Adverse associations of sedentary behavior with cancer incidence and all-cause mortality:A prospective cohort study
Yun Lin,Qion Liu,Fnho Liu,Kyon Hun,Jinxin Li,Xuli Yn,Xinyn Wn,Jihun Chn,Xioqin Liu,Ji Co,Chon Shn,Lin Yu,Fnhon Lu,Xinpin Wu,Linhn Zho,Yin Li,Donshn Hu,Xinn Lu,Jinn Hun,Donn Gu,j,*
a Key Laboratory of Cardiovascular Epidemiology,Chinese Academy of Medical Sciences,Beijing 100037,China
b Department of Epidemiology,Fuwai Hospital,National Center for Cardiovascular Diseases,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100037,China
c Division of Epidemiology,Guangdong Provincial People’s Hospital and Cardiovascular Institute,Guangzhou 510080,China
d Department of Epidemiology and Biostatistics,School of Public Health,Nanjing Medical University,Nanjing 211166,China
e Department of Cardiology,Fujian Provincial Hospital,Fuzhou 350014,China
f Cardio-Cerebrovascular Control and Research Center,Institute of Basic Medicine,Shandong Academy of Medical Sciences,Jinan 250062,China
g Sichuan Center for Disease Control and Prevention,Chengdu 610041,China
h Department of Epidemiology and Health Statistics,College of Public Health,Zhengzhou University,Zhengzhou 450001,China
i Department of Biostatistics and Epidemiology,School of Public Health,Shenzhen University Health Science Center,Shenzhen 518071,China
j School of Medicine,Southern University of Science and Technology,Shenzhen 518055,China
Abstract Background:Inconsistent results have been reported in developed countries for relationships between sedentary behavior and cancer incidence and mortality,and evidence from the Chinese population is scarce.This study aimed to investigate such relationships in large Chinese population-based prospective cohorts and to explore the joint effect and interaction of sedentary behavior and moderate-to-vigorous physical activity(MVPA)on these relationships.Methods: We included 95,319 Chinese adults without cancer from 3 large cohorts and assessed their sedentary behavior and physical activity with a unified questionnaire.Cancer incidence and mortality were confirmed by interviewing participants or their proxies and checking hospital records and death certificates.Hazard ratios (HRs) and 95% confidence intervals (95%CIs) for cancer and mortality were estimated using Cox proportional hazards regression models.Results:During 559,002 person-years of follow-up,2388 cancer events,1571 cancer deaths,and 4562 all-cause deaths were recorded.Sedentary behavior was associated with increased risk of developing cancer and deaths in a dose-response manner.The multivariable-adjusted HRs (95%CIs) were the following:HR=1.16,95%CI:1.01-1.33;HR=1.24,95%CI:1.04-1.48;and HR=1.15,95%CI:1.04-1.28 for cancer incidence,cancer mortality,and all-cause mortality,respectively,for those having ≥10 h/day of sedentary time compared with those having<6 h/day of sedentary time.Sedentary populations(≥10 h/day)developed cancer or died 4.09 years and 2.79 years earlier,respectively,at the index age of 50 years.Failure to achieve the recommended level of MVPA may further aggravate the adverse associations,with the highest cancer and mortality risks being observed among participants with both ≥10 h/day of sedentary time and<150 min/week of MVPA.Limitations of this study include the fact that physical activity information was obtained via questionnaire instead of objective measurement and that there were insufficient incident cases for the analysis of associations between sedentary behavior and site-specific cancers.Conclusion: Sedentary behavior was associated with an increased risk of cancer and all-cause mortality among Chinese adults, especially for those with ≥10 h/day of sedentary time.It is necessary to reduce sedentary time, in addition to increasing MVPA levels, for the prevention of cancer and premature death.
Keywords: All-cause mortality;Cancer;Chinese population;Cohort study;Sedentary behavior
1.Introduction
Cancer is the second leading cause of morbidity and mortality worldwide.There were 18.1 million incident cases and 9.6 million deaths due to cancer globally in 2018,and the number of cancer incidents was expected to reach 29.5 million in 2040.1It was reported that 4.3 million cancer cases and 2.9 million cancer deaths occurred in China in 2018.2Physical activity has been shown to have beneficial effects on cancer incidence and mortality.3However, nearly one-third of adults are physically inactive globally, and people in developing countries, including China, are becoming more sedentary due to shifts in lifestyle.4
Sedentary behavior is defined as any waking behavior including sitting,reclining or lying postures,with a low energy expenditure of 1.5 metabolic equivalents(METs)or less.5The 2018 Physical Activity Guidelines Advisory Committee(2018 PAGAC)of the United States concluded that there was moderate and limited evidence to suggest an increased risk for cancer and mortality in relation to sedentary behavior,6and other research on whether this relationship was affected by physical activity level has yielded conflicting conclusions.7-9Although several systematic reviews have analyzed the relationship between sedentary behavior and cancer and mortality, the results have been inconsistent and have depended on the type of cancer.10-13Thus,the recently published American Cancer Society Guideline for Diet and Physical Activity for Cancer Prevention indicates that more research is needed to address the effect of sedentary behavior on cancer.14Additionally,most of these studies have been conducted in high-income countries,and the findings are of uncertain applicability to the Chinese population.7,15-18Thus far,no study has investigated the effect of sedentary behavior on cancer incidence and mortality in China.
Therefore, our study aimed to investigate the associations of sedentary behavior with cancer incidence and mortality, as well as all-cause mortality, based on large prospective cohorts of 95,319 Chinese adults and to further evaluate the modification effects of physical activity levels on the associations.
2.Methods
2.1.Study population
Participants in this study were from 3 cohorts from the Prediction for Atherosclerotic Cardiovascular Disease Risk in China (China-PAR) project, which included the China Multi-Center Collaborative Study of Cardiovascular Epidemiology—1998 (China MUCA 1998), International Collaborative Study of Cardiovascular Disease in Asia(InterASIA),and Community Intervention of Metabolic Syndrome in China and Chinese Family Health Study (CIMIC).Detailed information of these cohorts has been described in the previous study.19Briefly,China MUCA 1998,InterASIA,and CIMIC were initiated in 1998,2000-2001,and 2007-2008,respectively.China MUCA 1998 and InterASIA were followed up twice during 2007-2008 and 2012-2015, while CIMIC was followed up once during 2012-2015.Our study was approved by the Institutional Review Board at Fuwai Hospital in Beijing and by other participating institutions.Written informed consent was signed by each participant before data collection.
