurovascular injury in the subpectoralis region due to association with brachial plexus palsy and musculocutaneous nerve injury[117-119].From these studies, no difference in outcomes can be found between open and arthroscopic biceps tenodesis.




Imaging and diagnostic injections
Supporters of the interference screw technique argue that it creates more surface area contact between the tendon and cancellous bone and thus results in greater exposure to marrow-derived endogenous stem cells[150-153].However, this comes at a cost, as securing the tendon within a bone socket can result in local deformations in the tendon[140,154].In Tan[150], researchers used a rabbit model of bicep tenodesis and compared tendon healing within the bone socket to healing on the cortical surface.Histologic analysis showed similar healing profiles between the two groups which allowed authors to conclude that the creation of large bone sockets with interference screws, which can lead to increased fracture risk, may be unnecessary.Furthermore, the interference screw technique has been associated with additional complications such as persistent pain and bioabsorbable screw reactions[119,155,156].
Diagnostic injections could also be utilized in patients with anterior shoulder pain as peritendinous or sheath injections are often used to clinically diagnose and treat biceps tendinopathy[75,76].Injections into the tendon sheath can be diagnostic and therapeutic by providing the physician information about the patient’s pathology based on their pain response post-treatment[77,78].It is important to note that injections should not be directly inserted into tendons as it can lead to tendon rupture[79].Improved injection accuracy through ultrasound guidance has proven to be effective compared to blind injection techniques.In a recent study by Hashiuchi[80], ultrasound-guided injections resulted in 87% accuracy while blind injections were accurate only 27% of the time.
Nonsurgical management of LHBT disorders is largely driven by individual surgeon experience.Typically, management begins with nonsteroidal anti-inflammatory drugs, physical activity, activity modifications, and ultrasound-guided corticosteroid injections into the biceps sheath[56,80,81].Although physical therapy improves overall shoulder strength, range of motion, and function, limited research has been done that analyzes the outcomes of physical therapy as a nonoperative management option for LHBT pathologies.As mentioned earlier, the corticosteroid injection should be carefully placed as accidentally guiding the injection into the biceps tendon may cause rupture[82].If correctly placed, ultrasound-guided corticosteroid injections have shown to cause lower patient discomfort as well as superior accuracy compared to palpated and blind injections[83].Unfortunately, corticosteroid injections were found only to be beneficial in the short term, but may be worse than other treatment options in the intermediate and long terms[84].Regardless of technique, research on the effectiveness of corticosteroid injections is inconclusive[85].
TREATMENT OPTIONS
The treatment of LHBT pathology can be separated into nonsurgical and surgical management.Initially, LHBT injuries should be treated conservatively followed by surgery when all conservative treatments fail.
Nonsurgical management
Having travelled from land to land in this fashion without finding anything to rivet10 his attention, it occurred to him to take the form of an eagle, and in this shape he flew across many countries and arrived at length in a new and lovely spot, where the air seemed filled with the scent11 of jessamine and orange flowers with which the ground was thickly planted
Other options for nonsurgical management include iontophoresis, phonophoresis, ultrasonography, extracorporeal shock wave therapy, and laser therapy.Unfortunately, these have shown conflicting results in the literature[86,87].Furthermore, promising yet inconclusive clinical outcomes have been shown for treatment options such as regenerative injection therapy which includes platelet-rich plasma[88,89].If all nonsurgical treatment options fail, then patients should consider surgical treatment options.
Surgical management
The two types of fixations that can be used in intra-articular, suprapectoral, and subpectoral approaches include inlay and onlay.With inlay fixation, the biceps tendon is inserted perpendicularly into the bicipital groove.This technique is less technically challenging to perform, but can result in tenodesis failure in patients with poor tendon quality or osteoporosis at the screw insertion site[133,134].For the onlay technique, the biceps tendon lays parallel to the bicipital groove.Onlay fixation with a suture anchor may be technically challenging and require longer operative times, but may have superior clinical and functional outcomes compared to the inlay technique[135,136].
