单中心急性前循环大血管闭塞性醒后脑卒中血管内治疗有效性与安全性研究
王立志?朱晔宁?邓宇平?李朱勤?刘武

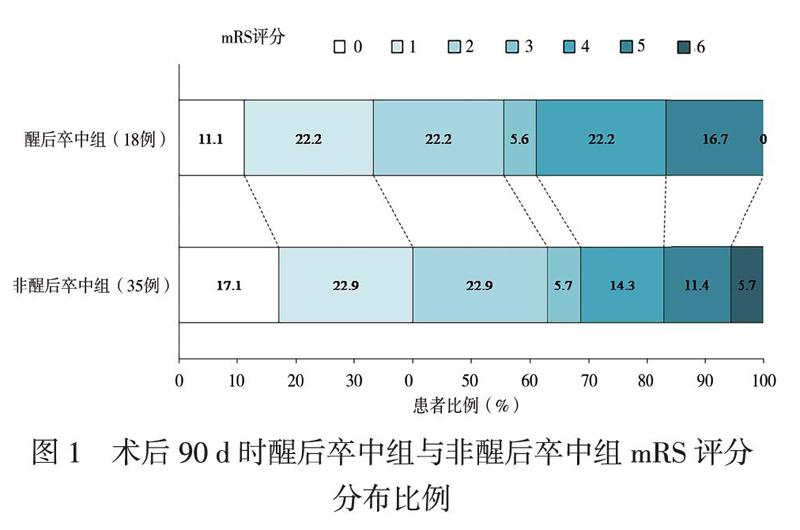
【摘要】目的 探討急性前循环大血管闭塞性醒后脑卒中血管内治疗的安全性及有效性。方法 收集急性前循环大血管闭塞性缺血性脑卒中患者,以CT血管成像(CTA)证实颈内动脉或大脑中动脉M1段闭塞、Alberta脑卒中项目早期CT(ASPECT)评分≥6分及美国国立卫生研究院卒中量表(NIHSS)评分≥6分为主要入组标准,以术后24 h及术后7 d NIHSS评分评估患者神经功能缺损改善程度,以术后90 d改良Rankin量表(mRS)评分评估患者预后。按发病时间分为醒后卒中组和非醒后卒中组,比较2组基线资料、手术相关特征、术后脑出血率、术后90 d病死率、术后24 h及术后7 d NIHSS评分、术后90 d预后良好患者比例。结果 共纳入53例急性前循环大血管闭塞性缺血性脑卒中患者,其中醒后卒中组18例、非醒后卒中组35例。醒后卒中组与非醒后卒中组的年龄、性别构成、脑卒中危险因素、入院NIHSS评分、脑卒中病因学分型、ASPECT评分比较差异均无统计学意义(P均> 0.05)。醒后卒中组术前静脉溶栓患者的比例低于非醒后卒中组(11% vs. 57%,P < 0.05),2组的入院至穿刺时间、责任血管、血管内治疗方式、血管再通率、术后脑出血率、术后90 d病死率比较差异均无统计学意义(P均> 0.05)。醒后卒中组和非醒后卒中组术后24 h及术后7 d NIHSS评分均比入院时下降(P均< 0.025),2组间入院时、术后24 h及术后7 d NIHSS评分比较差异均无统计学意义(P均> 0.05)。术后90 d时醒后卒中组预后良好患者占56%(10/18),非醒后卒中组预后良好患者占63%(22/35),组间比较差异无统计学意义(P > 0.05)。结论 部分急性前循环大血管闭塞性醒后脑卒中血管内治疗安全、有效。
【关键词】醒后脑卒中;血管内治疗;机械取栓;预后
Efficacy and safety of endovascular therapy for wake-up stroke with acute large vessel occlusion of anterior circulation in a single stroke center Wang Lizhi, Zhu Yening, Deng Yuping, Li Zhuqin, Liu Wu. Department of Neurology, Huizhou Municipal Central Hospital, Huizhou 516001, ChinaCorresponding author, Liu Wu, E-mail: orangeliuwu@ 163. com
【Abstract】Objective To evaluate the safety and efficacy of endovascular therapy for wake-up stroke with acute large vessel occlusion of the anterior circulation. Methods Ischemic stroke patients with acute large vessel occlusion of the anterior circulation who were treated with endovascular therapy were retrospectively recruited. The occlusion of internal carotid artery or M1 segment of the middle cerebral artery was diagnosed by computer tomography angiography (CTA), Alberta Stroke Program Early CT (ASPECT) score≥6 and National Institute of Health Stroke Scale (NIHSS) score≥6 were used as the primary inclusion criteria. The NIHSS scores at 24 h and 7 d after operation were utilized to evaluate the improvement of neurological deficit. The modified Rankin