Three-dimensional printing in paediatric orthopaedic surgery
INTRODUCTION
Over the last decade, three-dimensional (3D) printing–or additive/layer manufacturing-has become a more and more interesting application in medicine.It has been used in various surgical specialties, including neurosurgery, oral and maxillofacial surgery, plastic surgery and cardiothoracic surgery[1-3].Also in the field of orthopaedic surgery the interest and use of 3D printing has grown over the years, since it started in 1999 in a case of complex spinal surgery[4].
In the orthopaedic field, 3D technology can be used in three different sections: Including preoperative planning, 3D-printed models and 3D printing for patientspecific instrumentation (PSI).A recent meta-analysis reported that the use of 3Dprinted models in preoperative planning significantly reduced the operative time, intraoperative blood loss and fluoroscopy use during orthopedic trauma surgery[5].These outcomes may be the result of a better understanding of the pathological anatomy in complex cases.Moreover, 3D printing helps the surgeon in preoperative planning of the surgical procedure by means of fracture reduction and the sizes and positioning of plates and screws for internal fixation.This could possibly reduce operation time and the amount of dissection of surrounding tissues and therefore blood loss[5].In addition to trauma surgical applications, PSI allows the surgeon to perform precise osteotomies for deformity correction[5-8], which is specifically interesting for paediatric patients[9].
I think he is not in his right senses! said the Princess, and walked on, butwhen she had gone a little way, she stopped again. One must encourage art, said she, I am the Emperor s daughter. Tell him he shall, as on yesterday,have ten kisses from me, and may take the rest from the ladies of the court.
Correcting limb deformities in children is a challenging and complex type of surgery.Therefore, novel technologies such as 3D printing are increasingly applied, aiming to achieve more accurate corrections and improved outcomes[9].The use of patient-specific 3D-printed models is specifically interesting and promising in paediatric orthopaedic surgery, as limb deformity corrections require [sh6] an individual 3D treatment.For example, the use of 3D printing in preoperative planning of hip preservation surgery created an improvement in trainee and patient education for understanding the abnormality of the patient’s disorder[6].However, due to its novelty, evidence on the use of 3D printing in pediatric orthopedics is still limited.
This editorial provides an overview of the various intraoperative applications of 3D printing in pediatric orthopedic surgery and assesses the overall role, challenges and future of this relatively novel technique.
Although the production time of a 3D product has decreased since it was invented, preparation and production of PSI still take at least several days[32].Therefore, the application in the acute setting is challenging (, for fractures).However, research and development in 3D printing is a growing field of interest, resulting in new upcoming materials with better biomechanical and biocompatible characteristics.Furthermore, the development of 3D printers that can create models within hours is very promising.
TECHNICAL ASPECTS OF 3D PRINTING
Intraoperative applications of 3D printing in pediatric orthopedics involve the creation of PSI to perform more accurate complex surgery or correct deformities.There are increasingly interesting and promising applications in both upper limb and lower limb deformities.
The process of creating 3D-printed models for medical applications starts with highresolution imaging (Figure 1)[7,8,10-12].Multi-row detecting computed tomography (MDCT) and magnetic resonance imaging (MRI) are frequently used in orthopedics for diagnostics of complex anatomy or severe deformities[7,11-13].MDCT is a highcontrast computed tomography (CT) that produces thin-section slices of less than 1 mm and therefore highly suitable for analysing bony structures.After acquiring the clinical dataset, MDCT images are stored according to a universal data format; standardized digital imaging and communications in medicine (DICOM).Postprocessing software extracts these DICOM files[7,8,14].This extraction process is called segmentation.It separates the outlines of different anatomical structures in each individual 2D image (slice) by using colour contrast to create separate objects.In the next phase, computer-aided design (CAD) software (, MIMICS or InPrint) combines all the individual 2D images (slices) and creates a virtual 3D initial object (Mesh creation)[7,8,10,14].This makes it possible to see depth, angulation and diameters of the anatomical structure or pathology.Next, the 3D object is transformed into a file that is ready for printing.In some cases, the resolution of the radiology is suboptimal, or the 3D object has no clear boundaries.In these cases, a manual reconstruction of a 3D object can be performed (ReplicatorG software) and anatomical corrections of the model can be made in this CAD software[7,8,14].It also provides control of the filling of the model, with possibilities between 0% filling (shell alone) to 100% filling and makes the model more suitable for 3D printing or material of preference[7,8,10,14].Once the CAD model is finalised, it is converted into a common 3D file format, stereolithography (SLA) file and sent to the appropriate 3D printer[2,7,8,14].Post process, the materials first need to cool down before they can be used and consequently sterilization is required for intraoperative use[12].

