Comparing shoulder maneuvers to magnetic resonance imaging and arthroscopic findings in patients with supraspinatus tears
INTRODUCTION
Several shoulder maneuvers have been described and performed on patients undergoing shoulder arthroscopy; however, previous studies have shown that only the empty can and full can tests accurately diagnose supraspinatus tears[1].Moreover, other studies demonstrated that the drop arm test has the highest specificity (Sp) for supraspinatus tears[2].
When Muriel and I reached our little garden and sat down, his words came back to me. God had spoken through an inebriated18 old derelict. It is you who is whispering to my spirit, I likes it, tha s good, I said aloud. I may be on the bench, but if you like it and say it s good, that s all that counts.
For diagnostic confirmation of clinical findings, magnetic resonance imaging (MRI) has been used to evaluate rotator cuff tears (RCTs).MRI showed high sensitivity (Se) and Sp for full thickness tears; however, poor Se for detecting partial tears[3].Moreover, MRI is valuable in surgical planning of RCTs, allowing a detailed assessment of the tear size and muscle atrophy[4-7].
Resisted external rotation test: The patient stands, elbow at side and flexed at 90°, shoulder in neutral rotation, and then asked to externally rotate the shoulder maximally against the tester’s isometric resistance, applied at the wrist[9].
Although the literature is extensive on this subject, there is a lack of studies that compared the Se and Sp of shoulder maneuvers and MRI for supraspinatus tears.Therefore, the aim of this study was to evaluate the diagnostic values of seven clinical tests and MRI for supraspinatus tears in patients undergoing shoulder arthroscopy.We hypothesized that clinical tests will be as specific as MRI in diagnosing supraspinatus tendon tears.
MATERIALS AND METHODS
Study design
We carried out a prospective multicenter accuracy study at four orthopedic centers (Sao Paulo Hospital, Christóvão da Gama Hospital and Maternity, Wladimir Arruda Hospital and the Japanese-Brazilian Beneficent Hospital of São Paulo) from April 2017 to April 2019.The study was approved by an institutional review board under registration number 1662/2016 and registered on the ISRCTN registry platform (ID: ISRCTN13083925 – https://doi.org/10.1186/ISRCTN13083925)[11,12].
The inclusion criteria were patients who had an indication of arthroscopy for RCTs with symptoms of shoulder pain for at least 4 wk.The patients included in this study underwent shoulder maneuvers, MRI and arthroscopy; some of these patients were treated with physiotherapy for RCTs between the physical examination and arthroscopy.Patients excluded were those with adhesive capsulitis, glenohumeral osteoarthritis, or shoulder instability, three months after the physical examination, MRI and arthroscopy.
The empty can, full can and resisted external rotation tests showed improved results when positive for pain and weakness.Positivity only for pain in these tests had better Se, but less Sp; the positivity only for muscle weakness occurred in just a few cases and it was not possible to perform statistical analysis for this specific positivity criterion.The diagnostic values of these three clinical tests were calculated according to positivity only for pain and pain associated with weakness.
