个性化内镜技术在经鼻入路岩斜区病变手术中的应用
王志成 傅骏 颜小荣 王行富 李坚 江常震 王晨阳 林元相 康德智
岩部尖系指颞骨最内侧的锥状部分,其外侧基底为耳蜗、迷路和颈内动脉(ICA)岩骨段,内侧为斜坡和脑干,前方为颈内动脉斜坡段,后方正对脑桥小脑角(CPA)和颈静脉孔,上方为海绵窦、颈内动脉海绵窦段和 Meckel憩室[1⁃2]。岩斜区病变的病因谱广泛,包括胆固醇肉芽肿、胆脂瘤、表皮样囊肿、脑膜瘤、神经鞘瘤、神经纤维瘤、脊索瘤、真菌性炎症、慢性骨髓炎致骨质增生等[2⁃4]。岩斜区解剖结构复杂,位于颅底,位置深在,该部位病变常与颈内动脉、第Ⅱ~ Ⅵ对脑神经、脑干和海绵窦密切相关,给手术安全切除带来极大挑战[1⁃2,5]。目前的外科手术方式主要包括开颅经侧方入路和内镜下经鼻入路。福建医科大学附属第一医院近2年采用神经导航辅助内镜下经鼻入路手术切除6例岩斜区病变,回顾总结其临床资料,探讨内镜技术在经鼻岩斜区病变切除术中的应用及其有效性和安全性。
资料与方法
一、临床资料
1.纳入与排除标准 (1)术前头部MRI提示岩斜区占位性病变。(2)均行内镜下经鼻入路手术。(3)排除岩斜区以外颅内病变和开颅手术患者。(4)所有患者及其家属均对手术方案知情并签署知情同意书。
2.一般资料 选择2018年1月至2020年12月在福建医科大学附属第一医院神经外科行神经导航辅助内镜下经鼻入路岩斜区病变切除术的患者共6例,男性4例,女性2例;年龄30~ 56岁,中位年龄 48.50(32.25,55.25)岁;临床表现为眼球外展受限占3/6,视物重影占3/6,视力下降占2/6,视野缺损占1/6,头晕占2/6,头痛占1/6。术前头部MRI显示,肿瘤累及斜坡4例,海绵窦2例,岩部尖1例。6例岩斜区病变患者的临床资料参见表1。

表1 6例岩斜区病变患者的临床资料Table 1. Clinical data of 6 patients with petroclival lesions
二、研究方法
1.术前准备及手术入路 所有患者均行神经导航辅助内镜下经鼻岩斜区病变切除术+鞍底修补术。术前30 min和手术时间>3 h时,分别予头孢唑啉1 g静脉滴注预防感染。患者平卧位,气管插管全身麻醉,头稍向左侧偏斜、右旋10°、后仰5°,立体定位头架固定,注册神经导航系统。经双侧鼻腔注入碘伏消毒,以肾上腺素生理盐水棉片收缩双侧鼻腔黏膜和鼻甲,在神经内镜(德国Karl Storz公司,0°和30°镜头)引导下根据肿瘤部位选择性切除单侧或双侧部分中鼻甲、钩突、筛泡和后组筛窦;根据鞍底修补需要,于右侧或左侧鼻腔内制备带蒂鼻中隔黏膜瓣并置于后鼻孔处备用;确认蝶窦开口后切开鼻中隔黏膜,显露犁状骨,磨开蝶窦前壁,根据需要磨除部分翼突,扩大开放蝶窦前壁,充分显露并确认鞍底、斜坡隐窝、颈内动脉沟和翼管等重要解剖结构;磨除蝶窦分隔,清除蝶窦黏膜并充分止血。
2.手术方法 根据患者肿瘤部位和大小,个性化剥离颈内动脉并向侧方移位、垂体移位、选择性切除海绵窦壁、磨除蛋壳化骨质、术中多普勒超声等技术切除肿瘤。(1)内镜下经鼻入路切除右侧海绵窦⁃鞍旁区⁃右侧岩部尖病变:1例(例1)肿瘤位于右侧海绵窦⁃鞍旁区并累及右侧岩部尖患者,术中经神经导航系统探测到颈内动脉斜坡段和肿瘤部位后,沿斜坡隐窝与鞍底交界处磨除骨质,可见斜坡骨质异常增生,骨质内可见肿瘤,呈灰色,大小约4.00 cm×2.00 cm×3.50 cm,质地柔软,血供一般,伴钙化,磨除增生骨质及其内肿瘤后,显露岩部尖方向肿瘤,刮圈刮除后可见斜坡硬脑膜局部破损,有脑脊液渗出,以自粘人工脑膜行鞍底修补。