Information about sedentary behavior was collected from the 2007-2008 follow-up using a unified questionnaire for the 3 cohorts;hence, the 2007-2008 survey was used as the baseline in this study.Participants who responded to the 2007-2008 survey(n=104,957)were initially enrolled.We then excluded 1255 individuals from 3 sites in the InterASIA project because these individuals were only followed up until 2008.A total of 7654 individuals were excluded because they were lost to follow-up.Finally,317 individuals were excluded due to missing or incorrect activity information(daily total time<22 h or>26 h per day)and 412 individuals were excluded because they were diagnosed with cancer at baseline.Thus, a total of 95,319 participants were included for the current analysis(Fig.1).
2.2.Data collection
At baseline and follow-up visit, data on physical activity,sedentary behavior, and other covariates were collected by trained staff through the use of a unified questionnaire.A physical examination and blood biochemical examinations were also conducted under strict quality control.
The information on physical activity at baseline was collected by asking individuals, “How many hours did you usually spend on these activities per day on weekdays/weekends in the previous year?” Daily activities were categorized according to the 2011 Compendium of Physical Activities.20This compendium uses the following categories for the intensity of physical activity:vigorous activities(>6.0 METs,e.g.,running or heavy farming work), moderate activities (3.0-5.9 METs,e.g., brisk walking or yard work), light activities (1.5-2.9 METs,e.g.,walking slowly or standing at work),sedentary activities (<1.5 METs, e.g., watching television, reading, or reclining), and sleeping.Moderate-to-vigorous physical activity (MVPA) was calculated by summing the time spent on moderate physical activity and on vigorous physical activity weighted by 2.MVPA was further categorized by the level recommended by the Physical Activity Guidelines for Americans(150 min/week).21
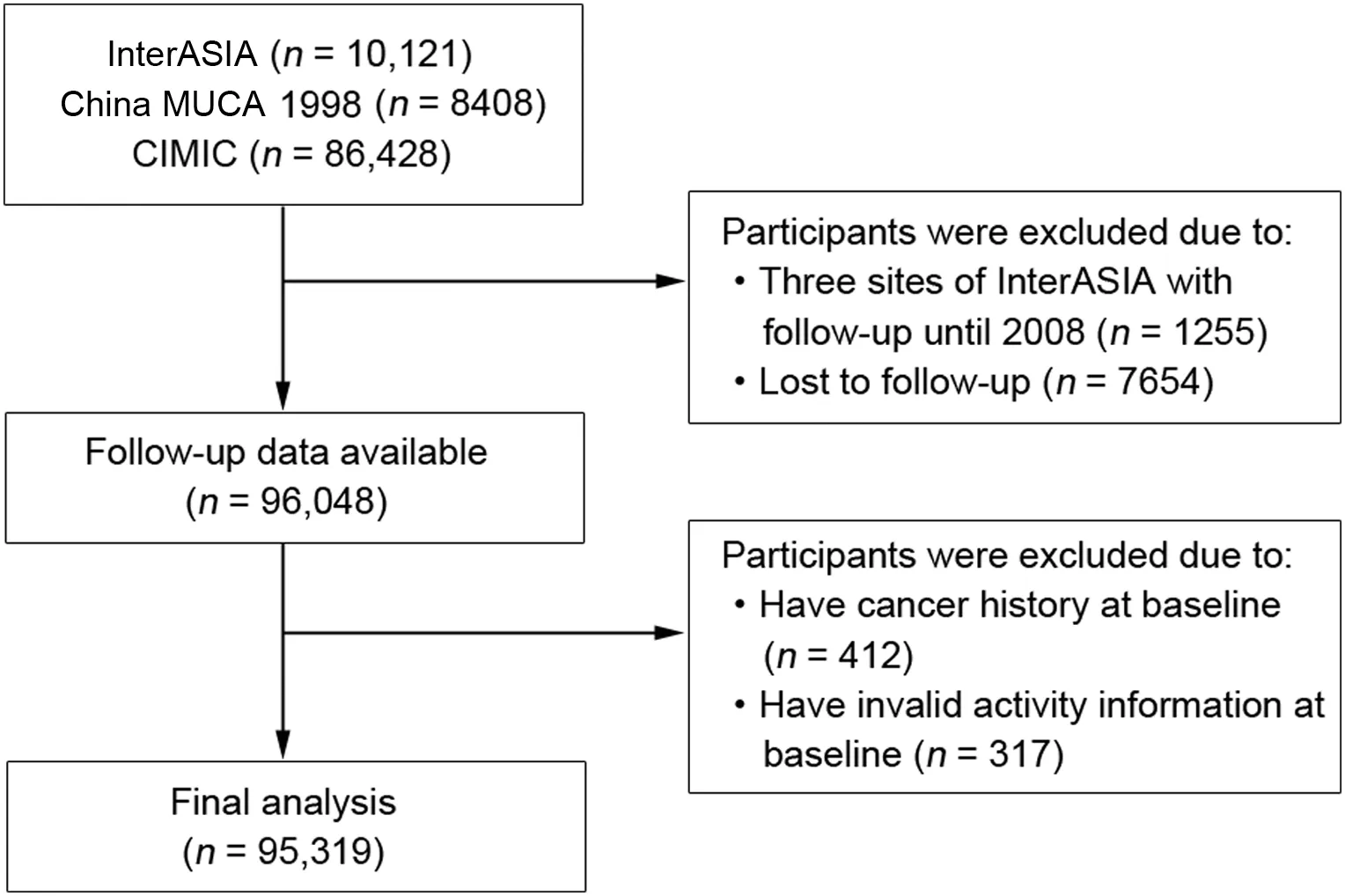
Fig.1.Flow chart of study participants included and excluded in the study.China MUCA 1998=China Multi-Center Collaborative Study of Cardiovascular Epidemiology—1998; CIMIC=Community Intervention of Metabolic Syndrome in China and Chinese Family Health Study; InterASIA=International Collaborative Study of Cardiovascular Disease in Asia.