Different types of 3D printing techniques have been used over the last years, including printers that use powder, melted polymers, gel, liquids, or a combination of these substances[7,8].In the past, Fused Deposition Modeling (FDM) was used as a 3D printing technique, in which a movable nozzle places long, thin wire of thermoplastic material on top of each other.A 3D object is created layer by layer.It is a relatively cheap and fast production method to create anatomical models.However, the shape of a FDM print differs greatly in quality from a professional 3D printer[7,8,15,16].Therefore, different 3D printing procedures are used for the production of patientspecific models and patient-specific surgical guides at this moment.Selective laser sintering (SLS) is a powder-based fusion technology that uses a laser beam to locally sinter polymer powder to build 3D objects layer by layer[7,8,15,16].SLS uses bio-based polyamide materials and metals for 3D printing.Other 3D printing techniques are SLA and digital light processing (DLP) that use UV laser and a liquid bath containing a UVsensitive liquid polymer[8,10,12,17].This liquid is illuminated layer by layer by the laser where the liquid has to cure.The surface cures into a solid state and subsequently the surface raises one layer.The next layer is then exposed and cured.3D-printed objects that are generated SLS, DLP and SLA can be sterilized and therefore can be used in the operating room.
INTRAOPERATIVE APPLICATIONS OF 3D PRINTING IN PEDIATRIC ORTHOPEDIC SURGERY
3D printing, or additive layer manufacturing, is a technique to create a 3D object from a digital model.It is an advanced, computer-controlled technology that deposits successive layers of materials (, metals or plastic) to create an object.In contrast to traditional subtractive manufacturing processes that take away or shape material, 3D printing has the advantage to create complex structures by adding hundreds of miniscule layers that are fused together.Another advantage of 3D printing is the possibility to create shapes of different materials including plastic, rubber, metals or ceramics[7,10].
Upper limb
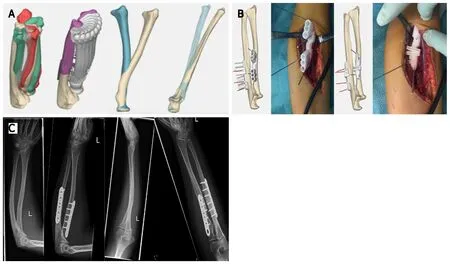
Currently, the most commonly described application of 3D printing in the upper extremity is the forearm, usually rotational impairment after malunited forearm fractures.Byrne[18] used 3D-printed patient-specific osteotomy guides and custom-made plates for multiplanar corrective osteotomies in 5 patients with posttraumatic malunion of the forearm.An angular correction of the ulna and radius of 9.9° and 10.0° was planned, respectively.They reported mean postoperative corrections of 10.1° and 10.8°, respectively.Forearm pronation improved from 68° to 87° and supination improved from 47° to 89°.Furthermore, a significant improvement in pain relief and grip strength was seen.Another prospective study enrolled 16 patients with a total of 17 bone deformities, including distal radial malunion, distal humeral malunion and forearm diaphyseal malunion[19].They reported that the use of 3D patient-matched instruments for corrective osteotomies showed a significant deformity improvement of 22.2°.Also, in patients treated for distal radial malunion and diaphyseal malunion, the flexion, extension and pronation of the forearm were significantly improved.Clinical implications as pain, range of motion, and grip strength were also significantly improved compared to the preoperative situation.Another study used 3D-printed templates to guide the osteotomy orientation in a posttraumatic forearm malunion of a 15-year-old female[3].The authors reported that 3D-printed templates made it possible to achieve near-anatomical reduction close to 1° residual deformity in all three planes and a recovery to full function within 3 mo.One of our own cases presented with decreased rotational range of motion after sustaining a forearm fracture as a child, without improvement after extensive rehabilitation.3D