Biceps tenotomy is a viable option to surgically manage LHBT pathology and involves cutting the LHBT at its origin and maintaining the integrity of the labrum (Table 1)[49].While numerous studies have shown excellent outcomes, pain relief, and improved patient-reported outcomes in individuals who undergo biceps tenotomy, there are a few complications shown in Table 1[46,90-92].Other cited complications include stiffness, infection, transient nerve injuries, complex regional pain syndrome, and stroke secondary to cerebral hypoperfusion[93].In recent studies, surgeons have tried to address some of these complications by testing arthroscopic techniques to limit distal migration of the LHB after tenotomy to minimize and even eliminate the occurrence of the Popeye deformity[94-97].Other studies have reported ways to improve the efficiency of arthroscopic biceps tenotomy by using a biceps squeeze maneuver[98].This is a simple method that entails manually squeezing the biceps muscle belly while performing the arthroscopic biceps tenotomy in order to shorten and tension the intra-articular portion of the tendon.In doing so, this technique improves the efficiency and safety of the procedure without adding additional cost.
Biceps tenodesis is increasingly used to treat individuals with LHBT pathology (Table 1).It involves releasing the LHBT from its origin and attaching it at one of four locations: (1) Within the glenohumeral joint to the intact rotator cuff; (2) To the conjoint tendon or the transverse humeral ligament; (3) Proximal to or within the bicipital groove in a suprapectoral fashion; or (4) Distally in a subpectoral fashion (mini-open approach)[6].Current areas of debate include whether orthopaedic surgeons should perform biceps tenodesis open or arthroscopically, the best method of fixation (interference screw, suture anchor, or cortical button), and the ideal location of tenodesis (intra-articular, suprapectoral, subpectoral, and other positions such as extra-articular top of groove or extra-articular bottom of groove)[99].
I stretched myself cosily upon the soft grass, and with the bundle of hemp for a pillow slept as tranquilly as if there were no such things as sheep in the world, while they for their part wandered hither and thither119 at their own sweet will, as if there were no such thing as a shepherdess, invading every field, and browsing120 upon every kind of forbidden dainty, until the peasants, alarmed by the havoc121 they were making, raised a clamour, which at last reached the ears of the King and Queen, who ran out, and seeing the cause of the commotion122, hastily collected their flock
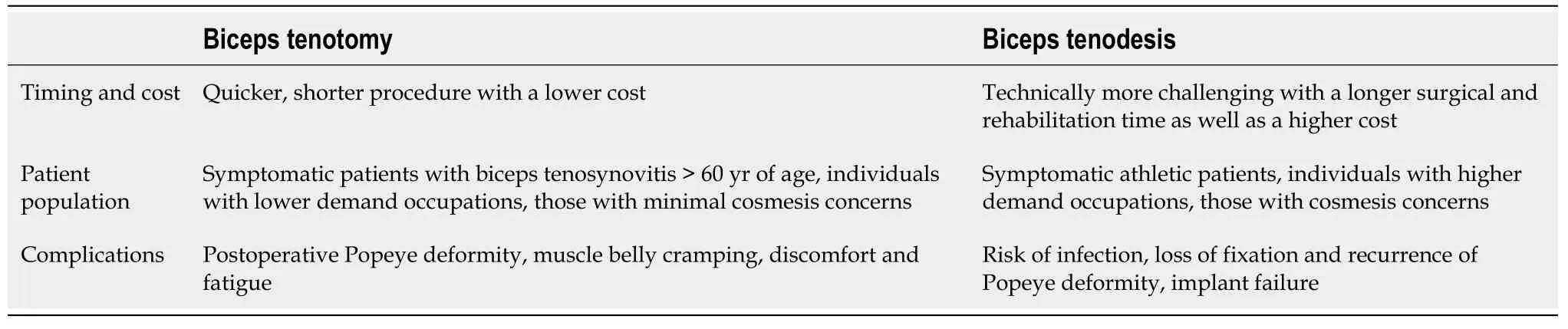
Open arthroscopic:Biceps tenodesis can be performedan open or arthroscopic approach; both methods have excellent clinical outcomes[100,101].While a comparison between approaches is difficult due to concomitant pathology and different types of fixation, a comparison highlighting timing and cost, functional outcomes, range of motion, and complications can be seen in Table 2[102-105].With no consensus over which method is superior, surgeons should take into account their own preference and technical experience when deciding on the proper approach for their patients.