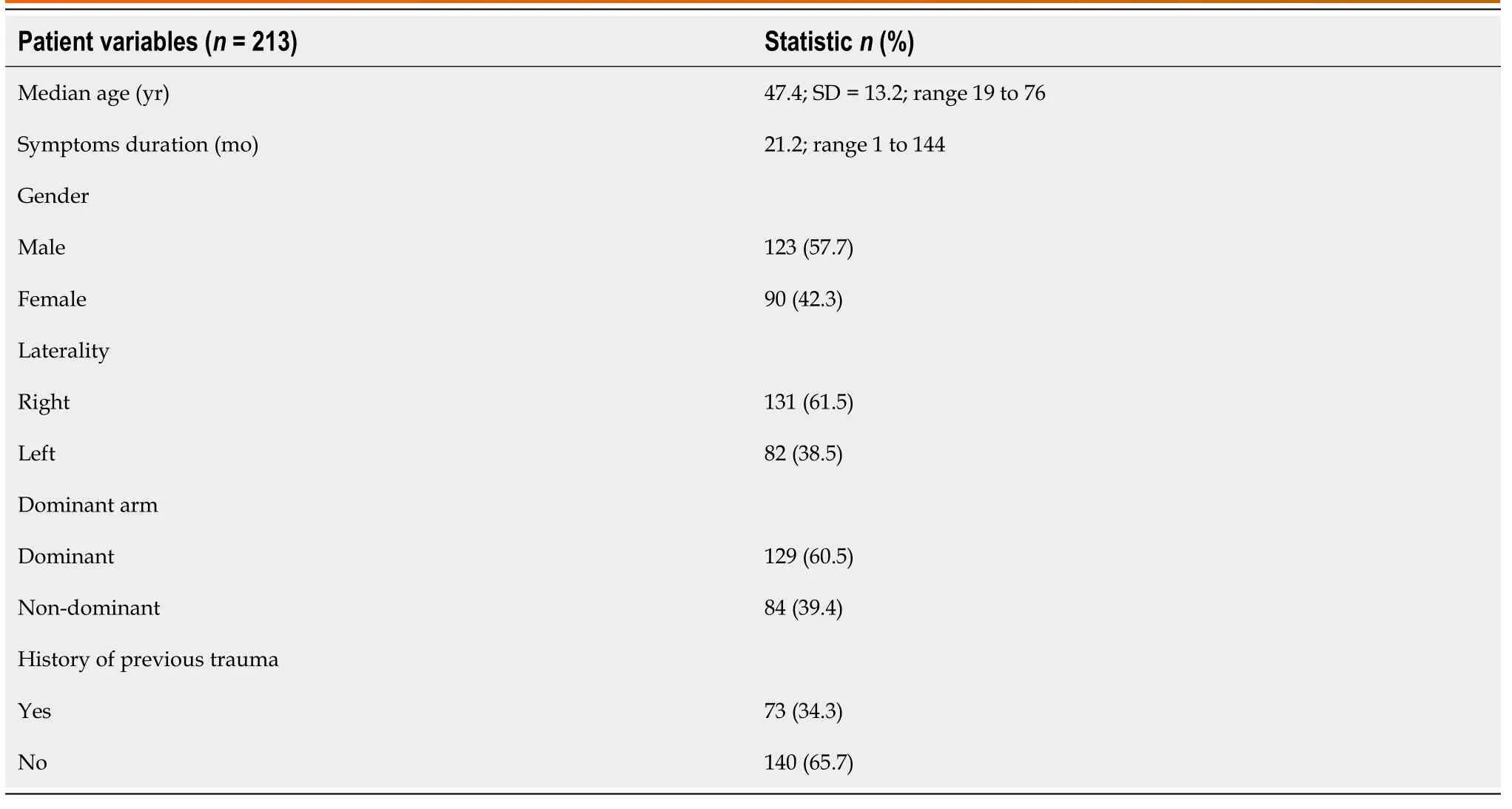
The following demographic information was obtained: Gender, age, symptoms duration (months), side involved, dominance of the affected limb, and history of previous shoulder trauma.Moreover, the time between the index tests (shoulder maneuvers and MRI) and the reference standard (arthroscopy) was evaluated.
Physical examination
Seven clinical tests (full can, empty can, drop arm, resisted external rotation, Hawkins’, painful arc, and Neer’s sign) were independently performed by four experienced orthopedic shoulder surgeons, in all patients sequentially, following a random order according to the choice of each evaluator and were not always performed in the same order.These tests were chosen based on previously published studies that evaluated the diagnostic values of the shoulder maneuvers for RCTs.The empty can, full can, Hawkin’s painful arc and Neer’s sign were standardized according to their original description; the drop arm and resisted external rotation tests, according to the description in the study by Hanchard[9].Before the start of the study, all four evaluators underwent training to standardize the technique and the positivity criteria of the shoulder maneuvers, in a sample of patients who were not included in this study.Clinical tests were conducted following an average interval of two minutes between each maneuver and a goniometer was used to measure the angles in the limb assessed.The evaluators were blinded to any previous clinical examination and imaging exams but had access to the history and demographic data of the patients.Only one shoulder surgeon assessed each patient.
