经脐单孔腹腔镜全子宫切除术不同途径缝合阴道残端的研究
周明辉?纪燕琴?邱华娟
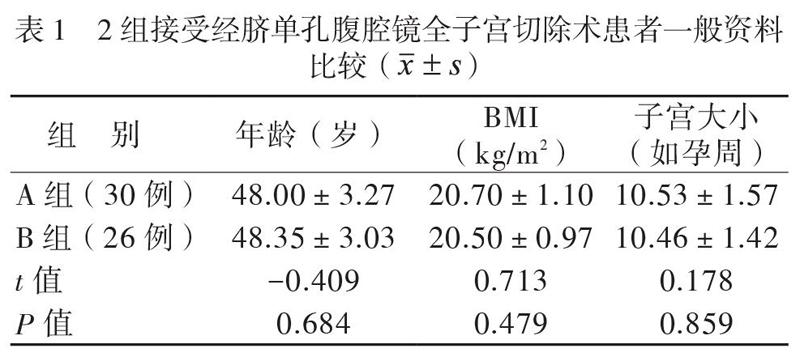

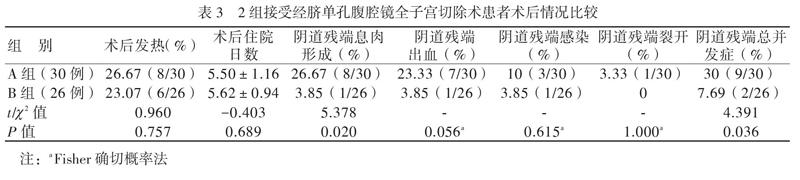
【摘要】目的 比較经脐单孔腹腔镜全子宫切除术采用倒刺线经不同途径缝合阴道残端的效果。方法 选取因子宫良性疾病接受经脐单孔腹腔镜全子宫切除术患者56例。56例均采用倒刺线缝合,经腹腔镜缝合阴道残端者被纳入A组(30例),经阴道缝合阴道残端者被纳入B组(26例)。比较2组的术中失血量、手术操作时间、术后住院日数、阴道残端总并发症(术后阴道残端出血、阴道残端感染、阴道残端裂开)、术后阴道残端息肉形成率。结果 2组均能顺利完成单孔腹腔镜全子宫切除术。A组手术操作时间和缝合时间均少于B组(P均< 0.05)。术后A组出现1例阴道残端裂开,B组则无(P > 0.05)。A组术后阴道残端息肉形成率高于B组(P < 0.05)。A组术后阴道残端总并发症发生率高于B组(P < 0.05),但2组术后阴道残端出血、阴道残端感染、阴道残端裂开发生率差异则无统计学意义(P均> 0.05)。结论 经脐单孔腹腔镜全子宫切除术采用倒刺线经腹腔镜缝合阴道残端有利于阴道残端的愈合,可降低术后残端并发症发生率。
【关键词】单孔腹腔镜;全子宫切除术;阴道残端缝合;单向倒刺线
Study of different methods of suture of vaginal stump in transumbilical single-port laparoscopic total hysterectomy Zhou Minghui, Ji Yanqin, Qiu Huajuan. Department of Gynecology, Huizhou Municipal Central Hospital, Huizhou 516001, China Corresponding author, Ji Yanqin
【Abstract】Objective To compare the effect of different methods of suturing vaginal stump with barbed thread in transumbilical single-port laparoscopic total hysterectomy. Methods A total of 56 patients with benign uterine diseases who underwent transumbilical single-port laparoscopic total hysterectomy were selected in this study. All 56 patients were sutured with barbed thread. Patients undergoing laparoscopic suture of vaginal stump were allocated into group A (n = 30), and those receiving transvaginal suture of vaginal stump were assigned into group B (n = 26). The intraoperative blood loss, operation time, length of postoperative hospital stay, total vaginal stump complications (postoperative vaginal stump bleeding, vaginal stump infection and vaginal stump dehiscence) and incidence of postoperative vaginal stump polyps were statistically compared between two groups. Results All patients in both groups successfully completed single-port laparoscopic total hysterectomy. The operation time and suture time in group A were significantly shorter than those in group B (both P < 0.05). In group A, 1 patient presented with vaginal dehiscence and no vaginal dehiscence in group B (P > 0.05). The incidence of postoperative vaginal stump polyps in group A was considerably higher than that in group B (P < 0.05). In group A, the incidence of vaginal stump complications was significantly higher than that in group B (P < 0.05), whereas the incidence of vaginal stump bleeding, vaginal stump infection and vaginal dehiscence did not significantly differ between two groups (all P > 0.05). Conclusion Transumbilical single-port laparoscopic total hysterectomy via laparoscopic suture of vaginal stump is beneficial to the healing of vaginal stump and reduces the incidence of postoperative vaginal stump complications.