Other information was collected on sociodemographic covariates (age, gender, address, urban or rural resident, and educational attainment) and lifestyle behaviors (smoking status and alcohol consumption).Information on disease history and medication use were collected by using standardized questionnaires.Area of residence was classified into either urban or rural.A detailed address of residency was collected for determining geographical region.Educational attainment was measured by asking participants what level of education they had attained (uneducated, primary school, middle school, high school, college or university, post-graduate study, or above).Current smoking status was evaluated by asking participants whether they had smoked more than 100 cigarettes thus far,and those who answered “Yes” were then asked whether they were currently smoking.Participants who answered “Yes” to both questions were categorized as current smokers; if they answered“Yes”or no to only the first question,they were categorized as non-current smokers.Alcohol drinking was defined as alcohol consumption at least 12 times in the last year.Body weight and height were measured with participants wearing light clothes without shoes, and body mass index (BMI) was defined as body weight in kilograms divided by height in meters squared.
Outcome ascertainment was conducted in 3 steps.First,study participants or their proxies were interviewed regarding whether participants had developed diseases or had died since the last survey.Those who failed to respond were lost to follow-up.Second,medical records or death certificates were collected if participants had been diagnosed with cancer or had died.Third, medical records or death certificates were further ascertained by a study-wide end-point assessment committee established by the Chinese Academy of Medical Sciences.The diagnosis of cancer was coded according to the codes used in the International Classification of Diseases,Tenth Revision(ICD-10),and overall cancer was coded as C00-97 in our study.
2.3.Statistical analysis
In our study, participants were classified into 4 categories by daily sedentary time according to dose-response association and quartiles: <6 h/day,6-<8 h/day,8-<10 h/day,and≥10 h/day.The least sedentary category (<6 h/day)served as the reference.Baseline characteristics of included participants are presented as mean ± SD for continuous variables and as percentages for categorical variables.
For analyses of cancer incidence, person-years were calculated from the date of baseline to the date of cancer incidence,death,or last follow-up,whichever occurred earlier.For analyses of cancer mortality and all-cause mortality, person-years were calculated from the date of baseline to the date of death or last follow-up,whichever occurred earlier.Cox proportional hazards regression models stratified by cohort were used to estimate hazard ratios (HRs) and 95% confidence intervals(95%CIs)for cancer incidence,cancer mortality,and all-cause mortality associated with sedentary behavior.The analysis was performed with 3 models.Model 1 was adjusted for gender and age at baseline;Model 2 was further adjusted for geographic region (northern or southern China), education level(below high school, high school, or above), urbanization(urban or rural), alcohol consumption (yes or no), current smoking status(yes or no),and BMI;and Model 3 was further adjusted for daily MVPA level.Model 3 was used as the main model in this study.Test of trend was conducted by modeling the median of sedentary time in each category as a continuous variable.
Restricted cubic splines with 4 knots at the 5th, 35th,65th, and 95th percentiles were fitted with the Cox proportional hazards model to explore the dose-response relationship between sedentary time and outcomes, with reference set at 6 h/day.In addition, loss of life expectancy and loss of cancer-free years related to excess sedentary time were estimated as the differences of the areas under the survival curves based on Cox proportional models, with age as the timescale.The joint associations of sedentary behavior and MVPA with risks of cancer incidence and mortality were evaluated.Participants were cross-categorized into 8 groups according to sedentary time (<6 h/day,6-<8 h/day, 8-<10 h/day, and ≥10 h/day) and MVPA(<150 min/week and ≥150 min/week), and the most active category (with sedentary time <6 h/day and MVPA ≥150 min/week) served as the reference.
Subgroup analysis by specific baseline characteristics (age,gender, smoking, and alcohol consumption) was conducted,and the interaction terms with sedentary time were tested to investigate potential effect modifications.To evaluate the robustness of the results, sensitivity analyses were conducted by excluding participants who developed cancer or died within the first year of follow-up and those who had cardiovascular diseases or end-stage renal disease at baseline.In addition,sensitivity excluding BMI as a covariate was conducted since BMI might be a potential causal pathway factor of sedentary behavior and cancer and mortality.Furthermore, to adjust for the influence of the occurrence of non-cancer deaths on cancer events, we conducted a competing risk analysis by using Fine and Gray’s approach.22
All analyses were performed with SAS Version 9.4(SAS Institute Inc., Cary, NC, USA).All statistical tests were two-sided, with apvalue <0.05 considered statistically significant.
3.Results
3.1.Baseline characteristics
Among the 95,319 participants enrolled in our study, the mean age was 53.1 ± 12.3 year old at baseline, and 39.6%were male.The mean sedentary time was 7.9±3.4 h/day.Participants with longer sedentary time were more likely to live in northern China and in urban areas,to have a higher education level,and to have a higher BMI.Subjects with more sedentary time tended to spend less time on MVPA (Table 1).Thebaseline characteristics of each included cohort are shown in Supplementary Table 1.
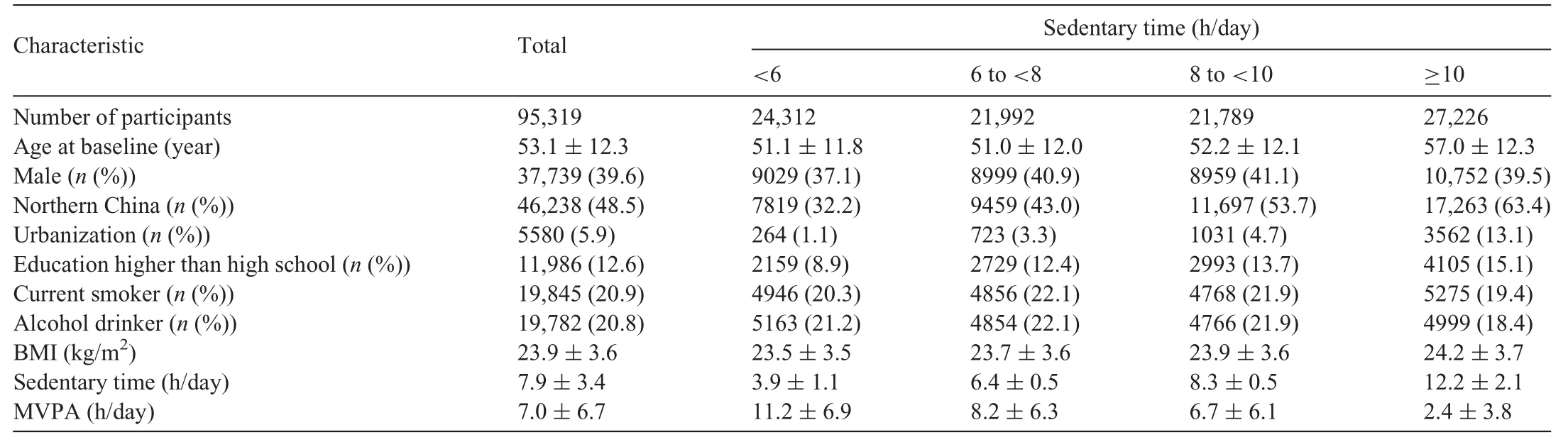
Table 1Baseline characteristics of participants according to categories of daily sedentary time.
