Application of Kaiser Sepsis Calculator in culture-positive infants with early onset sepsis
Gretchen Kopec 1 · Marc Collin 2 · Anirudha Das 3
Abstract
Keywords Early onset sepsis · EOS · Kaiser Sepsis Calculator · Neonatal sepsis · Neonate · Newborn · Blood culture
Introduction
Neonatal early onset sepsis (EOS) is defined as a bloodstream or central nervous system infection occurring within the first 3 days of life [ 1]. With the advent of intrapartum antibiotic prophylaxis (IAP) for Group B streptococcus (GBS) colonization, the incidence of EOS has decreased, from 3-4 per 1000 live births to < 0.5 per 1000 live births [ 2- 4] EOS leads to Neonatal Intensive Care admission in 60% of term infants and 2-3% of infants ≥ 35 weeks die [ 1, 2, 5]. Despite the institution of GBS intrapartum antibiotic prophylaxis (IAP) in 2002, GBS remains the number one pathogen in EOS at 36%, followed closely byEscherichia coli(E Coli) at 25% [ 5].
The 2010 Center for Disease Control and Prevention(CDC) guidelines and 2012 guidelines by the Committee on the Fetus and Newborn (COFN) guidelines on early onset sepsis were the commonly used guidelines for EOS in newborns in the past [ 6, 7]. In 2011, a team of experts from Kaiser Permanente, using Bayesian risk assessment tools in > 600,000 live births, developed two models. An objective risk score generated from the gestational age, highest maternal antepartum temperature, GBS carriage status, duration of rupture of membranes, and timing of intrapartum antibiotic administration and a second model that adjusts the baseline risk depending on the clinical presentation of the infant at birth, forming the basis for new guidelines [ 8- 11].
Although the adoption of this new risk-based intervention is reported to reduce the use of antibiotics, laboratory testing,there are some concerns for the missed cases of EOS who present with clinical symptoms at a later time after birth, leading to a potential delay in the initiation of antibiotic therapy [ 12- 16].
We sought to apply the Kaiser Sepsis Calculator (KSC) risk assessment score for culture-positive infants with EOS retrospectively in infants born in the last 10 years in our hospital.
Methods
In this retrospective cohort study, all cases of culture proven early onset sepsis were obtained from Jan 2009 to May 2018 from the Neonatal Intensive Care Unit(NICU) and newborn nursery at MetroHealth Medical Center (MHMC), Cleveland, Ohio. EOS was defined as isolation of bacteria from the blood within 72 hours of birth and continuation of antibiotics for at least 5 days by the treatment team [ 17]. All infants who were born at MHMC between 35 and 42 completed weeks of gestation were included in the study. Centers for Disease Control and Prevention (CDC) guidelines were consistently followed by the unit during the 10-year study period to manage EOS in newborns. Infants were excluded if they were born outside of the hospital or if their blood culture was drawn after 3 days of life. Data were collected from the electronic medical record on demographics, maternal intrapartum conditions, and therapies, chorioamnionitis,NICU, and Nursery sepsis therapies, and pertinent laboratory values.
The online KSC was used ( https:// www. neona talse psisc alcul ator. kaise rperm amente. org) to enter maternal risk factors with a prior risk of 0.3/1000 live births [per Centers for Disease Control and Prevention (CDC) rates]. The EOS risk was determined from both the baseline risk factors and the adjusted score after the initial clinical examination of the infant. The default threshold for recommendation of antibiotic treatment (≥ 3 per 1000 births) was used according to the composite EOS risk stratification based on the online sepsis calculator, divided into no culture/antibiotics, blood culture/no antibiotics, empiric antibiotics or a score of < 3 with clinical illness where antibiotics should be strongly considered to determine the need for antibiotics. Based on whether antibiotics were recommended based on KSC score, patients were divided into Group A, no antibiotics were recommended (hereafter called as“no-antibiotics”) and Group B, antibiotics were recommended (hereafter called “antibiotics”) (Fig. 1). Data were analyzed using SPSS (SPSS, 2017). APvalue of < 0.05 was considered statistically significant.