Scale (mRS) score at 90 d after operation was used to evaluate clinical prognosis. All patients were divided into the wake-up stroke group and non-wake-up stroke group according to the time of onset. The baseline data, features of operation, cerebral hemorrhage rate after operation, mortality rate at 90 d after operation, NIHSS scores at 24 h and 7 d after operation, proportion of patients with good prognosis at 90 d after operation were statistically compared between two groups. Results A total of 53 ischemic stroke patients with acute large vessel occlusion of the anterior circulation were enrolled, including 18 patients in the wake-up stroke group and 35 patients in the non-wake-up stroke group. Age, gender, stroke risk factors, NIHSS score on admission, stroke etiology classification and ASPECT score did not significantly differ between two groups (all P > 0.05). The proportion of patients with preoperative intravenous thrombolysis in the wake-up stroke group was remarkably lower than that in the non-wake-up stroke group (11% vs. 57%;P < 0.05). The door-to-puncture time, responsible vessel, protocol of endovascular therapy, vascular recanalization rate, cerebral hemorrhage rate after operation and mortality rate at 90 d after operation did not significantly differ between two groups (all P > 0.05). In both groups, the NIHSS scores at 24 h and 7 d after operation were considerably lower than those upon admission (all P < 0.025). The NIHSS scores at postoperative 24 h and 7 d did not significantly differ between two groups (both P > 0.05). In the wake-up stroke group, 56% (10/18) patients obtained good prognosis at 90 d after operation, which did not significantly differ from 63% (22/35) in the non-wake-up stroke group (P > 0.05). Conclusion Endovascular therapy is safe and effective for partial wake-up stroke patients with acute large vessel occlusion of the anterior circulation.
【Key words】Wake-up stroke;Endovascular therapy;Mechanical thrombectomy;Prognosis