3.2.Association of sedentary behavior with cancer incidence and mortality
During 559,002 person-years of follow-up (median of 5.8 years), 2388 cancer events, 1571 cancer deaths, and 4562 all-cause deaths were recorded.The most observed types of cancer were lung cancer (n=391); gastric cancer (n=333); liver cancer(n=244); colon, rectum, and anus cancer (n=151); esophagus cancer (n=138); and breast cancer (n=135).The incidence or mortality rates for cancer,cancer deaths,and all-cause deaths were 431.7, 283.0, and 821.8 per 100,000 person-years, respectively.The associations of sedentary behavior with cancer and mortality are presented in Table 2.Generally, higher levels of sedentarybehavior were associated with increased risk of cancer incidence,cancer mortality, and all-cause mortality.Compared with those having <6 h/day sedentary time, the multivariable-adjusted HRs and 95%CIs of cancer incidence were HR=0.97, 95%CI: 0.85-1.11; HR=1.11, 95%CI: 0.98-1.27; and HR=1.16, 95%CI:1.01-1.33 for those with 6-<8 h/day, 8-<10 h/day, and≥10 h/day sedentary time, respectively (pfor trend: 0.013).The corresponding HRs and 95%CIs were HR=0.99, 95%CI: 0.83-1.17; HR=1.20, 95%CI: 1.02-1.42; and HR=1.24, 95%CI:1.04-1.48, respectively, for cancer mortality (pfor trend: 0.006)and HR=0.90,95%CI:0.81-1.00;HR=0.97,95%CI:0.88-1.08;and HR=1.15, 95%CI: 1.04-1.28, respectively, for all-cause mortality(pfor trend:<0.001)(Table 2).
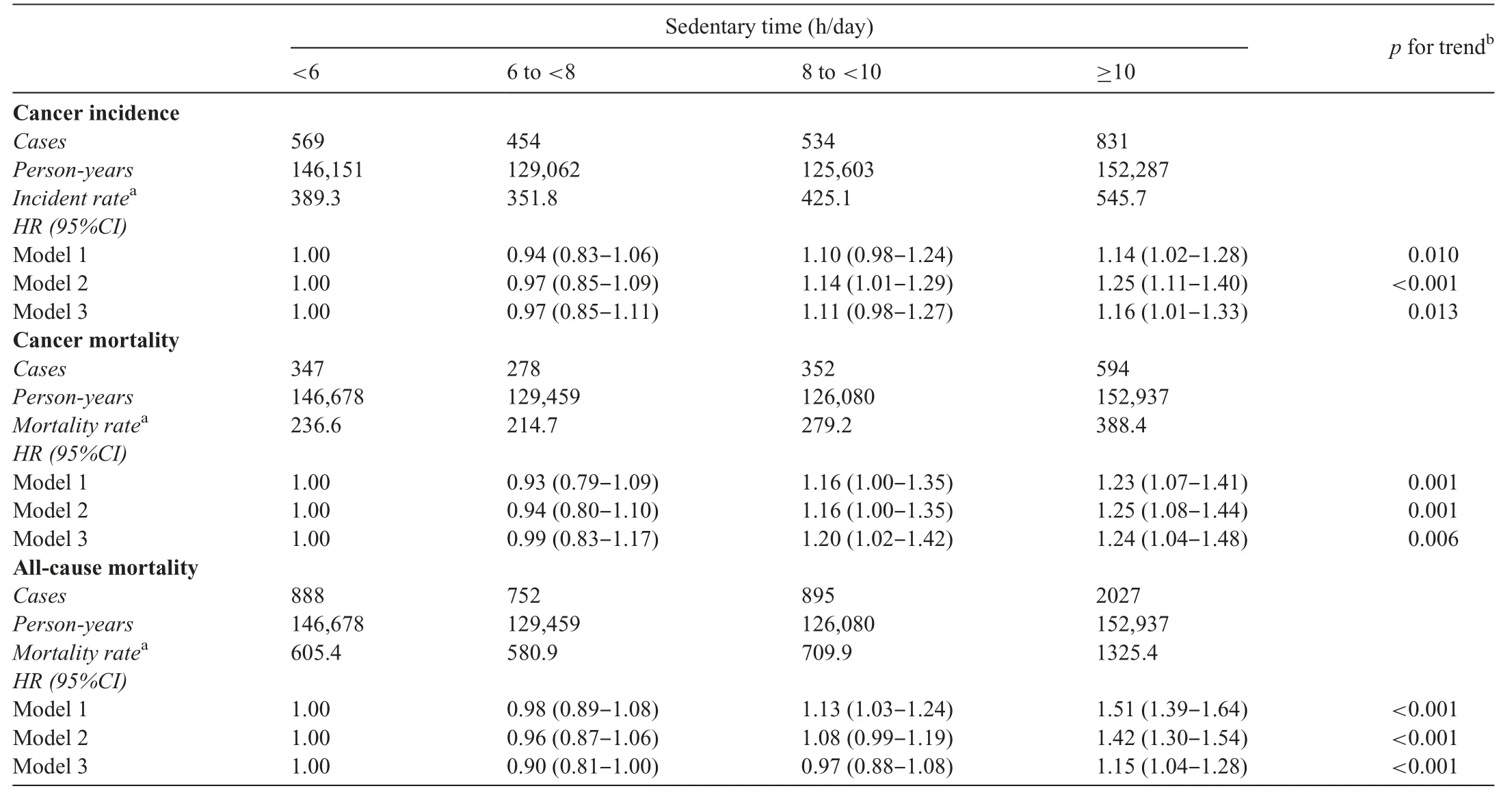
Table 2Hazard ratios of cancer incidence and mortality associated with categories of daily sedentary time.