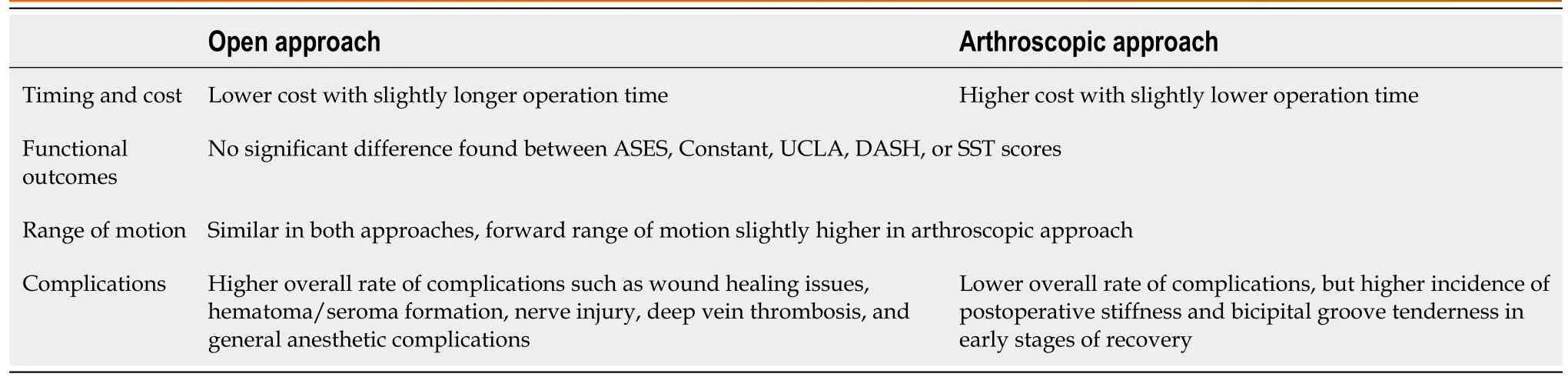
A number of studies have analyzed open biceps tenodesis procedures in patients without rotator cuff tears and demonstrated improved patient reported outcome measures as well as pain and functional outcome scores[106-110].Even though fewer studies have been identified for arthroscopic biceps tenodesis procedures in isolated LHB pathology, the patient reported outcome measures, pain scores, and objective outcomes are satisfactory in 98%-99% of patients with low rates of revision (0.4%) for biceps related problems[111-113].
While specific examinations in patients with biceps-related pathology and SLAP tears can be utilized to differentiate etiologies of shoulder pain, these maneuvers often lack specificity[51,52].For example, the Speed test, which is used to elicit anterior shoulder pain with resisted elbow flexion has overall sensitivity of 57% and specificity of 52% in diagnosing biceps tendon disorders and SLAP lesions (Figure 6)[47,52-55].Similarly, the Yergason test, which is used to elicit anterior shoulder pain with resisted forearm supination, has been shown to be an unreliable predictor of biceps pathology or SLAP tears with a reported sensitivity of 43% and specificity of 79%[54-56].Physical examination maneuvers specific for SLAP pathology, such as the O’Brien active compression test and the O’Driscoll dynamic labral shear test, have demonstrated reasonable diagnostic utility, but are still controversial (Figure 7)[57].While some studies initially reported excellent results for the diagnostic utility of the O’Brien active compression test, recent meta-analyses have suggested that it is not diagnostic of SLAP tears[58,59].The O’Driscoll dynamic labral shear test was also found to have excellent initial results in terms of diagnostic utility for SLAP tears, but was questioned by further studies[60-62].Furthermore, examination maneuvers for SLAP pathology are limited by shoulder pathology that is often observed in individuals with SLAP tears, such as Bankart lesions and partial-thickness rotator cuff tears[63-65].