醒后脑卒中是指入睡时完全正常或无新发卒中症状但在醒来时发现新发神经功能缺损症状的急性缺血性脑卒中,约占所有缺血性脑卒中的25%[1]。2015年以来的多项大样本、多中心随机对照研究显示,在经过筛选的急性前循环大血管闭塞性缺血性脑卒中患者中,以机械取栓为主的血管内治疗可带来明确获益[2]。因此,特定急性前循环大血管闭塞性缺血性脑卒中的血管内治疗被指南列为最高级别推荐[3]。但血管内治疗主要针对的是发病时间明确的缺血性脑卒中,针对醒后脑卒中的血管内治疗研究较少[4]。为此,本研究探讨急性前循环大血管闭塞性醒后脑卒中血管内治疗的安全性及有效性,现报告如下。
对象与方法
一、研究对象
回顾性纳入2019年10月至2020年10月在惠州市中心人民医院神经内科接受血管内治疗的急性前循环大血管闭塞性缺血性脑卒中患者。纳入标准:①符合《中国急性缺血性脑卒中诊治指南2018》的急性缺血性脑卒中诊断标准;②到院时距发病时间或最后正常时间≤24 h;③美国国立卫生研究院脑卒中量表(NIHSS)评分≥6分;④Alberta脑卒中项目早期CT(ASPECT)评分≥6分[6];⑤CT血管成像(CTA)证实缺血性脑卒中由颈内动脉或大脑中动脉M1段为责任动脉;⑥年龄≥18岁[5]。排除标准:①头颅CT或MRI提示大面积梗死(梗死面积> 1/3大脑中动脉供血区);②发病前改良Rankin量表(mRS)评分≥2分;③静脉溶栓后症状明显改善,NIHSS评分<6分;④存在手术禁忌证。纳入患者按发病时间是否明确,分为醒后卒中组和非醒后卒中组。研究方案经惠州市中心人民医院伦理委员会批准,患者或家属签署知情同意书。
二、研究方法
1. 临床资料收集
记录患者的年龄、性别、脑卒中危险因素[高血压、糖尿病、高脂血症、心房颤动、冠状动脉粥样硬化性心脏病(冠心病)、既往脑卒中或短暂性脑缺血发作病史、吸烟、饮酒]、入院时NIHSS评分、脑卒中病因学分型、ASPECT评分、责任血管、入院至穿刺时间(DPT)。
2. 治疗方案
急性缺血性脑卒中患者到达急诊后立即启动绿色通道,符合静脉溶栓指征且无禁忌证的患者先予以静脉溶栓治疗,符合条件的患者再予桥接血管内治疗;具有静脉溶栓禁忌证且符合血管内治疗指征的患者直接予血管内治疗。血管内治疗的方法:在局部麻醉辅以静脉药物麻醉或气管插管全身麻醉下进行,按Seldinger法穿刺右(左)侧股动脉,置入8F动脉鞘,首先行全脑血管造影确定责任血管,采用Revive SE取栓支架进行机械取栓或Penumbra血栓抽吸系统进行直接血栓抽吸或两者结合。
3. 血管再通的评价
血管再通为改良脑梗死溶栓分级(mTICI)2b/3级[6]。
4. 安全性指标
安全性指标包括血管内治疗后症状性脑出血转化率及术后90 d病死率。症状性脑出血的判定:术后0、4、24 h或临床症状恶化时行头颅CT检查,若发现颅内出血判定为术后脑出血,导致神经功能缺损加重(NIHSS评分升高≥4分)或死亡的为症状性脑出血。
5. 神经功能及预后评估
术后24 h及术后7 d评估患者NIHSS评分,分别与入院时NIHSS评分比较,评价患者神经功能缺损改善程度。术后第90 d通过门诊或电话随访获取患者mRS评分,mRS评分0 ~ 2分定义为预后良好,mRS评分3 ~ 6分定义为预后不良。
三、统计学处理
采用SPSS 25.0进行统计学分析。计量资料呈正态分布的用表示,组间比较采用独立样本t检验,组间入院时、术后24 h及术后7 d 的NIHSS评分比较采用重复测量资料方差分析,但因交互效应有统计学意义(F交互效应= 32.677,P < 0.001),故组内治疗前后NIHSS评分比较采用配对t检验,并用Bonferroni法校正检验水准,P < 0.05/2为差异有统计学意义,组间比较采用t检验。计数资料用例(%)表示,组间比较采用χ2检验或Fisher确切概率法。α = 0.05。
结果
一、醒后卒中組与非醒后卒中组患者基线资料比较
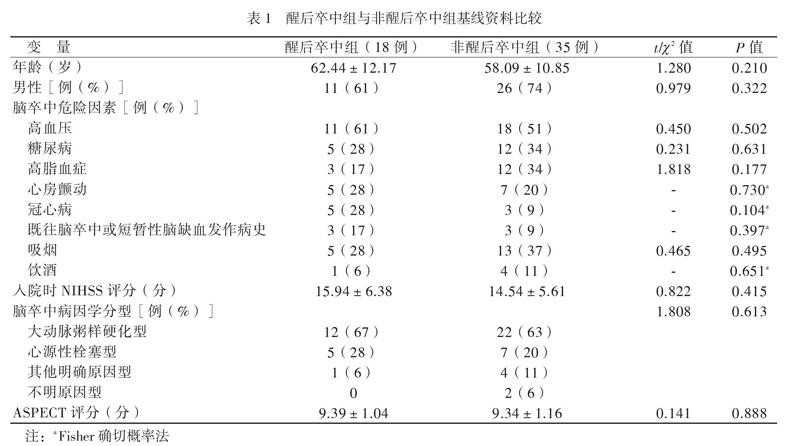
本研究共纳入急性前循环大血管闭塞性缺血性脑卒中患者53例,男37例、女16例,年龄(59.57±11.39)岁。其中醒后卒中组18例、非醒后卒中组35例,2组的年龄、性别构成、脑卒中危险因素、入院NIHSS评分、脑卒中病因学分型、ASPECT评分比较差异均无统计学意义(P均> 0.05),见表1。
二、醒后卒中组与非醒后卒中组手术相关特征比较
醒后卒中组2例(11%)患者术前接受了静脉溶栓治疗,非醒后卒中组20例(57%)患者术前接受了静脉溶栓治疗,醒后卒中组术前静脉溶栓患者的比例低于非醒后卒中组(P < 0.05)。2组间DPT、责任血管、血管内治疗方式、血管再通率比较差异均无统计学意义(P均> 0.05),见表2。