When he had finished his story, the wolf, who was in reality no wolf but a mighty9 magician, said he thought he could tell him who the thief was, and could help him to secure him
We demonstrated high Sp and PPV of the drop arm test, unlike Somerville[33], who mentioned that no clinical test in isolation is sufficient to diagnose RCTs.Our results showed that the drop arm test is valuable for confirming overall supraspinatus tears (PPV = 0.97).The drop arm test had a similar Sp to MRI for supraspinatus tears; however, one factor contributing to the high Sp of these clinical tests was the possible association of supraspinatus and infraspinatus tears in patients included in this study.
Painful arc: The patient actively elevates the shoulder to full elevation, and then lowers it in the scapula plane.The test was interpreted positively if pain was reported during elevation, lowering, or both, between 60° and 120°[18].
Full can test: With the arm at 90° of abduction in the plane of the scapula and external rotation (thumb pointing up), the patient was asked to resist a downward pressure applied by the examiner isometrically[14].
Drop arm test: The patient elevated the arm above 90° of abduction, using a goniometer, passively by the examiner; the support was removed, and the patient attempted to lower the arm actively in the plane of abduction.This maneuver was considered positive if the patient did not hold the position or if the arm dropped abruptly when lowering the arm in the coronal plane[9,15].
Systematic reviews point out limitations in the accuracy studies of clinical tests and imaging exams for diagnosing RCTs, and these reviews suggested new research with improved methodological standards[3,8-10].The main weakness identified was the lack of standardization of the clinical tests, small sample size, absence of blinded evaluators, long time interval between the index tests and arthroscopy, retrospective method evaluation and the use of MRI as a reference standard instead of arthroscopy[3,9].
Hawkins’ test: The upright patient’s arm was passively positioned at 90° of shoulder and 90° of elbow flexion.The examiner then forced an internal rotation of the patient’s shoulder.The test was considered positive if pain was reported[16].
Neer’s sign: The tester passively elevated the patient’s arm in the plane of the scapula, preventing scapular movement by holding with the other hand.The test was considered positive if pain occurred during the elevation[17].
Empty can test: With the arm at a position of 90° of abduction in the scapula plane and internal rotation (thumb pointing down), the patient was asked to isometrically resist a downward pressure applied by the examiner[13].
The muscle strength of empty can, full can and resisted external rotation was manually measured and interpreted positively if the patient was unable to overcome the resistance imposed by the examiner or if the strength decreased in relation to the contralateral side[1].If weakness was observed, the test was interpreted as positive.The pain was not graduated, and any level of pain when performing the maneuver was considered positive.The empty can, full can and resisted external rotation tests were interpreted as positive in the case of pain and/or weakness.
MRI
Yes, yes! the little lumps echoed. But already the seed had been planted and little lump 2 wondered what wisdom she was lacking if she failed to look to the nothingness.
Arthroscopy
Arthroscopy was the reference standard and was performed by two experienced orthopedic shoulder surgeons.The principal surgeon was involved in the clinical history and the preoperative physical examination; the assistant was blinded to all the clinical tests and MRI.All patients were placed in the lateral decubitus position with an anterior pad and another in the back, under general anesthesia, and a brachial plexus block.Eleven pounds of balanced suspension was used with the arm in 30° to 45° of abduction and 30° to 45° of forward flexion, and posterior inclination of the back to leave the glenoid parallel with the horizontal.The standard posterior portal was used to evaluate the supraspinatus tendon from the articular side.Through the lateral portal, the tendon was assessed from the subacromial space with a 30° arthroscope.A probe was used to identify tears, and the supraspinatus tendon was classified as intact, partial or full-thickness tears.