(2)内镜下经鼻入路切除斜坡右后上方、右颈内动脉斜坡段后内方病变:1例(例2)肿瘤位于斜坡右后上方、右颈内动脉斜坡段后内方患者,术中经神经导航系统探测到颈内动脉斜坡段和肿瘤部位后,自斜坡隐窝外侧、颈内动脉斜坡段内侧向后下方磨开斜坡骨质,显露部分肿瘤后,蛋壳化骨质磨除技术小心磨除颈内动脉沟骨质,显露颈内动脉斜坡段,继续向后下磨除骨质至破裂孔,充分显露颈内动脉,旷置并严密保护,继续扩大斜坡骨窗,小心剥离颈内动查颈内动脉后,蛋壳化骨质磨除技术小心磨除颈内动脉沟骨质,充分显露颈内动脉并严密保护;进一步磨除斜坡隐窝左侧骨质,充分显露肿瘤,刮圈逐步刮除,可见肿瘤侵犯左侧海绵窦下后壁,选择性切除海绵窦壁,彻底探查并刮除肿瘤,直至无明显残留;斜坡硬脑膜有少量澄清脑脊液渗出,以自粘人工脑膜进行鞍底修补。(6)内镜下经鼻入路切除斜坡左侧、左颈内动脉斜坡段后方病变:1例(例6)肿瘤位于斜坡左侧、左颈内动脉斜坡段后方患者,术中经神经导航系统确认病变位于斜坡旁左颈内动脉后方,磨除斜坡左侧骨质至硬脑膜,向外侧蛋壳化磨除左颈内动脉沟表面骨质,有黄色胆固醇结晶样囊液流出,严密保护颈内动脉后继续扩大骨窗,向下至破裂孔,吸除囊液后内镜进入囊腔,可见其中存在部分黄色残渣样组织,夹取部分组织行病理学检查,并尽可能分离与颅底硬脑膜的粘连,反复探查直至确认无明显残留;未见脑脊液渗出,以带蒂鼻中隔黏膜瓣进行鞍底修补。脉并向外侧化,充分显露肿瘤,呈黄色,约3.00 cm×2.50 cm×3.00 cm,质地柔软,严重侵袭骨质,部分斜坡和岩部尖骨质呈虫蚀状,可见肿瘤浸润,刮圈最大限度刮除肿瘤,观察硬脑膜是否完整、有无脑脊液漏;以带蒂鼻中隔黏膜瓣进行鞍底修补。(3)内镜下经鼻入路切除斜坡左后上方病变:1例(例3)肿瘤位于斜坡左后上方患者,于术中磨除鞍底骨质后,经神经导航系统确认双侧颈内动脉位置,自硬脑膜外向上移位垂体,小心磨除斜坡骨质,可见肿瘤侵袭斜坡松质骨,呈灰白色,约2.50 cm×1.50 cm×2.50 cm,质地较韧,以30°内镜向斜坡左上方探查,磨除斜坡骨质后见硬脑膜外质地坚硬的肿瘤组织,咬钳分块咬除硬脑膜外肿瘤组织,斜坡处硬有脑膜无色透明脑脊液渗出;采用自粘人工脑膜+带蒂鼻中隔黏膜瓣+右大腿外侧自体脂肪和阔筋膜进行鞍底修补。(4)内镜下经鼻入路切除斜坡隐窝旁、右颈内动脉斜坡段后方病变:1例(例4)肿瘤位于斜坡隐窝旁、右颈内动脉斜坡段后方患者,术中经神经导航系统确认肿瘤位于斜坡隐窝旁、右颈内动脉斜坡段后方,局部骨质突出,内镜下小心磨除斜坡骨质,显露肿瘤包膜,经多普勒超声确定颈内动脉位于肿瘤前方,镰状刀切开肿瘤包膜后可见肿瘤组织,呈黄白色,大小约3.00 cm×2.00 cm×2.50 cm,质地较脆,部分囊性变,分块切除部分肿瘤,充分减容后,以中鼻甲骨质+带蒂鼻中隔黏膜瓣进行鞍底修补。(5)内镜下经鼻入路切除左侧海绵窦区病变:1例(例5)肿瘤位于左侧海绵窦区患者,术中清除蝶窦黏膜后于左颈内动脉沟内侧见侵袭斜坡骨质、长入蝶窦内的肿瘤组织,呈红白色,大小约1 cm×1 cm×1 cm,质地柔软,确认翼管位置,经神经导航系统探
3.评价指标 术后观察症状缓解情况和缓解时间。记录术后3个月内脑脊液漏、中枢神经系统感染、视力较术前下降、新发视野缺损或视野缺损较术前加重等并发症发生率,非计划二次手术率及病死率。随访至术后3个月、6个月、1年、2年和5年,复查MRI观察是否复发。
结 果
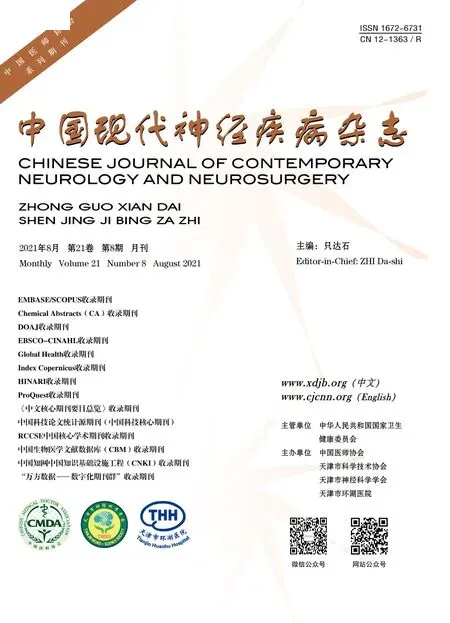
本研究6例患者均顺利完成手术,手术时间为3.08~ 5.92 h、平均4.53 h。术后病理证实3例软骨肉瘤(WHO 2级2例,WHO 1级1例;图1),1例神经鞘瘤(图 2),1例脊索瘤(图 3),1例胆固醇肉芽肿(图4)。除1例术后视物重影较术前未缓解外,其余5例术前症状均不同程度缓解。本组患者术后住院3~ 10 d,平均5.67 d;术后随访0.70~ 35.77个月,中位时间14.07个月。术后3个月内无一例出现脑脊液漏、中枢神经系统感染、视力较术前下降、新发视野缺损或缺损较术前加重等并发症,均未行非计划二次手术,无死亡病例。截至末次随访时,未见复发病例。本研究6例岩斜区病变患者的术后资料参见表2。