Biceps tenodesis is mainly done with intra-articular, suprapectoral, or subpectoral placement; other possible positions include extraarticular top of the groove and extra-articular bottom of the groove placement.In the intra-articular approach, the LHBT is cut and reattached within the intertubercular groove.While the clinical outcomes of this approach are excellent, patients may have persistent bicipital groove pain and tendinopathy with a portion of the tendon within the bicipital groove[120,121].In the suprapectoral approach, the LHBT is cut and reattached distally to the bicipital groove and proximally the pectoralis major tendon.Even though this approach avoids the inflammation from the tendon remaining in the bicipital groove and sheath, it may be a longer and thus more costly approach compared to the subpectoral method and has thinner bone stock for hardware fixation[120,122,123].Furthermore, in intra-articular and suprapectoral approaches, residual pain has been described[100,124].
Vasilissa was so frightened to see how the old witch ground her teeth that she almost told her of the little doll; but she bethought herself just in time, and answered: The blessing of my dead mother helps me.
In patients with significant inflammation in the biceps groove or patients where the suprapectoral part of the biceps is of poor quality or significantly injured, the subpectoral approach is the preferred method[125].Subpectoral tenodesis is advantageous because it eliminates the pain created from reattachment within the groove, it is associated with stronger bone for fixation in the humerus, and it can potentially lead to a quicker recovery[126-128].Like the other approaches, the subpectoral method has its disadvantages.The main disadvantages include scar formation, elongation of the biceps, biceps asymmetry, and partial detaching and reattaching of the pectoralis major to the humerus[126,128,129].Compared to the suprapectoral approach, thesubpectoral approach has more residual tenderness and spasm initially following the procedure[120].Furthermore, fracture has been described as a complication particularly with the use of interference screws[130,131].
For a moment he was stunned12 into silence by this new learning. Finally he said quietly, I never realized that,Amy. You re in a wheelchair all the time — I never thought you d mind sitting in the boat. It s the same thing.
Really her one idea was to let the Princess be seen by as few people as possible; so, throwing a veil over her head, she led her away and locked her up securely
In a study by Godshaw[121], authors compared forty-three patients who had undergone intra-articular tenodesis to fifty-six patients who had undergone suprapectoral tenodesis.While both groups showed improvement in all outcome measures, there was no difference between the groups in functional outcomes for physical and mental component scores as well as ASES scores.Werner[128] compared arthroscopic suprapectoral biceps tenodesis in nine cadavers to open subpectoral biceps tenodesis in nine cadavers.They found that the arthroscopic suprapectoral biceps tenodesis group had a significantly decreased load to failure compared to the open subpectoral biceps tenodesis group.Additionally, the arthroscopic suprapectoral technique over-tensioned the biceps tendon.Despite these findings, other individuals did not know if there would be similar results in live patients.To further test this idea, Werner[132] compared thirty-two patients who underwent arthroscopic suprapectoral biceps tenodesis to fifty patients who underwent open subpectoral biceps tenodesis patients.There was no significant difference reported in Constant, ASES, Single Assessment Numeric Evaluation, Simple Shoulder Test (SST), LHB, and Veterans RAND 36-Item Health Survey scores.Furthermore, there were no range of motion or strength deficits in either group.These studies prove that regardless of associated complications for intra-articular, suprapectoral, and subpectoral biceps tenodesis placement, all three approaches have excellent and similar clinical outcomes.
While surgical management of LHBT pathologies is reserved for individuals who have failed all previously performed nonsurgical treatment options or individuals with acute injuries, the optimal surgical treatment is still up for debate[17].The three options include biceps tenotomy, biceps tenodesis, and SLAP repair.