Sample size
The sample size was calculated assuming that the Se was 0.90, the prevalence of RCTs in the general population was 22%, a confidence interval (CI) of 95% with a marginal error of 0.10, resulting in a sample size of at least 157 patients[19-21].
Statistical analysis
The clinical tests and MRI results were compared with the surgical findings of arthroscopy to analyze the diagnostic values.Statistical analysis included the Se, Sp, positive predictive value (PPV), negative predictive value (NPV), accuracy, diagnostic odds ratio (DOR), and likelihood ratio[22].These ratios were used to predict overall, partial and full-thickness tears.The Se and Sp are presented with the 95%CI.Tests were performed using SPSS software (ver.25 for Mac; IBM Corp., New York, United States).
RESULTS
A total of 720 patients were consecutively seen at four orthopedic centers, 213 had an indication for shoulder arthroscopy and were included.Fourteen patients were excluded because the period between the performance of the index tests (shoulder maneuvers and MRI) and arthroscopy was greater than three months, and 199 patients met enrollment criteria for the final analysis.Demographic data were collected and are shown in Table 1.
A total of 47 intact tendons, 62 partial tears (32 bursal-side and 30 articular-side tears) and 90 full-thickness tears (70 supraspinatus, 20 supraspinatus and infraspinatus tears) were found during arthroscopy.The arthroscopy was performed within a mean of 37 d (range, 1 to 83 d) after the physical examination and within 55 d (range, 4 to 89 d) after MRI.
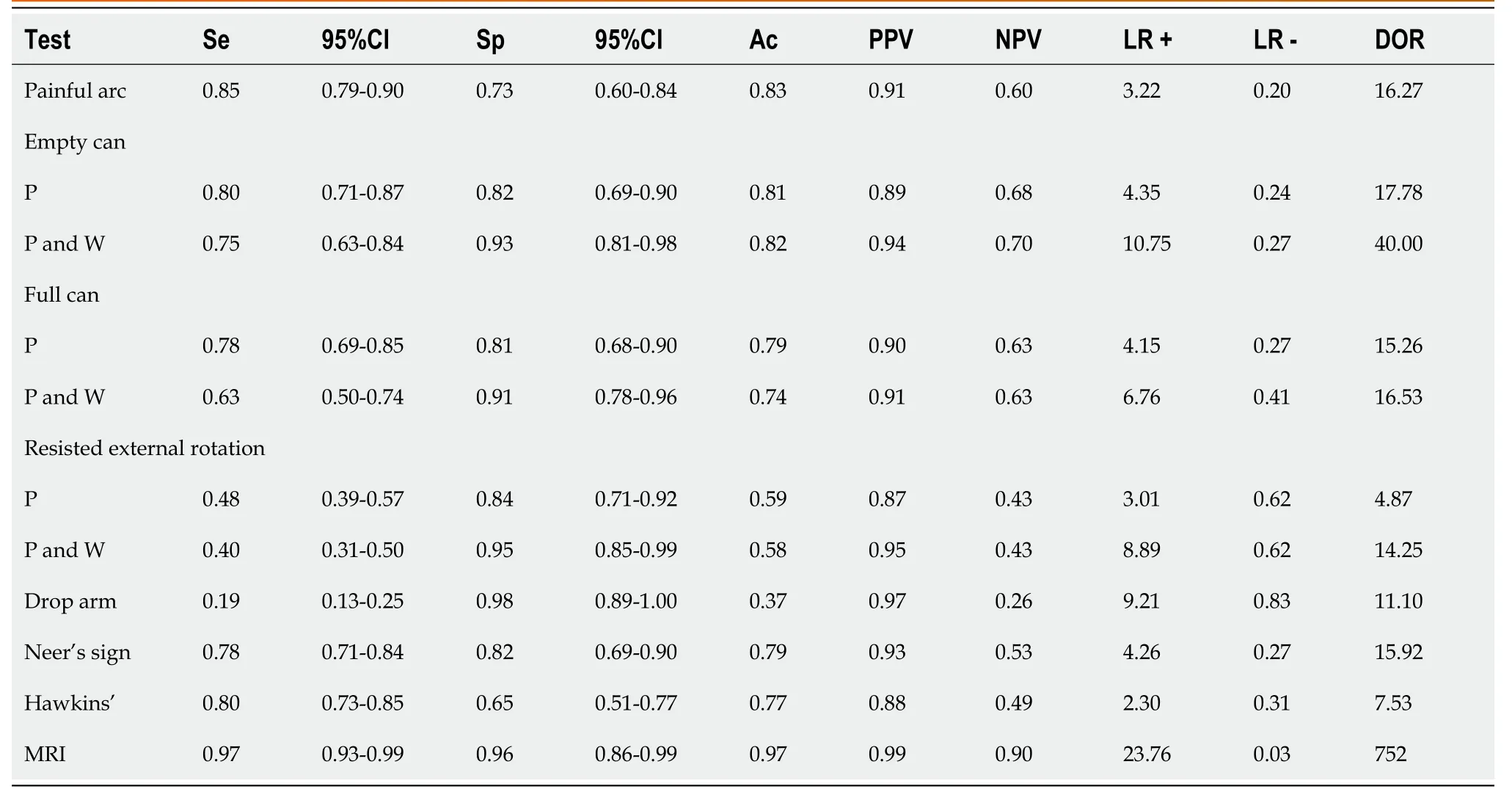
MRI had the highest Se for overall tears (Table 2) (Se = 0.97).Among the clinical tests, the painful arc had the highest Se (Se = 0.85) and the empty can (positive for pain and weakness) had the best performance (DOR = 40).The drop arm test had the highest Sp (0.98), whereas the Sp for MRI for diagnosis of supraspinatus tears was 0.96.The shoulder maneuvers presented low values to rule out tears and the empty can test had the highest NPV between the physical examinations (0.70).The drop arm test and MRI had the highest PPV (0.97 and 0.99, respectively).
The false positive results for overall tears were: Painful arc (0.28), empty can (pain = 0.19/pain and weakness = 0.08), full can (pain = 0.19/pain and weakness = 0.11), resisted external rotation (pain = 0.20/pain and weakness = 0.06), drop arm (0.04), Neer’s sign (0.19), Hawkin’s (0.36), and MRI (0.02).
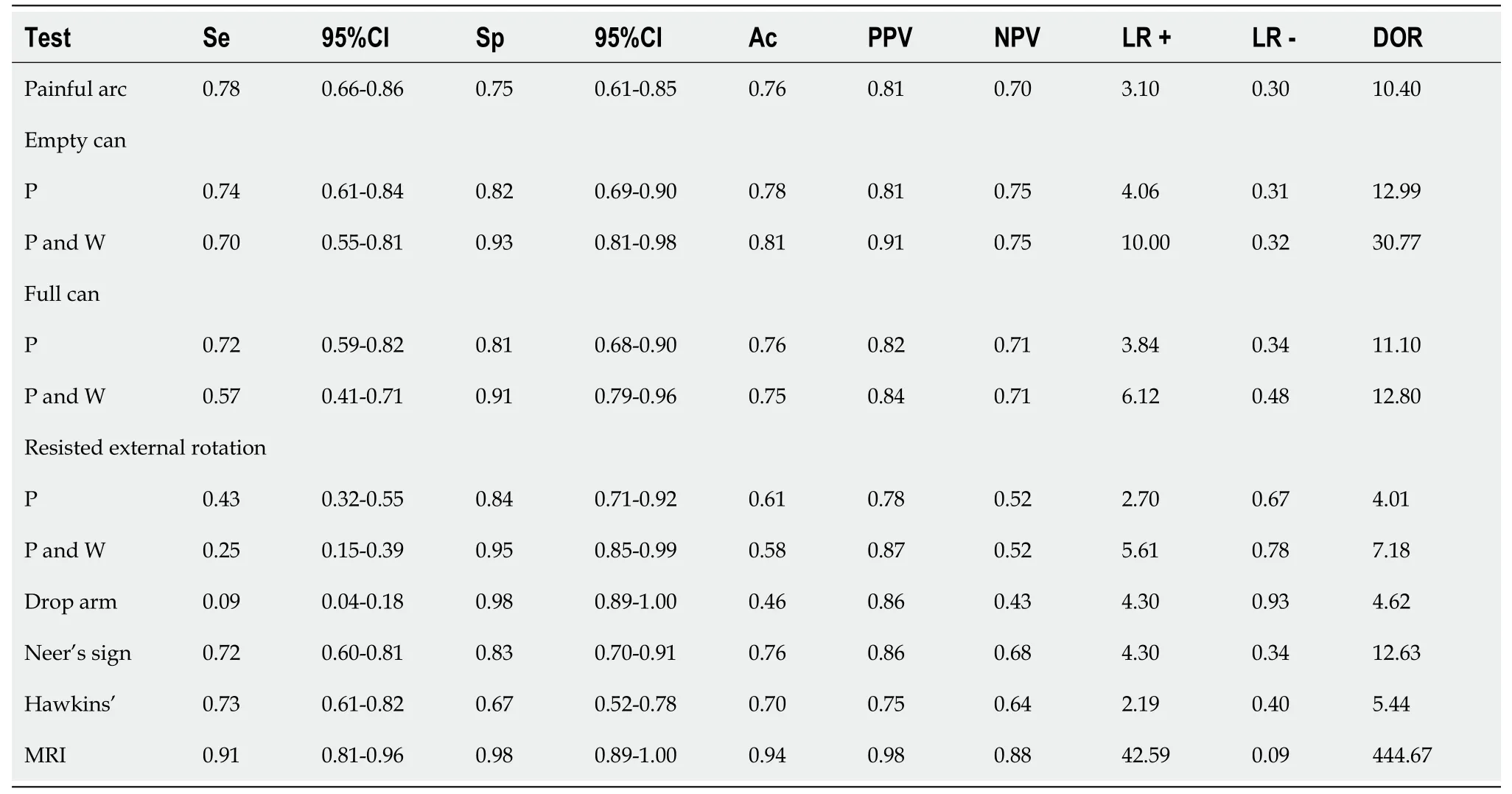
For partial tears (Table 3), MRI had the highest Se (0.91); however, MRI had the same Sp (0.98) as the drop arm test.For full thickness tears (Table 4), the empty can test (positive for pain and weakness) had a Se = 0.84; Sp of the drop arm was 0.98, and the MRI had a Se = 0.99 and Sp = 0.98.

DISCUSSION
This study demonstrated the significance of clinical tests for the diagnosis of supraspinatus tears in patients with an indication for shoulder arthroscopy.The Sp of the drop arm test for supraspinatus tears was similar to that of MRI.On the other hand, the physical examination demonstrated limited diagnostic value in ruling out tears when compared to MRI.
IN a certain Tsardom,2 across three times nine kingdoms, beyond high mountain chains, there once lived a merchant.3 He had been married for twelve years, but in that time there had been born to him only one child, a daughter, who from her cradle was called Vasilissa the Beautiful. When the little girl was eight years old the mother fell ill, and before many days it was plain to be seen that she must die.4 So she called her little daughter to her, and taking a tiny wooden doll5 from under the blanket of the bed, put it into her hands and said:
32. Dead: Bruno Bettelheim interprets the story as a classic mother/daughter conflict in which children receive cathartic pleasure in seeing the mother/stepmother endure a horrible punishment for her crimes against innocent youth (Bettelheim 1975). HAH Return to place in story.