The results of the dose-response analyses were in conformity with the categorical analyses.Restricted cubic splines indicated nonlinear dose-response relationships between daily sedentary time and risk of cancer incidence, cancer mortality,and all-cause mortality (pfor nonlinear association: 0.002,0.015, and <0.001, respectively; Fig.2).The dose-response relationships showed a J-shape,with the lowest risks observed at approximately 6 h/day.
Participants with ≥10 h/day of sedentary time were estimated to have fewer cancer-free years and shorter life expectancy compared with those with<6 h/day.As shown in Fig.3,those in the sedentary population (≥10 h/day) developed cancer or died 4.09 years or 2.79 years earlier,respectively,at the index age of 50 years.
3.3.Joint associations of sedentary behavior and MVPA with cancer and mortality
The HRs and 95%CIs for joint associations of sedentary behavior and MVPA with cancer incidence and cancer mortality are shown in Fig.4.Notably, compared with those spending <6 h/day of sedentary time and not meeting MVPA recommendation, those with ≥10 h/day of sedentary time had a higher risk of all-cause mortality whether they reached the MVPA recommendation or not, with HRs (95%CIs) of 1.21(1.08-1.35) and 1.72(1.56-1.90), respectively.In addition,although insignificant interactions between sedentary time and MVPA were observed, participants with both ≥10 h/day of sedentary time and <150 min/week of MVPA had significantly more risk (45% and 38%, respectively) of developing cancer incidence and cancer mortality in comparison to those who reported the least sedentary time and achieved the MVPA recommendation of 150 min/week(Fig.4)
3.4.Subgroup and sensitivity analyses
In the subgroup analyses, associations between categories of sedentary time with cancer incidence, cancer morality, and all-cause morality were consistent across age,gender,and smoking status(Table 3).However,the risk of cancer mortality associated with sedentary behavior showed different trends among alcohol drinkers and non-drinkers (pfor interaction=0.009;Table 3).The sensitivity analyses did not considerably alter the significant associations of sedentary time with cancer incidence,cancer mortality, and all-cause mortality (Table 4).For cancer incidence, after exclusion of subjects who developed cancer within the first year of follow-up, the trends across sedentary categories remained significant.Moreover, after excluding BMI as a covariate, the results were robust, although the magnitude of effect estimates were slightly decreased.
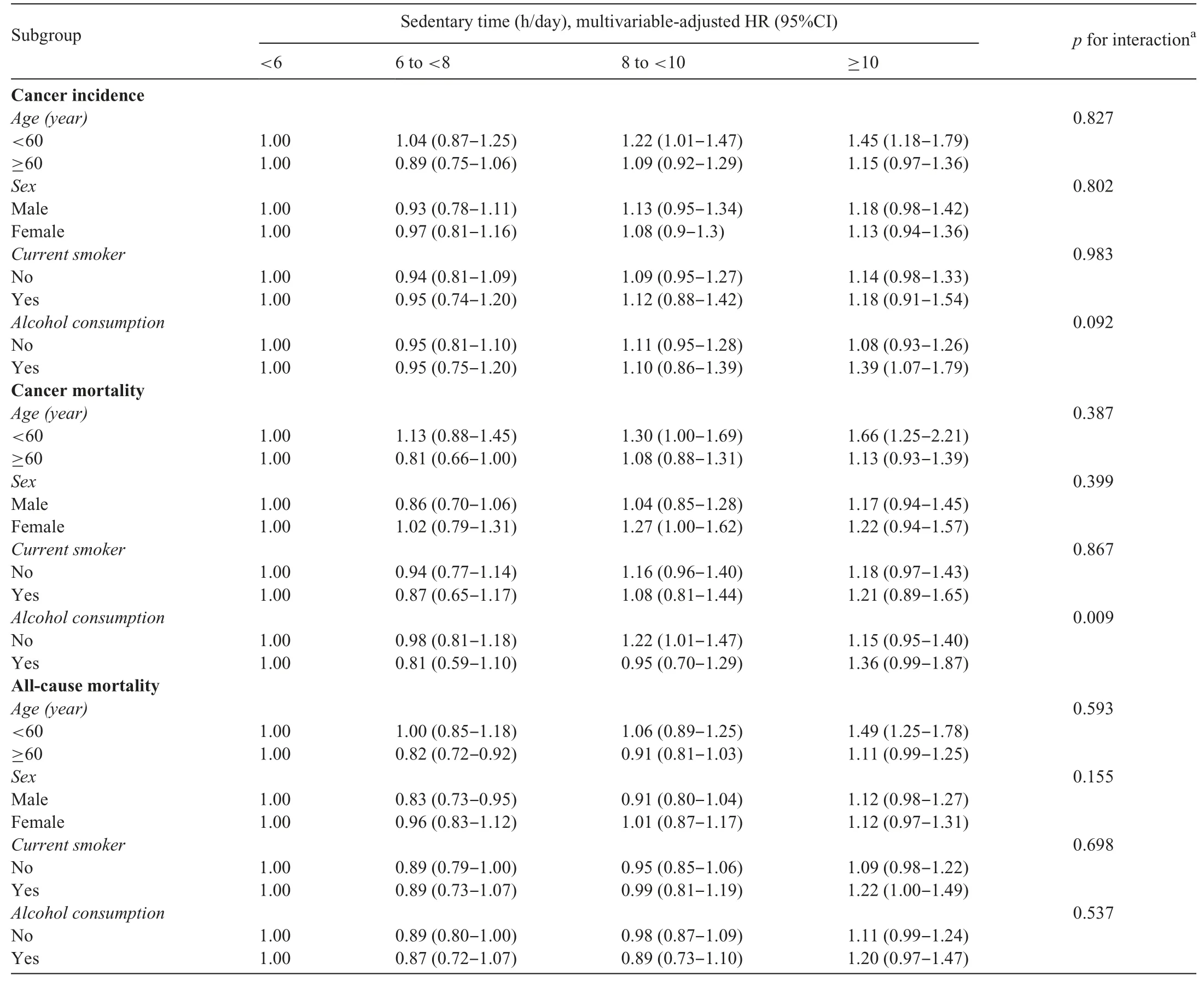
Table 3Subgroup analyses for cancer incidence and mortality associated with sedentary time according to baseline characteristics.