Within inlay and onlay strategies, the different fixation techniques include interference screw and suture anchor, which are the most common, as well as cortical button and all-suture suture anchor constructs.Arthroscopic intra-articular biceps tenodesis has historically utilized an inlay technique in which the tendon is docked into a bone socket perpendicular to the bicipital groove and secured with an interference screw[113,137].In open subpectoral tenodesis, the onlay technique is used with a suture anchor meant to heal the tendon to the cortical surface of the humerus[138-141].
The various types of interference screws include titanium, polyether ether ketone (PEEK), and bioresorbable screws.Titanium interference screws are infrequently used as they have an increased risk of tendon laceration during screw insertion and can make postoperative assessment challenging due to significant artifact on MRI[142,143].PEEK interference screws have become more popular for several reasons: (1) They are chemically inert and insoluble; (2) They have a modulus of elasticity similar to human cortical bone; and (3) They are compatible with MRI and have a higher resistance to radiation[144,145].Suture anchors require a smaller bone socket compared to interference screws and as previously mentioned secure the tendon to the humeral cortex.Furthermore, all-suture suture anchors allow for even less violation of the cortex.
While all constructs have been studied and proven to be effective, there is no consensus on which fixation strategy provides the most superior fixation[141,146-148].In a study by Buchholz[147], researchers compared intramedullary cortical button fixation to interference screw usage and found similar results in regard to stiffness and ultimate failure loads.In Chiang[149], interference screws and all-suture suture anchors were found to have similar failure loads and stiffness which correlates to an increased likelihood of tenodesis failure.Likewise, Tashjian[141] found failure loads to be similar when comparing interference screws to dual-anchor all-suture suture anchors.Despite these results, additional studies have concluded contrary findings.In Richards[148], authors analyzed eleven cadaveric humerus specimens in which biceps tenodesis was performed with interference screw fixation or double suture anchor fixation.Authors reported consistent failure at the anchor or anchor eyelet in the suture anchor cadaver models and concluded that interference screw fixation had superior fixation strength.On the other hand, Golish[133] found interference screws to have a higher failure load and stiffness compared to all-suture suture anchors.With mixed results from these studies, there is no consensus on which fixation strategy provides the greatest advantage.
With the lack of specificity in physical examination maneuvers, imaging studies are often used to differentiate LHBT pathology.Unfortunately, this too has its faults.While radiographs can be useful in assessing bony anomalies and ruling out concomitant osseous disorders, they often appear normal[7,52].Advanced imaging studies such as MRI demonstrate reasonable sensitivity and specificity for the diagnosis of SLAP tears, LHBT rupture, and other inside lesions of the BLC; however, junctional and bicipital tunnel lesions are poorly identified[66-70].Additionally, ultrasonography is a fast, cost-effective, and radiation-free diagnostic method for shoulder and has been used for LHBT instability, dynamic examination of the tendon, examination of hypoechogenic areas, and increased tendon diameter[71,72].While ultrasound techniques are useful in detecting LHBT pathology with a sensitivity between 50%-96% and a sensitivity of 98%-100%, it is less helpful in diagnosing partial-thickness tears[71,73,74].Regardless of its faults, ultrasonography techniques should be used in conjunction with MRI when examining LHBT pathology.
In contrast, all-suture suture anchors provide the benefits of conventional interference screws while being less traumatic to the bone and thus having a lower risk of fracture[157,158].Frank[157] compared torsional energy in humeri that underwent biceps tenodesis with all-suture suture anchors to humeri that underwent biceps tenodesis with interference screws.They found that humeri in the all-suture suture anchor group required greater torsional energy to fracture suggesting that this construct creates less of a stress riser than the interference screw construct.