表2 6例岩斜区病变患者的术后资料Table 2. Postoperative clinical data of 6 patients with petroclival lesions
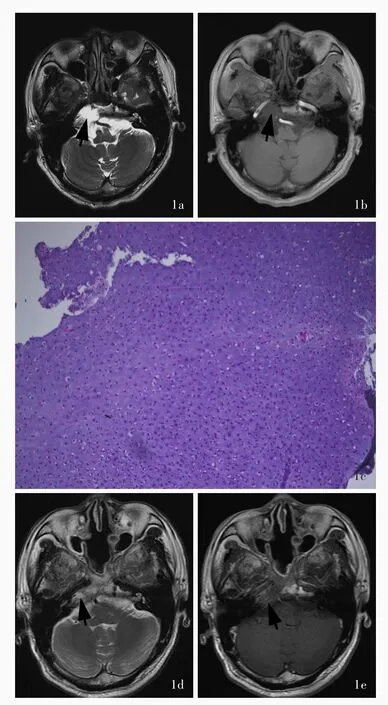
图1 例2患者,男性,56岁,因斜坡右后上方、右颈内动脉斜坡段后内方占位性病变入院,行神经导航辅助内镜下经鼻入路斜坡区病变切除术,最大限度切除病变,术后病理证实为软骨肉瘤 1a 术前横断面T2WI显示,斜坡右侧不规则异常高信号影,界限尚清,边缘欠规整,大小约3.20 cm×2.40 cm×2.90 cm(箭头所示) 1b 术前横断面增强T1WI显示病变呈轻度斑片样强化(箭头所示) 1c 组织病理学检查显示,软骨样细胞呈轻至中度增生,轻度异形性,可见双核细胞,符合低级别(WHO 1级)软骨肉瘤 HE染色 ×100 1d 术后6个月复查横断面T2WI,斜坡右侧仍可见不规则略高信号影,界限尚清,边缘欠规整(箭头所示) 1e 术后6个月横断面增强T1WI显示,病变呈轻度不均匀强化(箭头所示)Figure 1 A 56⁃year⁃old male(Case 2)was admitted to the hospital for space⁃occupying lesions in the upper right posterior side of the cilvus and the posterior inner side of right ICA,and underwent neuronavigation assisted endoscopic endonasal approach resection of the lesion. The lesion was removed to the maximum extent during the operation,and which was confirmed to be chondrosarcoma by pathology Preoperative axial T2WI showed irregular long T2abnormal signal shadow on the right side of the cilvus,the boundary was still clear,the edge was not regular,the size was about 3.20 cm×2.40 cm×2.90 cm (arrow indicates,Panel 1a). Preoperative axial enhanced T1WI showed mild patchy enhancement (arrow indicates),and the adjacent clival bone was invaded(Panel 1b).Histopathological examination showed chondroid cells were mildly to moderately proliferated,mildly atypia,and binuclear cells could be seen,in line with low⁃grade(WHO grade 1)chondrosarcoma(Panel 1c). HE staining ×100 Axial T2WI 6 months after operation showed irregular long T2abnormal signal shadow could still be seen on the right side of the cilvus,the boundary was still clear, the edge was irregular (arrow indicates,Panel 1d).Axial enhanced T1WI 6 months after operation showed the lesion was mild uneven enhancement(arrow indicates,Panel 1e).