The strengths of this study were the inclusion of a consecutive and representative sample of patients; experienced shoulder surgeons performed the physical examination; the technique was standardized, and the positivity criterion for each clinical test was fulfilled.Therefore, we demonstrated that trained orthopedists could perform clinical tests with high Sp for the diagnosis of supraspinatus tears[3,23-27].Moreover, arthroscopy was utilized as a reference standard, a minimally invasive surgical procedure that is the gold standard for diagnosis and is widely used to treat RCTs[1].Through arthroscopy, the evaluator can inspect and probe the partial articular and bursal-side tears, assess the rotator cuff footprint accurately and perform a general examination of the shoulder joint in order to identify and treat associated rotator cuff lesions[3].
To standardize shoulder maneuvers is challenging due to the high variability in performance and interpretation.The empty can test, for example, adopts the interpretative criteria of pain, muscle weakness, or both, affecting Se and Sp, as demonstrated in this study[8,9].Muscle weakness was previously demonstrated in other studies as a reliable criterion, and in our study, the pain associated with weakness obtained the highest Sp[1,28].We observed that many patients with supraspinatus tears had pain associated with weakness, demonstrating that pain can be a cause for functional disability when performing the test[1,28], as described by Jobe[13,29].
He became patient and understanding about things that are important to me in my life like school and my grades. Now we work at different places but we make plenty of time to see each other, loyally attending each other s homes and events. I love him and how this love appeared doesn t matter to me.
Another methodological criterion adopted here was establishing a time limit between physical examination, MRI and arthroscopy, a criterion little used in other accuracy studies and cited as one of the weaknesses in systematic reviews[3,9].In this study, we choose a three-month interval between the index tests and arthroscopy, to reduce the interpretation bias, different to that in other studies[5,30-33].The ideal would be to carry out the index tests and arthroscopy in the same day or week;however, we chose the limit of three months, mainly due to the logistics of the orthopedic centers included in the study, as there is a waiting list for these procedures[34].
The seven clinical tests were performed as described below:
A dense1 forest lay all round the cottage, and there was hardly a path or a tree in the whole wood that was not familiar to the peasant from his boyhood
Physical examination has already been demonstrated in previous studies as limited in ruling out RCTs[1,33].The limitations of the shoulder maneuvers for excluding supraspinatus tears were also shown in our study; moreover, the painful arc and Hawkins’ tests had the highest false-positive rates in patients with intact tendons.
Physical examination alone cannot quantify the size and extension of the supraspinatus tear, muscle atrophy, and associated rotator cuff lesions (biceps tendon pathologies and acromioclavicular joint osteoarthritis).Therefore, imaging exams, such as radiography, ultrasonography, or MRI, are essential to determine surgical indication[33].
The large trees which grew round it saw the plant and heard theremarks, but they said not a word either good or bad, which is thewisest plan for those who are ignorant.
The Prince s grief at the death of his mother was great, but it was nothing compared to that of the King, his father, who was quite inconsolable for the loss of his dear wife
MRI results were evaluated by two blinded musculoskeletal radiologists, who had no prior information on the patient’s physical examination.The radiologists evaluated each MRI together and there was a consensus on diagnosis of the lesions.MRI was performed using 3.0 Tesla devices, and the shoulder was placed in a dedicated receiveonly shoulder coil.The supraspinatus was evaluated in the axial, oblique coronal, and oblique sagittal planes, at 4 to 5-mm section thickness.The sequences performed were two T1-weighted planes centered on the rotator cuff muscles: The axial plane, covering from the greater tubercle of the humerus to the spinal edge of the scapula, and the oblique sagittal plane, covering the tuberosity to the medial third of the scapula.In T2-weighted imaging, three acquisition planes were chosen: The axial plane, from the top of the acromioclavicular joint to the lower recess of the glenohumeral joint; oblique coronal plane, parallel to the supraspinatus and covering the entire scapular-humeral joint; and the oblique sagittal plane, perpendicular to the supraspinatus, from the distal end of the tendon to the middle part of the rotator cuff muscle belly.The supraspinatus was classified as intact tendon, partial or full-thickness tears according to the fluid signal intensity in T2-weighted coronal and sagittal scans.