Although many studies have compared the biomechanical qualities of these constructs, few have compared differences in clinical outcomes.Park[140] compared clinical and anatomic outcomes of the interference screw and suture anchor fixation techniques for biceps tenodesis and found that both methods improved functional outcomes.Additionally, there was no difference in patient-reported outcomes measured by the visual analog scale (VAS) for pain, ASES score, SST, Constant score, Korean shoulder score, and LHB score between the two groups.With that said, the authors did find interference screw fixation and more physically demanding work levels to be associated with tenodesis failure.In another study by Millett[159], no statistically significant differences were reported at thirteen months postoperatively in VAS, ASES, and modified Constant scores between individuals who underwent biceps tenodesis with interference screw fixation and individuals who underwent biceps tenodesis with all-suture suture anchor fixation.
From the various biomechanical studies described above, the decision on which fixation strategy to utilize can be rather nuanced.While some studies have cited no differences in regards to stiffness or ultimate failure load between fixation strategies, other studies have contradicted these findings declaring interference screw fixation as more superior in terms of fixation strength and more inferior in regards to failure load and stiffness[133,141,147-149].Despite the lack of consensus amongst the ideal fixation technique regarding biomechanical data, there appears to be no difference between fixation techniques in terms of clinical outcomes.
Biceps tenotomy biceps tenodesis: Several studies have investigated the differences between biceps tenotomy and biceps tenodesis, but mainly for LHB tendinopathy with rotator cuff tears, which makes it difficult to determine the extent to which biceps management influences outcomes[160-162].A comparison of the techniques can be found in Table 1.In a systematic review by Leroux[160], authors analyzed patients who underwent rotator cuff repair in combination with either biceps tenotomy or biceps tenodesis.They reported that patients who underwent biceps tenodesis had better Constant assessment scores (92.8 [tenodesis]90.6 [tenotomy],< 0.01) and decreased rates of biceps deformity compared to patients who underwent biceps tenotomy (3.8% [tenodesis]15.5% [tenotomy],< 0.01).
Another study compared the clinical results of biceps tenotomy and biceps tenodesis based on technique.In Shank[163], seventeen patients underwent biceps tenotomy, nineteen patients underwent suprapectoral biceps tenodesis with a doubleloaded anchor fixation, and thirty-one control patients did not have any biceps surgery performed.Analysis showed no significant difference in either forearm supination nor elbow flexion strength among patients in all three groups.
One theory that has been challenged recently is the duration of postoperative rehabilitation.Zabrzyński[164] attempted to test different rehabilitation protocols in tenotomytenodesis groups with the tenotomy group undergoing a personalized postoperative rehabilitation protocol.They found that patients who underwent tenotomy with a shortened postoperative rehabilitation protocol were able to achieve better clinical outcomes and ensure faster return to sports activity compared to those who underwent tenodesis[164].
The results described above demonstrate how challenging it can be to make direct comparisons between tenotomy and tenodesis in hopes of determining which is superior.Furthermore, the concern for cosmesis plays a role in determining whether a patient should undergo tenotomy or tenodesis.Typically, tenotomy is indicated in older patients as cosmesis is of minimal concern whereas tenodesis is indicated in younger more active patients where cosmesis tends to play a more significant role.Recent systematic reviews and meta-analyses by MacDonald[165], Zhou[166], and Kooistra[167] confirm the findings that there is no evidence-based difference in LHB tenodesistenotomy when evaluating shoulder function, pain, or biceps-related strength.
Soon after he died the king set forth1 a proclamation through the whole country that whoever could build a ship that should float both on land and sea should have his daughter to wife
Treatment recommendations for SLAP lesions are based on patient age as well as activity level and include nonsurgical management, arthroscopic debridement, arthroscopic repair, and biceps tenodesis.Over the last five years, orthopaedic literature has documented the growing trend to move away from SLAP repair due to an increased incidence of subsequent revision surgery[168,169].Instead, literature has shown an increase in the frequency of biceps tenodesis, particularly in patients over the age of forty and athletes as return to activity after biceps tenodesis was significantly higher than the rate after revision SLAP repair[170,171].