图2 例4患者,女性,55岁,因斜坡隐窝旁、右颈内动脉斜坡段后方占位性病变入院,行神经导航辅助内镜下经鼻入路斜坡区病变切除术,部分切除病变,充分减容,术后病理证实为神经鞘瘤 2a 术前横断面T2WI显示,右侧岩部尖可见一囊实性异常信号影,大小约3.00 cm×2.30 cm×2.50 cm,实性部分呈稍高信号,边界尚清(箭头所示) 2b 术前横断面增强T1WI显示,病变实性部分和囊壁明显强化(箭头所示),邻近骨质破坏 2c 组织病理学显示,肿瘤细胞呈梭形,符合神经鞘瘤 HE染色 ×100 2d 术后5个月横断面T2WI显示,右侧岩部尖可见囊实性病变范围较术前减小(箭头所示) 2e 术后5个月横断面增强T1WI显示,病变实性部分和囊壁明显强化Figure 2 A 55⁃year⁃old female(Case 4)was admitted to the hospital due to space⁃occupying lesions near the recess of the clivus and behind right ICA, and underwent neuronavigation⁃assisted endoscopic endonasal approach resection of the lesions. Part of the lesion was surgically removed,the volume was fully reduced. Postoperative pathology confirmed that the lesion was schwannoma Preoperative axial T2WI showed a cystic solid abnormal signal shadow could be seen in the right apex of petrous part,and the size was about 3.00 cm×2.30 cm×2.50 cm,and the solid part showed a slightly long T2signal,the boundary was still clear(arrow indicates, Panel 2a). Preoperative axial enhanced T1WI showed the solid part and capsule wall of the lesion were significantly strengthened(arrow indicates),and the adjacent bone was invaded(Panel2b). Histopathological examination showed spindle cell tumor in line with schwannoma(Panel 2c). HE staining ×100 Axial T2WI 5 months after operation showed that cystic solid abnormal signal shadow was smaller than thatof before operation (arrow indicates, Panel 2d). Axial enhanced T1WI 5 months after operation showed the solid part and capsule wall of the lesion were significantly strengthened(arrow indicates,Panel 2e).