Results
A total of 25,688 infants were born in the study period.Overall, 49/25688 (1.9/1000) had positive blood culture,of which 25/49 (51%) were contaminants. Cases were excluded as contaminants based on organisms, number of positive cultures, symptomatology, and NICU team/infectious disease specialist documentation. A total of 24/25,688 (0.93/1000) cultures were considered EOS (Fig. 1). Out of them, 17/24 (71%) were assigned to the Group B (antibiotic group), while 7/24 (29%) were in the Group A (no-antibiotic group) (Table 1). All 24 infants were started on antibiotics per CDC guidelines,soon after birth, per existing guidelines in the hospital.Cases were determined to be contaminants based on organisms, number of positive cultures, symptomatology, and infectious disease specialist recommendation.
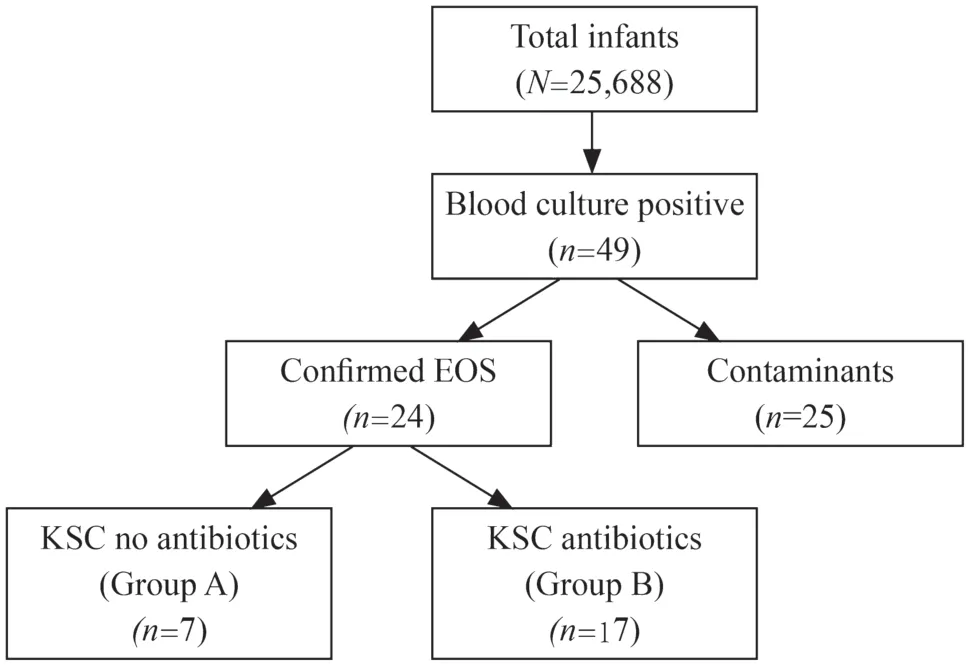
Fig. 1 Flow diagram showing the inclusion and exclusion of cases of early onset sepsis. EOS early onset sepsis, KSC Kaiser Sepsis Calculator
The initial early onset sepsis (EOS) risk between the groups was not significantly different (no-antibiotics vs. antibiotics = 0.76,P= 0.41). After considering the clinical presentation, the final EOS risk score was significantly different between the groups, no-antibiotics, 0.33 vs antibiotics, 9.41(P< 0.001). In the no-antibiotics group, 4/7 infants were never symptomatic, while 3/7 were symptomatic at 9, 25, and 42 h,respectively. This is significantly different from the antibiotics group, where all infants were symptomatic at an average of 4.4 h after birth. In this group, the minimum time to become symptomatic was immediately after birth for 9 infants, out of which 7 had risk scores < 3/1000, while the rest were symptomatic after 2-23 h.Escherichia coli(E. coli) was the predominant organism isolated in the no-antibiotic group, 4/7 (57.1%),whileGroup Bstreptococcus(GBS), 6/17 (35.2%) andCoagulase-negativestaphylococcus(CONS), 4/17 (23.5%) were the main organisms isolated from the blood cultures in the antibiotics group (Table 2). In the non-antibiotics group, all infants were discharged, while one infant died in the antibiotics group. The infant had sepsis due to CONS.
Discussion
The study demonstrated that in contrast to the CDC guidelines, KSC scores would not have recommended starting antibiotics on the initially asymptomatic infants who became symptomatic later or never so. In this study, since all infants presenting late received antibiotics according to the CDC guidelines, it is impossible to determine retrospectively if the outcome would have been different had the antibiotics not been started initially. Since, the final KSC score depends on subjective components like persistent tachycardia, tachypnea and assessment of respiratory distress, there is a potential for delay in starting antibiotics while using KSC.