analysis determined the deformity and optimal planes of correction (Figure 2).Patientspecific osteotomy guides with predrilling of the screw holes were designed, and hardware for fixation was selected (Figure 2).The surgical procedure was then completed according to plan, which resulted in a vast improvement in range of motion and high patient satisfaction.In the period 2014-2020, 42 cases were operated using this technique, of which 16 were malunited forearms with rotational impairment.Most patients had a severe supination deficit (mean -10 degrees), which improved to a mean supination of +60 degrees.Pronation limitation was much less severe (mean +45 degrees) with a mean improvement to +55 degrees.We experienced one complication due to a transient posterior interosseous nerve paralysis, which recovered spontaneously within the first 6 wk after surgery.Thus, in deformities of the forearm due to malunion, the use of 3D PSI shows improvement in correction angles as well as in clinical outcomes as grip strength and pain relief[1,18,19].Nevertheless, it is important to realize that the studies mentioned above are low-grade evidence and therefore the results need to be analysed with a critical view.
For lower limb paediatrics, 3D printing has been used for various complex techniques, including femoral and pelvic osteotomies and tarsal coalition resection[15,22].Femoral and pelvic osteotomies with use of 3D guides have been applied for late sequelae of developmental dysplasia of the hip (DDH), slipped capital femoral epiphysis (SCFE) and Legg-Calvé-Parthes (LCP) disease[15].
Lower limb
Cubitus varus deformities are sometimes seen after elbow fractures in children.Correction of this deformity is a complex surgical procedure and requires a 3D approach.Hu[20] included 35 patients and assigned them into two different groups comparing traditional surgery to surgery using an intraoperative patientspecific 3D-printed navigation template.All patients underwent similar surgery with wedge osteotomy of the lateral distal humerus.The 3D-printed patient-specific template significantly reduced the operation time with a mean of 11 min and significantly improves the accuracy of the correction by a mean of 3°.However, the question remains whether and accuracy of 3° is clinically relevant.Another study analysed 25 patients with cubitus varus deformity and compared a group of patientspecific 3D-printed osteotomy guides with a traditional group[21].The 3D guiding template procedure resulted in a significant decrease of the operation time (almost 30 min), less intraoperative blood loss (17.5 mL) and higher satisfaction.However, the most important achievement of correcting deformities in pediatric orthopedics is recovery of function.
A recent review confirmed that use of PSI for the above indications has led to improved accuracy and precision, decreased procedure times, and decreased intraoperative imaging requirements, compared to conventional methods of performing femoral or pelvic osteotomy[15].
SCFE leads to a posterior and inferior displacement of the femoral head, giving an altered mobility of the hip joint and a syphon-shaped femoral neck after consolidation.A 3D sub- or intertrochanteric osteotomy can be performed for correction of the varus, internal rotation and flexion of the hip and thereby restoring its function.Cherkasskiy[24] used 3D models for proximal femoral osteotomy following SCFE and also found decreased operation and fluoroscopy times.We have used a CT-based 3Dprinted model to plan and perform a complex osteotomy in a previously pinned SCFE case, with favourable results with regard to osteotomy precision, positioning of the implant, surgical time and use of the image intensifier (Figure 3).In this case the patient had a pre-operative externally rotated right hip of 40 degrees.Post-operatively,she was able to internally rotate the hip 10 degrees, compared to 20 degrees of internal rotation on the contralateral left side (Figure 3).