图3 例5患者,男性,55岁,因左侧海绵窦区占位性病变入院,行神经导航辅助内镜下经鼻入路斜坡区病变切除术,手术全切除病变,术后病理证实为脊索瘤 3a 术前横断面T2WI显示,左侧海绵窦区可见一类圆形异常稍高信号影,大小约0.80 cm×1.00 cm×1.10 cm,边界尚清,病变后向突入桥前池(箭头所示) 3b 术前横断面增强T1WI显示,病变明显强化(箭头所示) 3c 组织病理学显示,肿瘤细胞呈片状排列,胞质丰富、嗜酸性,可见黏液性间质,符合脊索瘤 HE染色 ×100 3d 术后3个月横断面增强T1WI显示,术区原病变消失Figure 3 A 55⁃year⁃old male(Case 5)was admitted to the hospital due to a space⁃occupying lesion in the left cavernous sinus,and underwent neuronavigation⁃assisted endoscopic endonasal approach resection of the lesion. The lesion was completely resected,which was confirmed to be chordoma by postoperative pathology Preoperative axial T2WI showed a kind of circular abnormal signal shadow could be seen in the left cavernous sinus area,showing slightly long T2signal,and the size of the lesion was about 0.80 cm×1.00 cm×1.10 cm with clear boundary,the focus protruded into the prepontile cistern(arrow indicates,Panel 3a). Preoperative axial enhanced T1WI showed obvious enhancement of lesion(arrow indicates,Panel 3b).Histopathological examination showed the tumor cells were arranged in flakes,with rich cytoplasm and eosinophilic.Mucinous stroma could be seen,which was in line with chordoma(Panel 3c). HE staining ×100 Axial enhanced T1WI 3 months after operation showed no obvious abnormal signalshadow and enhancement focus were found in the operation area(Panel 3d).

图4 例6患者,男性,30岁,因斜坡左侧、左颈内动脉斜坡段后方占位性病变入院,行神经导航辅助内镜下经鼻入路斜坡区病变切除术,术后病理证实为胆固醇肉芽肿 4a 术前横断面T2WI显示,左侧岩部尖可见团块状异常高低混杂信号影,病变略突向左侧脑桥小脑角区,边界尚清,大小约为2.40 cm×3.60 cm×2.50 cm(箭头所示) 4b 术前矢状位T1WI显示病灶呈不均匀高信号影(箭头所示) 4c组织病理学可见凝血组织,周围纤维结缔组织形成,伴含铁血黄素沉积和胆固醇结晶形成,以及少量淋巴单核细胞浸润,符合胆固醇肉芽肿 HE染色 ×100 4d 术后3个月复查横断面 T2WI,可见术区片状高信号影(箭头所示) 4e 术后3个月复查矢状位T1WI显示术区可见片状高信号影(箭头所示)Figure 4 A 30⁃year⁃old male(Case 6)was admitted to the hospital with a space⁃occupying lesion on the left side of the clivus and behind the left ICA,and underwent neuronavigation⁃assisted endoscopic endonasal approach resection of the lesion.Postoperative pathology confirmed that the lesion was cholesterol granuloma Preoperative axial T2WI showed a mass of abnormal signal shadow could be seen in the left apex of petrous part area,high and low mixed signals,slightly protruding to the left CPA area. The boundary was still clear,with a size of about 2.40 cm×3.60 cm×2.50 cm(arrow indicates,Panel 4a). Preoperative sagittal T1WI showed heterogeneous short T1signal of the lesion (arrow indicates,Panel 4b). Histopathological examination showed coagulation tissue surrounding by fibrous connective tissue,hemosiderin deposition,cholesterol crystallization, and a small amount of lymphomonocyte infiltration were seen,which was in line with cholesterol granuloma (Panel4c). HE staining × 100 Axial T2WI 3 months after operation showed flake long T2signal shadow in the operation area(arrow indicates,Panel 4d). Sagittal T1WI 3 months after operation showed flake short T1 signal shadow in the operation area(arrow indicates,Panel 4e).