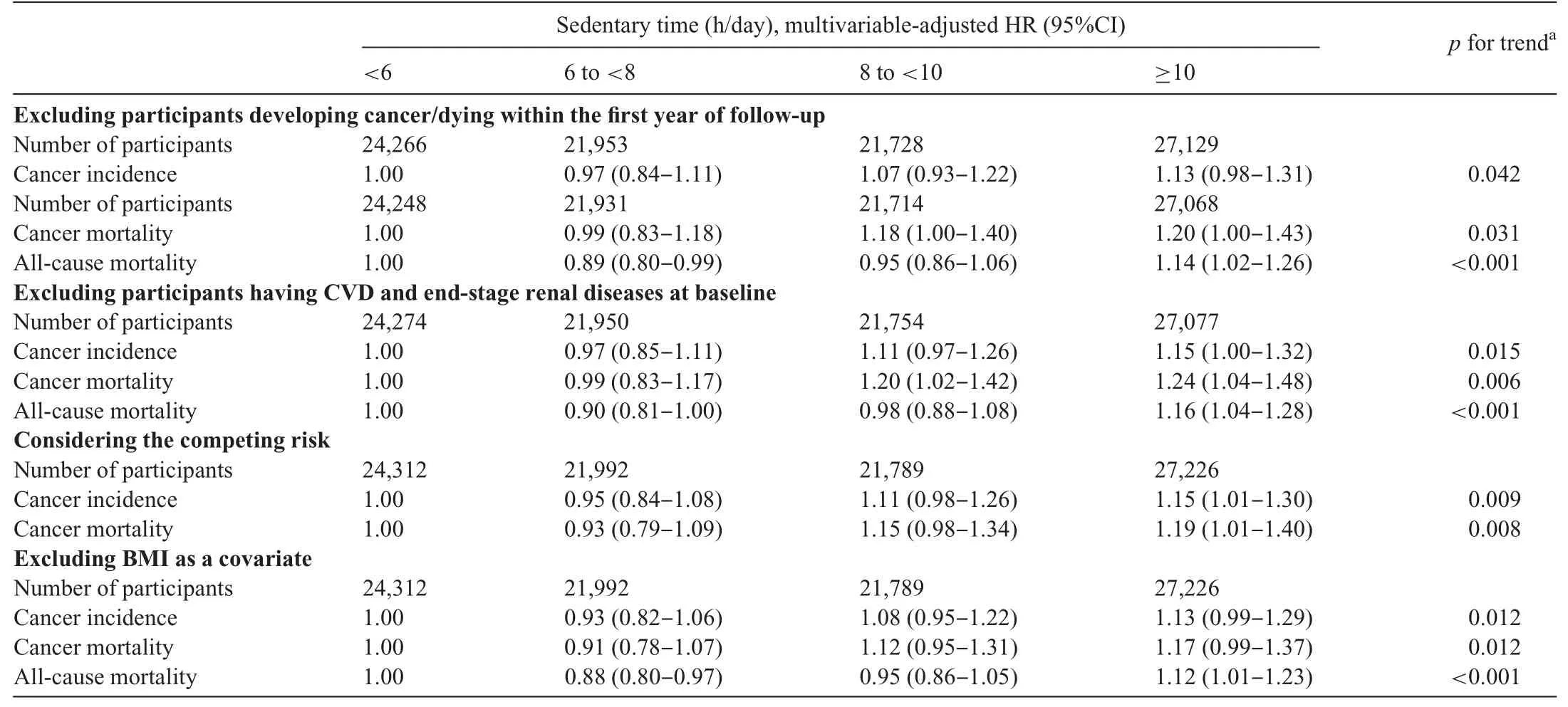
Table 4Sensitivity analysis for cancer incidence and mortality associated with categories of sedentary time.
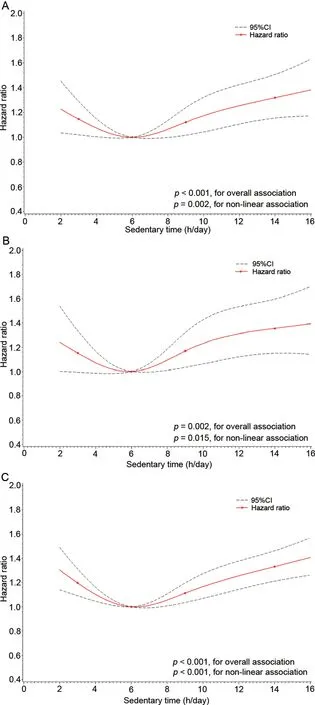
Fig.2.Dose-response associations between daily sedentary time and cancer and mortality.(A) cancer incidence, (B) cancer mortality, and (C) all-cause mortality.Data were fitted by restricted cubic spline Cox proportional hazards models, with 4 knots placed at the 5th (3 h/day), 35th (6 h/day), 65th (9 h/day), and 95th (14 h/day) percentiles of daily sedentary time as a continuous variable.Models were adjusted for cohort, gender, age, geographic region(northern/southern China), urbanization, education, current smoking status and alcohol consumption, body mass index, and daily time of moderate-tovigorous physical activity.95%CI=95%confidence interval.