LCP disease can lead to deformity of the femoral head and an adaptive deformity of the acetabulum.Six patients with LCP disease were treated with a 3D-printed patientspecific osteotomy model[25].The model allowed the surgeon to correct the femoral head almost identical to the contralateral healthy side[25].
Just at this time the Fairy of the Beech-Woods received a visit from an old friend of hers called Saradine, who rushed into her house so breathless with rage that she could hardly speak
2. Little Red Riding Hood: The red riding hood is a popular and familiar symbol to much of Europe and North America. In the height of portraiture11 in the nineteenth century, many young daughters of wealthy families were painted wearing red capes12 or hoods13. Today, some little girls still want to wear red capes for Halloween or other imaginative play.
Severe DDH can lead to hip deformity that may require surgical correction.Zheng[23] compared 12 cases of femoral corrective osteotomy after DDH using patientspecific 3D navigation templates with 13 cases using conventional approaches[23].No differences in varus and angles were reported.However, significantly decreased operation time (26 min) and fluoroscopy were reported in favour of the 3D-printed model group.
3D techniques have also been used in pediatric foot orthopaedics.De Wouters[22] used 3D-printed PSI to guide the surgeon in removal of talocalcaneal and calcaneonavicular coalitions.It helped to orientate the saw blade for the resection of the bone bridge at the correct depth, which resulted in complete resections with no recurrence after a mean follow-up period of 18 mo.We have promising experience with 3D-guided resection of a calcaneonavicular coalition based on preoperative MRI (Figure 4).
He arrived home on February, 3, 1981.Three days later, he arranged to see Diana at Windsor Castle. Late that evening, while Prince Charles was showing Diana the nursery, he asked her to marry him.


ADDITIONAL APPLICATIONS OF 3D PRINTING IN PAEDIATRIC ORTHOPAEDICS
Over the last years, 3D printing has been successfully introduced in pediatric orthopaedics.Because of its seemingly endless possibilities, this relatively novel technique expands further than surgical applications alone.
As outlined, 3D printing seems to have great potential in numerous paediatric orthopaedic applications.However, there are several challenges in this field that need further investigation and improvement.
It was an immediate30 hit. Within six months sheet-music sales topped half a million copies. The haulting ballad31 expressed all the fears of a soldier far from home, yearning32 to be in his love s arms. Adaptations of Leip s poem have appeared in more than 40 languages
In the conservative treatment of paediatric fractures, two studies described the treatment of nondisplaced forearm fractures with a 3D-printed device compared to a traditional plaster cast[30,31].The results showed an improvement of wrist function after immobilization with a 3D-printed device.Moreover, activities of everyday life, patient satisfaction and patient comfort during the immobilization were improved compared to the traditional cast group.In addition, the 3D-printed devices were reported to be lighter than traditional casts and removable, which make them more patient-friendly (when taking a shower).This suggests that a 3D device can also be an effective alternative approach in the conservative treatment of fractures in paediatric orthopaedics.
CHALLENGES AND FUTURE OF 3D PRINTING IN PAEDIATRIC ORTHOPAEDIC SURGERY
In the technology of prosthetic limbs, 3D printing is increasingly used.Traditional prostheses for children with upper extremity amputees have been considered to be too heavy or too expensive to be a true benefit for a child[22].In addition, children outgrow prostheses and may damage them[26]In 3D printed prostheses, there is the possibility to replace a part of the prosthesis instead of the complete device[13].Children are also allowed to choose the design and colour schemes, which make 3Dprinted model prostheses more tailored to a child’s choices.Therefore, children may be more self-confident, as described in various studies of 3D-printed upper limb replacement[13,27-29].
He ducked, then countered with a left hook right under my eye. It was the first time all night he hadn’t offered me a selection. I collapsed12 semiconscious into my chair, as someone in authority rushed over and berated13 Pauly.