讨 论
岩斜区病变的传统手术入路为经侧方入路,主要包括经颞骨入路和经颅中窝入路。需保留患侧听力时,通常选择经迷路下入路、经耳蜗下入路和经颅中窝入路;而无保留患侧听力要求的患者,则选择经迷路入路[5⁃6]。经侧方入路过程中常遇到许多重要解剖结构,包括颈内动脉岩骨段、第Ⅱ~ Ⅵ对脑神经、海绵窦等,手术创伤大、并发症多[2],而且岩斜区胆固醇肉芽肿等囊性病变,术后难以长期保持良好的引流通道[5]。此外,经侧方颞骨入路还受颞骨气化程度的影响,术中存在前庭蜗神经和面神经损伤之风险,而经颅中窝入路手术难度大,术中对脑组织的牵拉难以避免地造成一定程度的脑组织损伤[6]。
1977 年,Montgomery[7]首次报告显微镜下经鼻入路手术切除岩斜区病变,并提出该入路适用于进展至蝶窦的胆固醇肉芽肿等囊性病变,但在未向内侧生长的其他岩斜区病变的处理上则较为困难。此后的一段时间内,该入路主要用于岩斜区胆固醇肉芽肿的外科手术。1994年,Fucci等[8]采用内镜下经鼻入路手术切除岩斜区胆固醇肉芽肿并获得成功。此后,随着内镜设备和内镜技术的进步、对内镜下颅底解剖学研究的深入以及术中神经导航系统和超声定位技术的应用,内镜下经鼻入路逐步应用于其他岩斜区病变的治疗。1999年,Goravalingappa等[9]对蝶岩斜复合体进行内镜下和显微镜下解剖学研究,揭示其神经血管三维解剖关系。2004 年,Jho和 Ha[10]提出,内镜下经鼻入路向侧方的手术范围并不局限于颈内动脉,还可显露至卵圆孔、圆孔、岩部尖和颈内静脉球。2007年,Herzallah和Casiano[11]将内镜手术中涉及的颈内动脉分为岩骨段、破裂孔段、斜坡旁段、海绵窦段和鞍旁段,并提出可以将翼管神经作为定位颈内动脉破裂孔段的标记。
2009 年 ,Zanation 等[6]将 内 镜 下 经 鼻 入 路 切 除岩斜区病变的手术入路进一步分为内侧入路、颈内动脉侧化的内侧入路和经翼突岩下入路。这3种入路的选择主要依据肿瘤性质、肿瘤与颈内动脉位置关系和肿瘤向内侧扩展程度。当病变位于岩部尖内侧或囊性病变向内侧扩展且蝶窦气化良好时,可采用内侧入路经蝶窦达病变部位,该入路技术难度最低、风险最小。对于位于斜坡后上方的病变,可经该入路采用硬膜外垂体移位技术进行有效显露。当蝶窦气化不良、病变较少向内侧扩展或位于颈内动脉后侧方时,脑干与颈内动脉斜坡旁段之间的空间狭小,需磨除颈内动脉沟骨质,将其内的颈内动脉向侧方移位以提供更开阔的入路空间。磨除颈内动脉沟骨质时应注意采用蛋壳化骨质磨除技术,即先将颈内动脉表面骨质磨成纤薄骨片,再以咬骨钳小心剥除,最大限度减少对颈内动脉的损伤。尽管既往认为脑干与颈内动脉斜坡旁段之间的空间是经鼻入路手术的相对禁区,但神经导航系统的应用以及经验丰富的手术团队可使该入路的风险可控。对于经内侧入路和颈内动脉侧化的内侧入路难以到达的部分病变,经翼突岩下入路可能更加合适,经该入路可沿颈内动脉岩骨段下表面磨除岩部尖骨质,充分显露肿瘤,但该入路难度较大,对手术技术要求较高。
有文献报道,开颅经颞骨入路手术切除岩斜区病变的症状缓解率为77%~ 84%,非计划二次手术率约为9.6%,前庭蜗神经和面神经损伤、脑脊液漏、颈内动脉损伤等并发症发生率约为32%[12⁃14];内镜下经鼻入路手术切除岩斜区病变的症状缓解率约84%,症状性胆固醇肉芽肿复发率约7.5%,鼻衄、慢性蝶窦炎、脑脊液漏、短暂性面神经麻痹等并发症发生率约 13%[15⁃17]。本研究除1例(例1)术前视物重影症状术后未缓解外,余5例术前症状均不同程度缓解;术后3个月内无一例患者出现脑脊液漏、中枢神经系统感染、脑神经损伤等并发症,未行非计划二次手术,无死亡病例;截至末次随访,无一例患者病变复发。
综上所述,内镜下经鼻入路岩斜区病变切除术相对安全、有效。该入路具有以下优点:(1)充分利用人体自然孔道达到减少手术创伤、微侵袭的目的。(2)经前方入路手术可保留前庭蜗神经和面神经功能。(3)神经内镜自身具有能够局部抵近放大观察、灵活变换角度的优势。(4)手术和住院时间短,术后恢复迅速。(5)头面部无瘢痕,美容效果较好,患者在心理上更易接受。(6)术后可在门诊进行内镜下观察和随访,对于术后引流通道轻度梗阻的患者可方便进行再通。本研究亦存在不足之处:(1)作为单中心回顾性研究,存在研究对象选择偏倚等固有缺陷。(2)均由同一术者施行手术,受其手术技术的影响较大。(3)样本量较小。今后尚待纳入更多样本并开展更全面的临床研究。
利益冲突 无