Table 1 A detailed description of patients characteristics in the Groups A and B
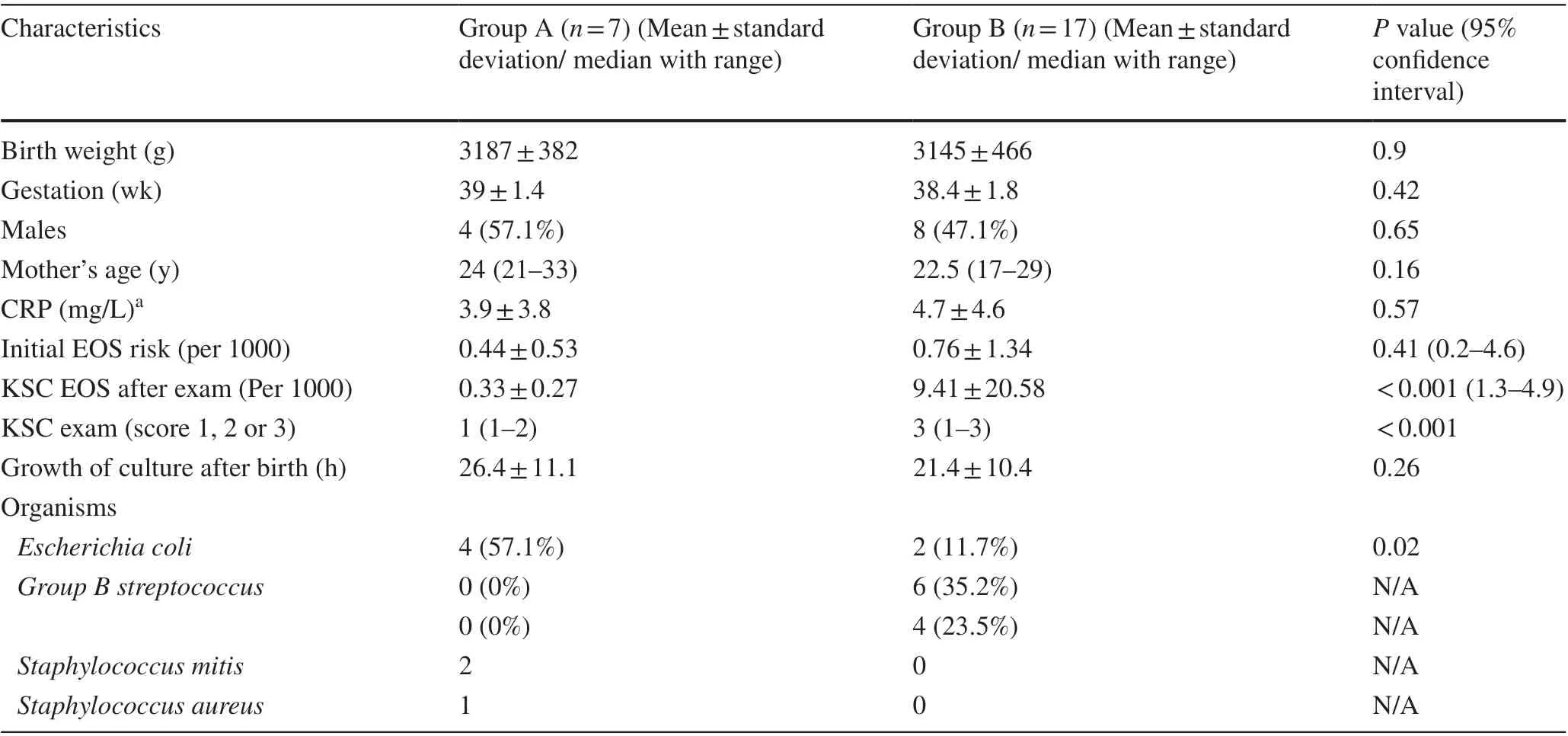
Table 2 Differences in characteristics between the Group A (no-antibiotics) and Group B (antibiotics)
The rate of EOS in this study was similar to previous studies [ 2, 17]. Wortham found that 87% of the infants whose mothers were diagnosed with chorioamnionitis developed symptoms within 6 hours after birth. That leaves a significant number (13%) of babies who became symptomatic later [ 17]. In this study, 6/7 infants who were asymptomatic initially and would not have received antibiotics per KSC recommendations, either never developed any symptoms or developed symptoms after 24 hours demonstrating the need for close clinical monitoring.