Limitations
First, the reliability of the clinical tests, MRI and arthroscopy was not evaluated.Previous studies demonstrated a moderate to substantial agreement of the empty can, painful arc and external rotation resistance tests, but a fair agreement for the Hawkins’ and the Neer’s sign[35].We suggest that future studies should evaluate mainly the reliability and analysis of Se and Sp of the physical examination.
That was the first time I knew he knew my name. Well, Rog, these guys from my college wanted to meet you, and I just wanted to say hello. The five of them paraded by and shook hands, and they couldn t believe it. I wished Rog good luck and he said, Wait a minute. I want to give you an autograph on a National League ball. And he went into the dugout and got a ball and signed it. I put it in my pocket and felt like a million dollars.
Second, muscle weakness was evaluated manually using subjective criteria according to each tester.We did not use a dynamometer for objective data collection, as some studies considered a 20% decrease in strength in relation to the contralateral side, a positivity criterion for weakness[36].Moreover, we did not quantify pain when performing each maneuver, with a visual analogue scale, for example, and any shoulder pain during the test was considered positive.
Third, the principal surgeon performing the arthroscopy was not blinded to the shoulder maneuvers and MRI; however, to reduce this bias, we included a second surgeon’s evaluation, blinded to physical examination and MRI.
CONCLUSION
Physical examination demonstrated good diagnostic value, showing that the drop arm test had a similar Sp to MRI for supraspinatus tears.However, MRI had higher Se compared with the shoulder maneuvers and was more accurate in ruling out supraspinatus tears.
ARTICLE HIGHLIGHTS
Research background
Shoulder maneuvers and magnetic resonance imaging (MRI) are performed in current practice in patients with rotator cuff tears (RCTs); however, there is insufficient evidence as to which clinical test is efficient for diagnosing supraspinatus tears.
Research motivation
The motivation for this study was the exponential increase in MRI requests and little appreciation of physical examination in patients with RCTs.
Research objectives
The objective of this study was to compare the accuracy of clinical tests with MRI for diagnosing supraspinatus tears.
Research methods
A prospective multicenter accuracy study of seven shoulder maneuvers and MRI for supraspinatus tears in patients undergoing arthroscopy was performed.
Research results
MRI and the drop arm test had the highest specificity (0.99 and 0.97, respectively) for overall supraspinatus tears; the Hawkin’s test had the highest rate of false-positive findings (0.36) in patients with intact tendons.
Research conclusions
Shoulder maneuvers had good diagnostic value for supraspinatus tears; however, MRI had the highest diagnostic value for ruling out tears.
Research perspectives
Futures studies are necessary to analyze the accuracy of clinical tests and MRI for infraspinatus and subscapularis tears.
The King in his anguish of mind consented, and the old woman led him to her little house where her daughter was sitting by the fire. She received the King as if she were expecting him,10 and he saw that she was certainly very beautiful; but she did not please him, and he could not look at her without a secret feeling of horror.11 As soon as he had lifted the maiden on to his horse the old woman showed him the way, and the King reached his palace, where the wedding was celebrated.
ACKNOWLEDGEMENTS
The authors would like to thank the contribution of the Orthopedics and Traumatology Department of Escola Paulista de Medicina – Universidade Federal de São Paulo – UNIFESP, for supporting the realization of this study; without their support, this project would not have been completed.
 World Journal of Orthopedics2022年1期
World Journal of Orthopedics2022年1期
- World Journal of Orthopedics的其它文章
- Long-term outcomes of the four-corner fusion of the wrist: A systematic review
- High-resolution, three-dimensional magnetic resonance imaging axial load dynamic study improves diagnostics of the lumbar spine in clinical practice
- Can bedside needle arthroscopy of the ankle be an accurate option for intra-articular delivery of injectable agents?
- Epidemiology and incidence of paediatric orthopaedic trauma workload during the COVID-19 pandemic: A multicenter cohort study of 3171 patients
- Should we use similar perioperative protocols in patients undergoing unilateral and bilateral one-stage total knee arthroplasty?
- Management of proximal biceps tendon pathology