讨论
腹腔镜手术近年来备受妇科医师和患者的青睐,但术后腹部皮肤难免会留下3 ~ 4个小瘢痕,影响美观。经脐单孔腹腔镜由于利用了脐部作为手术切口,脐部皱褶可掩盖瘢,美观效果明显优于传统多孔腹腔镜[5]。经脐单孔腹腔镜全子宫切除术与传统多孔腹腔镜全子宫切除术相比,中转开腹率、围术期并发症发生率无明显差别,且患者术后活动更早、疼痛更轻,表明经脐单孔腹腔镜全子宫切除是安全的[3, 6-7]。本研究中所有患者均顺利完成手术,无1例中转开腹,无发生肠管、膀胱损伤。
缝合是经脐单孔全子宫切除术的难点,本研究中所有患者均用0号V-LOC线缝合,其具有免打结、无需助手固定、溶解延迟等特点,能有效降低手术难度、缩短手术时间、降低阴道残端并发症发生率[8-11]。经阴道缝合能降低经脐单孔腹腔镜全子宫切除术的难度,缩短手术时间,本研究经腹腔镜缝合患者的总手术时间和缝合时间均长于经阴道缝合患者,与王晓樱等[3]的研究结果相似。
对于阴道残端是经阴道缝合还是经腹腔镜缝合更有利于阴道残端愈合,目前尚无定论。一些回顾性研究显示经阴道缝合能降低阴道裂开、肠管脱出风险,并提出这可能是由于经阴道缝合的打结力度要大于经腹腔镜缝合所致[12-15]。也有报道称阴道残端裂开的发生率与阴道残端缝合方法并无影响[16]。本研究结果显示,2组术后发热、术后住院日数以及术后残端出血、裂开、感染率均无差异,但2组术后阴道残端息肉形成和阴道残端总并发症发生率有差异,阴道残端总并发症发生率结果与Uccella等[4]的前瞻性随机对照试验结果相似,这可能与腹腔镜技术的提高、使用0号V-LOC线缝合、经腹腔镜缝合有助于较好地缝合腹膜(即使仅缝合后腹膜),更好地对合阴道黏膜、封闭阴道以及减少渗出等有关。
阴道残端的缝合是单孔腹腔镜全子宫切除术的难点,经腹腔镜缝合更是困难,我们的经验是膀胱下推应该更充分,留有足够的阴道残端,便于缝合。经阴道缝合可以降低手术难度,但也存在缺点,阴道黏膜难于对合会造成阴道残端黏膜不平整,增加术后阴道残端并发症发生率。而经腹腔镜缝合,可以将阴道黏膜对合整齐,同时可以将骶韧带缝合固定于阴道,恢复阴道残端的轴向,可能降低术后阴道残端脱垂风险。在本研究中,经腹腔镜缝合虽需时较长,但其术后阴道残端息肉形成和阴道残端并发症发生率更低,与刘维等[17]的报道相近。
综上所述,经脐单孔腹腔镜全子宫切除术经腹腔镜缝合阴道残端有利于阴道残端的愈合,降低术后阴道残端并发症发生率。本研究存在样本量小、非前瞻性研究等缺陷,结论有待大样本的、前瞻性的研究进一步验证。
参考文献
[1] 赵洪霞, 张新艳.单孔腹腔镜在妇科良性疾病中的临床应用.中国实用医药,2020,15(24):25-27.
[2] Matthews CA. Minimally invasive sacrocolpopexy: how to avoid short-and long-term complications. Curr Urol Rep,2016,17(11):81.