Another challenge is reduction of radiation exposure.Although the use of fluoroscopy during the surgical procedure is reduced by using 3D PSI or 3D-printed model guiding templates[23,33], the total dose of radiation might not be decreasedcase.A preoperative high-resolution CT scan is usually obtained to produce a 3D image, which is additional radiation exposure to the child[16,32].Instead, the use of MRI would help reduce the radiation exposure, with the possible additional advantage of a more detailed image of the paediatric anatomic structures (physeal bar, periosteum and soft tissue)[10].However, the process of undergoing an MRI scan is more difficult for very young children (under the age of 5), because of the necessity of sedation, motion reduction and/or accelerated imaging[7,8,17,34,35].Moreover, studies using MRI for preoperative imaging acquisition in 3D processes are scarce.Our case shows the potential of MRI to produce surgical 3D guides (Figure 4).
In addition, 3D printing requires advanced technology and financial resources, which may not be available in developing countries[32].However, printing costs seem to decrease over time[36] and costs of 3D printing may be outweighed by saving operation time.A cost analysis showed that using 3D-printed models saved a mean operating time of 62 min, translated to $3720case compared to conventional techniques[37].Due to the ambiguity in evidence on the cost-savings of using 3Dprinted models in paediatric orthopaedic surgery, an in-depth cost analysis is required of production costspotential savings obtained by improved intraoperative results[5].
Finally, more scientific evidence is required on the use of 3D techniques in paediatric orthopaedic surgery.Despite the fact that the current literature shows promising results for various indications as discussed, randomized trials on 3D printing compared to conventional methods are still lacking.It is likely to expect that 3D printing will be mainly beneficial for complex surgical cases.
It s good to be alive, and there are people out there who want your love. Get out and do something with the family. Spend time with the people who love you while you still can. Visit, ride bikes, stroll the beach, walk the dog, get some pictures, go out for coffee and pie, or go to church.
CONCLUSION
3D printing is a promising technique for numerous upper and lower limb surgical applications in paediatric orthopaedics.In upper limb surgery, 3D has been most frequently used in posttraumatic deformities.In lower limb surgery, 3D-printed models are mostly used to correct congenital and developmental deformities of the hip.Other applications of 3D-printed models include limb prostheses and non-surgical treatment of fractures.Future possibilities of this exciting technique are numerous.
The affordability of 3D printers has increased over the years, and literature shows that using 3D-printed models for PSI or intraoperative guiding reduces the operating time and radiation exposure.Moreover, an improved accuracy of deformity correction is attained.However, most studies have a low level of evidence.Moreover, using 3Dprinted models in pediatric orthopaedic surgery is complex due to growth of children and therefore, the moment of planningthe timing of the surgery is also a challenge to overcome.All in all, more research, preferably randomized controlled studies, is required to compare conventional approaches and the intraoperative use of 3Dprinted models.Nevertheless, the use of 3D-printed models as an intraoperative tool seems to have great future potential in complex pediatric orthopaedic surgical procedures.
ACKNOWLEDGEMENTS
The authors wish to thank Christa Niehot and Wichor Bramer from the Erasmus Medical Centre Medical Library for assistance with the literature search.
 World Journal of Orthopedics2022年1期
World Journal of Orthopedics2022年1期
- World Journal of Orthopedics的其它文章
- Long-term outcomes of the four-corner fusion of the wrist: A systematic review
- Comparing shoulder maneuvers to magnetic resonance imaging and arthroscopic findings in patients with supraspinatus tears
- High-resolution, three-dimensional magnetic resonance imaging axial load dynamic study improves diagnostics of the lumbar spine in clinical practice
- Can bedside needle arthroscopy of the ankle be an accurate option for intra-articular delivery of injectable agents?
- Epidemiology and incidence of paediatric orthopaedic trauma workload during the COVID-19 pandemic: A multicenter cohort study of 3171 patients
- Should we use similar perioperative protocols in patients undergoing unilateral and bilateral one-stage total knee arthroplasty?