SLAP tears are often categorized into Type I through Type X[172].In a type II SLAP lesion, there is detachment of the superior labrum and the origin of the LHBT insertion from the glenoid[173,174].Surgical techniques that can be used to repair a standard type II SLAP lesion include the use of a single suture anchor placed posterior to the biceps anchor or the use of two suture anchors with one suture anchor placed anterior and the other placed posterior to the biceps anchor[17].A few studies have reported on outcomes regarding type II SLAP repair.Saydeincluded 506 patients who underwent repair of type II SLAP tear and reported excellent satisfaction in 83% of patients and return to previous level of play in 73% of patients; however, in the 198 patients who were overhead athletes, inferior outcomes were reported with only 63% able to return to previous level of play.Similar studies have assessed the outcomes of overhead athletes who have undergone arthroscopic SLAP lesion repair and report a return to preinjury level of sports activity between 22% and 85%[175-178].In Frank[179], sixty-two patients underwent arthroscopic repair of a type II SLAP tear.Authors reported that patients aged twenty years and younger as well as overhead throwers were more likely to require revision surgery than patients greater than twenty years of age and non-overhead throwers.Furthermore, they concluded that patients greater than forty years of age were more likely to have inferior postoperative ASES scores compared to patients aged less than forty years of age.
An increasingly popular alternative to arthroscopic repair of SLAP lesions is biceps tenodesis as it has a significantly higher rate of return to activity following surgery[170,171].Some studies have performed biceps tenodesis in combination with SLAP repair or performed biceps tenodesis in place of SLAP repair.For example, Boileau[1] compared ten patients with an isolated type II SLAP lesion who underwent repair with the use of suture anchors to fifteen patients with an isolated type II SLAP lesion who underwent arthroscopic biceps tenodesis with the use of an absorbable interference screw.Patients in the SLAP repair group had inferior outcomes including lower mean Constant assessment scores, lower satisfaction, and lower return to previous level of sports activity.On the other hand, some studies have reported similar outcomes in patients with a type II SLAP tear who undergo biceps tenodesis.In Denard[2], thirty-seven patients greater than thirty-five years of age with an isolated type II SLAP tear underwent arthroscopic biceps tenodesis or SLAP repair.Authors demonstrated that patients in the biceps tenodesis group had shorter postoperative recovery, higher satisfaction rates, and higher rates of return to normal activity.Similarly, Ek[3] compared twenty-five patients with an isolated type II SLAP lesion who underwent biceps tenodesis or SLAP repair and found that both groups had improved clinical outcomes with low failure rates and similar rates of return to sports.These studies demonstrate that patients who undergo biceps tenodesis for SLAP lesions experience a shorter postoperative recovery time, higher Constant assessment scores, higher satisfaction rates, higher rates of return to normal sports activity, and lower failure rates compared to patients who undergo SLAP repair.
While type II SLAP tears have seen an increase in biceps tenodesis as treatment, type III and type IV SLAP tears can be adequately treated with SLAP repair depending on the extent of the injury[172].In a type III SLAP tear, a bucket-handle tear of the superior labrum occurs with potential displacement of the mobile labral fragment into the glenohumeral joint.In this case, the attachment of LHBT remains intact.Typically, type III SLAP lesions require resection of the unstable bucket-handle fragment with no further stabilization of the biceps anchor[172,180].Some authors have also recommended refixation of the torn flap analogous to meniscal tears if the lesion is caused by trauma and located within a specific part of the shoulder[181].For a type IV SLAP tear, there is a bucket-handle tear of the superior labrum that extends to the biceps tendon in a variable degree.Type IV SLAP lesion repair is reliant on biceps tendon stability after resection of the torn flap as at least half of the tendon should be intact to preserve stability of the labro-bicipital complex[172].In an unstable biceps tendon where more than 50% of the tendon is affected, a tenotomy or tenodesis is preferred over a SLAP repair.With SLAP repairs demonstrating a wide variability in outcomes, specifically in rates of return to play and failure rates for older individuals, biceps tenodesis has shown a significant improvement in ASES scores and VAS scores[182].