Numerous studies have identified GBS to be the most common organism related to EOS in term infants andE. coliin preterm and very low birth weight (VLBW) infants [ 18]. In our study, the KSC recommended correctly to start antibiotics in all cases of GBS sepsis but only in 2/6 cases ofE. colisepsis.This difference in the presentation of the two organisms cannot be attributed to gestational age (38 weeks and 4 days vs.38 weeks). The estimated risk for mortality inE. colisepsis is higher (6-10%) compared to GBS (2-3%) EOS suggesting a difference in virulence and possibly presentation [ 2]. Although,the sample size in this study was not powered to show a significant difference, the authors consider this finding important.
Prior studies in adults have demonstrated the importance of starting antibiotics early in sepsis for improved outcomes [ 19, 20]. Weiss et al. showed that delay in antibiotic therapy is an independent risk factor for prolonged organ dysfunction and mortality in pediatric patients admitted to the pediatric intensive care unit (PICU) [ 21].Implementation of KSC has led to decrease in blood culture at birth and initial antibiotic use substantially [ 22].Early use of antibiotics can lead to gut dysbiosis and immunological alteration which has the potential for longterm adverse effects [ 23, 24]. But, at the same time, delay in commencement of antibiotics while following the KSC recommendation has raised some concerns. Rajbhandari noted that 75% of culture-positive cases of sepsis in the study by Kuzniewicz et al. would not have received antibiotics at birth based on the KSC [ 16]. Hooven, while analyzing data from 6 studies published between 2003 and 2017, found three infants who may have been harmed related to the delayed start of antibiotics and therefore deduced that the number needed to harm was 1/1610 in those infants at risk for EOS [ 13]. Sloane et al. emphasized the need for enhanced and prolonged observation of neonates based on concerns about delay in antibiotic therapy[ 25]. In our study, none of the infants who presented late had unfavorable outcomes potentially because of early antibiotic use based on the existing CDC criteria. Many of these infants developed symptoms later suggesting that potentially higher morbidity and possible mortality would have resulted if antibiotic therapy was delayed.
The major limitation of the study is its retrospective nature and a low number of subjects. Retrospective chart review to look for signs and symptoms of EOS may also be unreliable due to a lack of KSC recommended protocol for observation at the time of the study.In conclusion, a significant number of infants that would not be on antibiotics per KSC guidelines presented later even on antibiotic therapy which indicates the need for prolonged observation of these infants. The clinical presentation ofE.coliEOS may differ from GBS which requires further investigation. Larger studies and long-term follow-up are needed to evaluate the potential effect of delayed initiation of antibiotics because of the adoption of KSC.
Author contributionsKG: conceptualization, methodology, data curation, writing-original draft preparation. CM: methodology, visualization, reviewing and editing. DA: conceptualization, methodology, statistical analyses, reviewing and editing and supervision.
FundingNo funding was received for the study.
Data availability statementThe datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Compliance with ethical standards
Ethical approvalThe study was approved by the Institutional Review Board of MetroHealth Medical Center, Cleveland, Ohio. The study number is IRB17-00371. Since this is a retrospective chart review,the need for informed consent was waived by the Institutional Review Board.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
 World Journal of Pediatrics2021年4期
World Journal of Pediatrics2021年4期
- World Journal of Pediatrics的其它文章
- Similarities and differences between multiple inflammatory syndrome in children associated with COVID-19 and Kawasaki disease: clinical presentations, diagnosis, and treatment
- Extent, reasons and consequences of off-labeled and unlicensed drug prescription in hospitalized children: a narrative review
- Clinical characteristics of COVID-19 in family clusters: a systematic review
- Cerebral palsy in children born after assisted reproductive technology:a meta-analysis
- Characteristics of immune and inflammatory responses among different age groups of pediatric patients with COVID-19 in China
- Impact of probiotics supplement on the gut microbiota in neonates with antibiotic exposure:an open-label single-center randomized parallel controlled study