[3] 王曉樱,李妍.单孔腹腔镜全子宫切除术临床疗效分析.中国现代手术学杂志,2019,23(3):215-219.
[4] Uccella S, Malzoni M, Cromi A, Seracchioli R, Ciravolo G, Fanfani F, Shakir F, Gueli Alletti S, Legge F, Berretta R, Corrado G, Casarella L, Donarini P, Zanello M, Perrone E, Gisone B, Vizza E, Scambia G, Ghezzi F. Laparoscopic vs transvaginal cuff closure after total laparoscopic hysterectomy: a randomized trial by the italian society of gynecologic endoscopy. Am J Obstet Gynecol,2018,218(5):500.e1-500.e13.
[5] 黄晓斌, 柳晓春, 郑玉华.经脐单孔腹腔镜手术治疗卵巢良性肿瘤的研究.新医学, 2015, 46(7):482-485.
[6] Sandberg EM, la Chapelle CF, van den Tweel MM, Schoones JW, Jansen FW. Laparoendoscopic single-site surgery versus conventional laparoscopy for hysterectomy: a systematic review and meta-analysis. Arch Gynecol Obstet,2017,295(5):1089-1103.
[7] Yang L, Gao J, Zeng L, Weng Z, Luo S. Systematic review and meta-analysis of single-port versus conventional laparoscopic hysterectomy. Int J Gynaecol Obstet,2016,133(1):9-16.
[8] 干晓琴, 林海, 刘江, 张凌, 张强, 黄利琼, 张家佳. Ⅴ-Loc倒刺线在腹腔镜下子宫腺肌瘤剥除术中的应用效果观察.中国计划生育和妇产科,2016,8(7):54-56,62.
[9] Rettenmaier MA, Abaid LN, Brown JV 3rd, Mendivil AA, Lopez KL, Goldstein BH. Dramatically reduced incidence of vaginal cuff dehiscence in gynecologic patients undergoing endoscopic closure with barbed sutures: a retrospective cohort study. Int J Surg,2015,19:27-30.
[10] Smith K, Caceres A. Vaginal cuff closure in minimally invasive hysterectomy: a review of training, techniques, and materials. Cureus, 2017, 9(10):e1766.
[11] Cong L, Li C, Wei B, Zhan L, Wang W, Xu Y. V-Loc? 180 suture in total laparoscopic hysterectomy: a retrospective study comparing Polysorb to barbed suture used for vaginal cuff closure. Eur J Obstet Gynecol Reprod Biol,2016,207:18-22.
[12] Nezhat C, Kennedy Burns M, Wood M, Nezhat A, Nezhat F. Vaginal cuff dehiscence and evisceration: a review. Obstet Gynecol,2018,132(4):972-985.
[13] Lee SH, Oh SR, Cho YJ, Han M, Park JW, Kim SJ, Yun JH, Choe SY, Choi JS, Bae JW. Comparison of vaginal hysterectomy and laparoscopic hysterectomy: a systematic review and meta-analysis. BMC Womens Health,2019,19(1):83.
[14] Teoh D, Lowery WJ, Jiang X, Ehrisman J, Halvorson P, Broadwater G, Bentley R, Secord AA, Sobolewski C, Berchuck A, Havrilesky LJ, Valea FA, Lee PS. Vaginal cuff thermal injury by mode of colpotomy at total laparoscopic hysterectomy: a randomized clinical trial. J Minim Invasive Gynecol,2015,22(2):227-233.
[15] Due?as-Garcia OF, Sullivan GM, Leung K, Billiar KL, Flynn MK. Knot integrity using different suture types and different knot-tying techniques for reconstructive pelvic floor procedures. Int Urogynecol J,2018,29(7):979-985.
[16] Das D, Sinha A, Yao M, Michener CM. Trends and risk factors for vaginal cuff dehiscence after laparoscopic hysterectomy. J Minim Invasive Gynecol,2020,S1553-4650(20)30883-30889.
[17] 劉维,李梅,黄淑贞.腹腔镜下全子宫切除术中阴道残端经镜下及经阴道缝合对患者预后的影响观察.基层医学论坛, 2017, 21(10):1162-1163.
(收稿日期:2021-01-29)
(本文编辑:洪悦民)