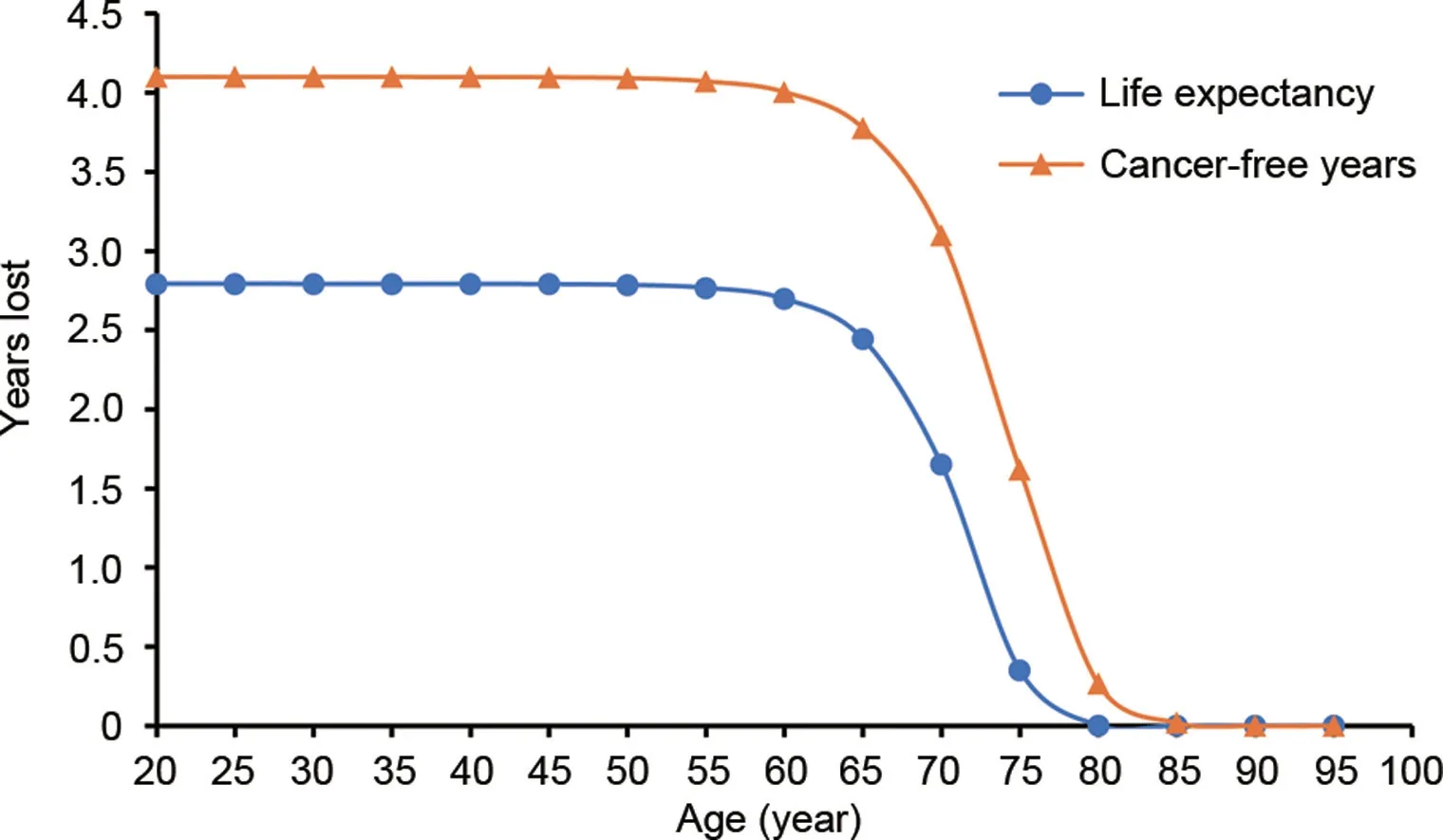
Fig.3.Years of life lost and cancer-free years lost in a sedentary population.Years of life lost and cancer-free years lost were evaluated in participants with≥10 h/day of sedentary time compared with those with <6 h/day at different ages.Years of life lost was estimated by the difference in the area under the survival curves based on Cox proportional models,with age as the time scale.
4.Discussion
Using large-population-based prospective cohorts, we observed a nonlinear dose-response associations between sedentary behavior and cancer incidence, cancer mortality, and all-cause mortality for the first time among a general Chinese adult population.The detrimental effect of sedentary behavior was strongest among participants with ≥10 h/day of sedentary behavior and <150 min/week of MVPA.Our study provides the first evidence that lower sedentary time combined with a higher MVPA level prevents cancer and premature death.
Evidence from cohort studies and meta-analyses comprising studies of populations from high-income countries have reported inconsistent risks of cancer incidence, cancer mortality,and all-cause mortality in sedentary populations.11-13,15,18Several meta-analyses and systematic reviews have shown nonlinear dose-response relationships between total sedentary time and cancer mortality, and all-cause mortality, but none of the included studies in our review was conducted in China.23-25Our results indicated J-shaped nonlinear dose-response relationships between daily sedentary time and cancer incidence,cancer mortality, and all-cause mortality in a general Chinese population.The lowest risk was seen at 6 h/day of sedentary time,and those with ≥10 h/day of sedentary time had significantly increased risks.Previous studies have indicated that the threshold of sedentary time is between 6 and 7 h/day, with the risks of cancer and mortality increasing more rapidly with sedentary time above this amount.24,25In addition, it has been reported that the average sedentary time was 8.6 h/day in 10 environmentally and culturally diverse countries and regions.23The mean sedentary time of participants in our cohorts was 7.9 h/day,which is slightly lower than 8.6 h/day but is still beyond the threshold of 6-7 h/day.Therefore, new strategies and actions are needed in order to alleviate the sedentary lifestyle in China,thus preventing cancer and extending longevity.
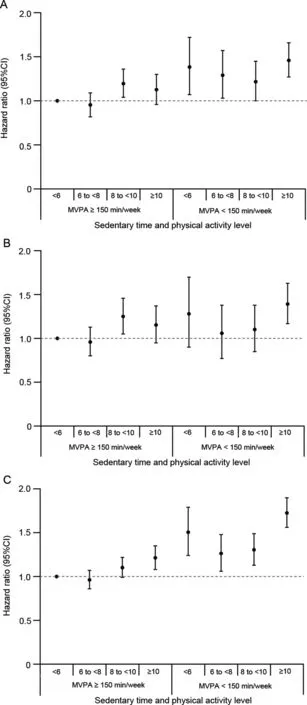
Fig.4.Hazard ratios for cancer and mortality (A)cancer incidence,(B)cancer mortality,and(C)all-cause mortality for joint associations between sedentariness and MVPA.The model was stratified by cohort and adjusted for gender, age, geographic region (northern/southern China), urbanization,education, current smoking status and alcohol consumption, and body mass index.The p values for interaction are 0.142, 0.187, and 0.139 for cancer incidence, cancer mortality, and all-cause mortality, respectively.The unit of ranges for<6,6 to<8,8 to<10,and ≥10 is h/day.95%CI=95% confidence interval;MVPA=moderate-to-vigorous physical activity.