三、醒后卒中组与非醒后卒中组安全性指标比较
醒后卒中组与非醒后卒中组的术后脑出血率、术后90 d病死率比较差异均无统计学意义(P均> 0.05),见表3。
四、醒后卒中组与非醒后卒中组预后比较
与入院时NIHSS评分比较,醒后卒中组和非醒后卒中组术后24 h及术后7 d NIHSS评分均下降,术后7 d下降更为明显(P均< 0.025),2组入院时、术后24 h及术后7 d NIHSS评分比较差异均无统计学意义(P均> 0.05),见表4。术后90 d时mRS评分分布比例见图1,醒后卒中组预后良好患者占56%(10/18),非醒后卒中组预后良好患者占63%(22/35),组间比较差异无统计学意义(χ2 = 0.265,P = 0.607)。
分布比例
討论
缺血性脑卒中是我国主要的致死致残病因之一,醒后脑卒中是临床工作中不容忽视的脑卒中亚型之一。颅内外大血管闭塞导致的缺血性脑卒中病情严重、预后不良,致死致残率高。对于缺血性脑卒中,治疗的关键在于尽早再灌注治疗,目前证实有效的再灌注治疗方法主要是静脉溶栓治疗及血管内治疗[3, 7]。然而,静脉溶栓治疗对大血管闭塞导致的缺血性脑卒中效果欠佳,再通率仅为13% ~ 18%[8]。2015年公布的多项大样本、多中心随机对照研究为发病6 h内前循环大血管闭塞性缺血性脑卒中行血管内治疗提供了A级证据[2]。但这些研究针对的是发病时间明确的患者。2018年DAWN研究及DEFUSE-3研究结果的公布,将急性前循环大血管闭塞性缺血性脑卒中血管内治疗的时间窗延长至16 ~ 24 h,为醒后脑卒中患者的血管内治疗提供了依据[9-10]。本研究表明,经过筛选的急性前循环大血管闭塞性醒后脑卒中患者行血管内治疗的安全性和有效性与发病时间明确的缺血性脑卒中患者相当。
DAWN研究及DEFUSE-3研究均采用多模式影像评估筛选患者,但目前急诊多模式影像在我国基层医院尚未广泛开展,实际应用受到限制。ASPECT评分可量化评价缺血性脑卒中早期缺血改变,其可重复性强、评分标准化,临床应用广泛,部分随机对照试验采用ASPECT评分筛选血管内治疗的病例[11-12]。但基于平扫CT的ASPECT评分的可靠性存在一定争议,而基于CTA的ASPECT评分则灵敏度较高[13]。本研究显示,采用基于CTA的ASPECT评分筛选适合血管内治疗的急性前循环大血管闭塞性醒后脑卒中患者是安全的,血管再通率无降低,症状性脑出血转化率及90 d病死率均无增加,与李晖等[14]、 Konstas等[15]研究相一致。提示对于无法急诊完成CT灌注成像(CTP)的卒中中心,采用基于CTA的ASPECT评分是一种安全的急性前循环大血管闭塞性醒后脑卒中血管内治疗影像评估策略。
本研究中醒后卒中组术前静脉溶栓患者比例低于非醒后卒中组。虽然WAKE-UP研究发现,对存在头颅MRI扩散加权成像(DWI)-液体衰减反转恢复(FLAIR)序列不匹配的、发病时间未知的缺血性脑卒中患者进行静脉溶栓治疗,可改善这部分患者的90 d功能预后,但受急诊MRI检查未广泛开展等客观条件限制,仍有较多醒后脑卒中患者因发病时间不明确被排除在静脉溶栓治疗之外[16]。
DAWN研究的入组患者为6 ~ 24 h内急性前循环大血管闭塞性缺血性脑卒中患者,其中醒后脑卒中患者占55.3%(在机械取栓组中占62.6%,药物治疗组中占47.5%),结果显示机械取栓组90 d时mRS评分0 ~ 2分的患者比例明显高于药物治疗组(49% vs. 13%)[9]。因此DAWN研究对于指导醒后脑卒中血管内治疗意义较大。本研究显示,急性前循环大血管闭塞性醒后脑卒中患者血管内治疗术后24 h及术后7 d NIHSS评分均比入院时下降,术后7 d下降更为明显,醒后卒中组与非醒后卒中组入院时、术后24 h和术后7 d NIHSS评分及术后90 d预后良好患者的比例均相近,与王冬梅等[17]研究相一致。研究提示血管内治疗可改善急性前循环大血管闭塞性醒后脑卒中患者的神经功能缺损及预后,与发病时间明确的缺血性脑卒中患者疗效相当。本研究中醒后卒中组90 d预后良好患者比例(56%)略高于DAWN研究,可能与本研究样本量较小及纳入部分发病6 h内患者有关。
综上所述,经过筛选的急性前循环大血管闭塞性醒后脑卒中血管内治疗安全、有效。但本研究为单中心研究,样本量较小,未来需要大样本、多中心随机对照研究提供更多的循证医学证据。
参考文献
[1] Huang X, Alakbarzade V, Khandanpour N, Pereira AC. Management of a wake-up stroke. Pract Neurol, 2019, 19(4):326-331.