Vingo sat there stunned10, looking at the oak tree. It was covered with yellow handkerchiefs. 20 of them, 30 of them, maybe hundreds, a tree that stood like a banner of welcome billowing in the wind. As the young people shouted, the old con rose and made his way to the front of the bus to go home.
The excellent outcomes and low rate of complications of biceps tenodesis for SLAP lesions have led to an increase in frequency of biceps tenodesis[119,183].In a study by Patterson[4], trends in the management of SLAP lesions were reviewed and the proportion of SLAP repairs between 2002 and 2011 decreased from 69.3% to 44.8%, whereas the proportion of biceps tenodesis procedures increased from 1.9% to 18.8%.Furthermore, the proportion of SLAP repairs used to manage SLAP lesions in combination with rotator cuff repair decreased from 60.2% to 15.3%, whereas the proportion of biceps tenodesis or tenotomy procedures increased from 6% to 28%.In a more recent study by Cvetanovich[171], there was a 69.3% decrease in isolated SLAP repair from 2007 to 2016 and an increase of 370% in biceps tenodesis for the diagnosis of an isolated SLAP tear over the same period.With this knowledge, Chalmers[184] conducted a study with three groups: (1) Forty-five patients with a SLAP tear who underwent isolated SLAP repair; (2) Twenty-three patients with a SLAP tear who underwent isolated biceps tenodesis; and (3) Eighteen patients with a SLAP tear who underwent SLAP repair in combination with biceps tenodesis.Authors reported substantially worse postoperative ASES scores and visual analog scale pain scores in patients who underwent SLAP repair in combination with biceps tenodesis compared to either of the other categories.These studies demonstrate the utility and improved clinical outcomes in patients with SLAP lesions who undergo biceps tenodesis compared to patients with SLAP lesions who undergo arthroscopic repair.Furthermore, improved outcomes seen in biceps tenodesis for SLAP tears is supported by the increase in volume of biceps tenodesis procedures over the last five years or so.
CONCLUSION
LHBT is a common source of disease and shoulder pain with etiologies including inflammation, instability, and trauma.Although the anatomy can be easily digested, the decision to operate is a little more nuanced.Despite various physical examination maneuvers, the lack of specificity requires orthopaedic surgeons to rely on patient history as well as advanced imaging in order to best manage the patient’s condition.Nonsurgical treatment typically includes physical therapy, anti-inflammatory medications, and ultrasound-guided corticosteroid injections.If nonsurgical treatment fails, surgical techniques such as biceps tenotomy, biceps tenodesis, or SLAP repair can be used.In biceps tenodesis, differences between arthroscopic and open biceps tenodesis, type of fixation system, and location of tenodesis should be discussed with patients keeping in mind that no functional differences have been established.Furthermore, SLAP lesions can be treated with SLAP repair or biceps tenodesis depending on the categorization.While debridement has been used as the standard of treatment in the past for SLAP lesions, the increase in volume of biceps tenodesis for SLAP lesions indicates a transition to a treatment option with better functional and clinical outcomes.
 World Journal of Orthopedics2022年1期
World Journal of Orthopedics2022年1期
- World Journal of Orthopedics的其它文章
- Three-dimensional printing in paediatric orthopaedic surgery
- Regional anesthesia for orthopedic procedures: What orthopedic surgeons need to know
- Should we use similar perioperative protocols in patients undergoing unilateral and bilateral one-stage total knee arthroplasty?
- Epidemiology and incidence of paediatric orthopaedic trauma workload during the COVID-19 pandemic: A multicenter cohort study of 3171 patients
- Can bedside needle arthroscopy of the ankle be an accurate option for intra-articular delivery of injectable agents?
- High-resolution, three-dimensional magnetic resonance imaging axial load dynamic study improves diagnostics of the lumbar spine in clinical practice