Populations with more sedentary time tend to spend less time on physical activity,and the effects of sedentary behavior on health outcomes need to be adjusted for physical activity.25Some recent studies focusing on sedentary behavior and healthoutcomes have taken the effect of MVPA into consideration.25,26In our study, the HRs for cancer incidence, cancer mortality, and all-cause mortality were mildly attenuated, but remained significant, after adjusting for daily MVPA time,thus suggesting that prolonged sedentary time might independently increase the risk of cancer and mortality.We further investigated the joint associations of sedentary behavior and MVPA with cancer incidence, cancer mortality, and all-cause mortality.Significant adverse effects of sedentary time on cancer incidence, cancer mortality, and all-cause mortality were observed regardless of the MVPA level, which is consistent with findings in previous studies.7,9,11,15The effects in our study were generally most pronounced among those with sedentary times of ≥10 h/day and MVPA times of <150 min/week.In addition, participation in a substantial amount of MVPA failed to counteract the increased risk of mortality caused by a high amount of sedentary time.Our findings call into question whether MVPA alone is sufficient to mitigate a high mortality risk in adults who spend large amounts of time engaging in sedentary behavior.Thus, populations unable to participate in large amounts of MVPA due to physical barriers and time constraints might achieve cancer prevention by reducing their sedentary time.
Evidence from the 2018 PAGAC is insufficient for determining whether the associations between sedentary behavior and cancer and mortality are modified by factors such as sexand age.20Our study demonstrated a consistent association between sedentary behavior and cancer and mortality among adults with different sex,age,and smoking status.In addition,several sensitivity analyses showed that associations between sedentary behavior and cancer incidence, cancer mortality,and all-cause mortality were robust.When we excluded the participants who developed cancer within the first year of follow-up,the trends remained significant.
Given that the detrimental effect of sedentary behavior is likely to be independent of decreased physical activity,previous studies have investigated the mechanisms underlying prolonged sedentary time and increased risks of cancer incidence, cancer mortality, and all-cause mortality.These studies found that sedentary behavior might affect metabolic dysfunction, chronic inflammation, sex hormone levels, and vitamin D levels directly or indirectly through adiposity,which increases risk of cancer.27Additionally, spending time sitting might be associated with other unhealthy behaviors, such as increased energy intake, which are also related to cancer development.28Despite the identification of these possible mechanisms, future studies are still warranted in order to reveal other pathophysiological mechanisms of the harmful effects of sedentary behavior on cancer development.
Our study has several strengths, including its large sample size, strict quality control, reliable information, and data collection, and adjustment for a series of important covariates at the individual level.However, several limitations should also be noted.First,information on physical activity and sedentary behavior was obtained via questionnaire rather than via objective measurement.Although our interviewers were trained to ensure a precise inquiry,measurement errors may nonetheless have attenuated the associations observed, and future studies using objective measures are warranted.Second, instead of collecting information on different types of sedentary behaviors,we only obtained information on the total daily time spent watching TV, eating, reading, and reclining during the workday and on days off, which made it impossible to analyze the health effects of different types of sedentary behavior.Health effects of occupational and leisure-time sedentary behavior have been reported in some previous studies,13,29-32and screen time has been shown to be more likely to increase the risk of cancer and mortality.In future follow-up surveys,information on the types of sedentary behavior should be collected.Third,because of an insufficient number of cases of site-specific cancers in our study sample, we were unable to provide solid evidence for associations between sedentary behavior and sitespecific cancers.In a previous meta-analysis comprising 43 observational studies, positive associations were observed between total sedentary time and risks of colon cancer,endometrial cancer, and lung cancer.13In our future follow-up work with our cohorts, we will attempt to obtain more data on the effect of sedentary behavior on the incidence and mortality related to site-specific cancers, especially those types that are highly prevalent in China.Finally, although we adjusted for confounders, including sociodemographic factors, lifestyle behaviors, and weight status, residual confounding from other factors,such as dietary habits,still possibly exist.33,34For example,the US National Health and Nutrition Examination Survey reported that the lowest risk of cancer mortality and all-cause mortality was observed among cancer survivors who had low levels of sedentary behaviors and healthy diets.35Additional investigations that consider other potential confounders should be conducted.
5.Conclusion
Our study found independent dose-response associations of sedentary behavior with cancer incidence,cancer mortality,and all-cause mortality among a general population of Chinese adults.Excessive sedentary time increases the risk of early onset of cancer and shorter life expectancy.In addition to promoting physical activity, public health programs and policies should advocate for a reduction in sedentary time in order to prevent cancer and premature mortality.
Acknowledgments
The authors thank the staff and participants of the Prediction for Atherosclerotic Cardiovascular Disease Risk in China project for their important participation and contribution.This study was supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences(2019-I2M-2-003 and 2017-I2M-1-004), National Key R&D Program of China (2017YFC0211700 and 2018YFE0115300), and the National Natural Science Foundation of China (91643208).
Authors’contributions
YL performed the statistical analysis, interpreted the data,and drafted the initial manuscript;QL performed the statistical analysis and interpreted the data; FL, KH, JL, XY, and XW interpreted the data and critically reviewed the manuscript;JCC, XL, JC, CS, LY, FL, XPW, LZ, YL, DH, XL, JH performed data acquisition, and critically reviewed the manuscript; DG conceived and designed the study, performed data acquisition,and critically reviewed the manuscript.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.04.002.
 Journal of Sport and Health Science2021年5期
Journal of Sport and Health Science2021年5期
- Journal of Sport and Health Science的其它文章
- Association between physical activity and cardiovascular risk factors:Dose and sex matter
- Dynamic resistance exercise increases skeletal muscle-derived FSTL1 inducing cardiac angiogenesis via DIP2A-Smad2/3 in rats following myocardial infarction
- Relationship of proprioception,cutaneous sensitivity,and muscle strength with the balance control among older adults
- Associations of accelerometer-determined physical activity and sedentary behavior with sarcopenia and incident falls over 12 months in community-dwelling Swedish older adults
- Physical activity and its relationship with COVID-19 cases and deaths:Analysis of U.S.counties
- Exercise attenuates bone mineral density loss during diet-induced weight loss in adults with overweight and obesity:A systematic review and meta-analysis