[2] Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG;HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet, 2016, 387(10029):1723-1731.
[3] Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL;American Heart Association Stroke Council. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke, 2018, 49(3):e46-e110.
[4] Alsahli K, Cheung AK, Wijesuriya N, Cordato D, Zagami AS, Wenderoth JD, Chiu AH, Tay K, Cappelen-Smith C. Thrombectomy in stroke of unknown onset, wake up stroke and late presentations: australian experience from 2 comprehensive stroke centres. J Clin Neurosci, 2019, 59:136-140.
[5] 中華医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018. 中华神经科杂志, 2018, 51(9):666-682.
[6] 中国卒中学会, 中国卒中学会神经介入分会, 中华预防医学会卒中预防与控制专业委员会介入学组. 急性缺血性卒中血管内治疗中国指南2018. 中国卒中杂志, 2018, 13(7):706-729.
[7] 姚麟, 连晓鹏, 秦冰. 急性缺血性脑卒中rt-PA静脉溶栓标准化诊疗流程实施效果分析. 新医学, 2015,46(10):702-705.
[8] Hasan TF, Todnem N, Gopal N, Miller DA, Sandhu SS, Huang JF, Tawk RG. Endovascular thrombectomy for acute ischemic stroke. Curr Cardiol Rep, 2019, 21(10):112.
[9] Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG;DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med, 2018, 378(1):11-21.
[10] Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG;DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med, 2018, 378(8):708-718.
[11] Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD;ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med, 2015, 372(11):1019-1030.
[12] Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Casta?o C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A;REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med, 2015, 372(24):2296-2306.
[13] ?zdemir A?, Ery?ld?z ES, Akarsu FG, Kocaba? ZU, Ayka? ?. The role of ASPECTs in patient selection for endovascular therapy-CTA source images versus noncontrast CT. J Clin Neurosci, 2020, 73:195-200.
[14] 李暉, 王硕, 李昌茂, 代成波, 黄思菲, 张斌. 血管内机械取栓治疗伴大动脉闭塞的醒后卒中疗效分析. 临床神经病学杂志, 2018, 31(6):465-468.
[15] Konstas AA, Minaeian A, Ross IB. Mechanical thrombectomy in wake-up strokes: a case series using alberta stroke program early CT score (ASPECTS) for patient selection. J Stroke Cerebrovasc Dis, 2017, 26(7):1609-1614.
[16] Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, Cheripelli B, Cho TH, Fazekas F, Fiehler J, Ford I, Galinovic I, Gellissen S, Golsari A, Gregori J, Günther M, Guibernau J, H?usler KG, Hennerici M, Kemmling A, Marstrand J, Modrau B, Neeb L, Perez de la Ossa N, Puig J, Ringleb P, Roy P, Scheel E, Schonewille W, Serena J, Sunaert S, Villringer K, Wouters A, Thijs V, Ebinger M, Endres M, Fiebach JB, Lemmens R, Muir KW, Nighoghossian N, Pedraza S, Gerloff C;WAKE-UP Investigators. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med, 2018, 379(7):611-622.
[17] 王冬梅, 郝鹏, 王梦瑶, 林镇洲, 周亮, 范祖森, 潘越, 张晓梅, 潘速跃, 姬仲. 基于动脉自旋标记与弥散加权成像的ASPECTS评分不匹配可以指导醒后卒中患者的机械取栓治疗. 南方医科大学学报, 2020, 40(1):1-5.
(收稿日期:2021-03-22)
(本文编辑:林燕薇)

