Saddle pulmonary embolism is not a sign of high-risk deterioration in non-high-risk patients: A propensity score-matched study
Dong Jia, Chao Ji, Min Zhao
1 Department of Emergency Medicine, Shengjing Hospital of China Medical University, Shenyang 110004, China
2 Department of Clinical Epidemiology, Shengjing Hospital of China Medical University, Shenyang 110004, China
KEYWORDS: Main pulmonary artery; Pulmonary embolism; Computerized tomography pulmonary arteriography
INTRODUCTION
Acute pulmonary embolism (PE) is an emergent cardiopulmonary disease caused by thrombotic blockage of the pulmonary artery. Reported mortality rates are as high as 25%.[1]Evaluating the prognosis of acute PE has shifted from examining mortality to deterioration in the short term,[2]particularly in non-risk acute PE patients.[3,4]This deterioration can be assessed by the occurrence of adverse events.[5]
Bova score and risk stratification are two widely used methods to predict the risk of deterioration.[2,6]In addition, identification of the thrombus location using computerized tomography pulmonary arteriography (CTPA) can also help to evaluate the risk of deterioration.[7-9]Saddle main pulmonary artery (MPA) embolism, defined as thrombus straddling the bifurcation of the MPA trunk,[10]is a special subtype of thrombus location. In general, the presentation of saddle MPA embolism is a sign of poor short-term prognosis.[10,11]However, some studies have reported no correlation between saddle MPA embolism and deterioration.[5,12,13]The low incidence (2.6%-9.0%) of saddle MPA embolisms,[5,12]and the inconsistent baseline and imbalance of PE severity between saddle and nonsaddle MPA embolism contribute to this controversy.[13]
Propensity score matching (PSM) analysis is suitable for studies with low rates of occurrence,[14]such as the incidence of saddle MPA embolism in acute PE. It reduces selection bias, as it balances the differences in clinical features and increases the statistical strength of retrospective studies.[15,16]To accurately assess the efficacy of saddle MPA embolism for predicting deterioration, we adjusted the baseline characteristics, balanced the acute PE severity with Bova score,[6]and performed risk stratifi cation, which included the simple PE severity index (s-PESI)[2]by PSM. After PSM, we analyzed whether saddle MPA embolism represented a high risk for deterioration in non-high-risk acute PE patients.
METHODS
Study design and setting
We conducted this retrospective study on non-high-risk acute PE patients between January 2011 and October 2019.
Study criteria
Totally 858 non-high-risk acute PE patients who presented to the Shengjing Hospital of China Medical University were reviewed retrospectively. Non-high-risk acute PE patients were defi ned as patients who were admitted to the hospital: (1) without a history of cardiopulmonary resuscitation; (2) with systolic blood pressure ≥90 mmHg (1 mmHg=0.133 kPa); (3) no need for vasopressors; (4 ) without end-organ hypotension as defined by systolic pressure drop of <40 mmHg lasting for ≤15 minutes.[2]The inclusion criteria were: a diagnosis of acute PE by CTPA and ag ed ≥18 years. The exclusion criteria were: (1) definitive diagnosis of cor pulmonale and heart failure; (2) chronic and recurring PE; (3) presence of pulmonary artery tumor; (4) current pregnancy; (5) absence of CTPA data or echocardiography; (6) absence of cardiac troponin I (cTn-I) and N-terminal probrain natriuretic peptide (NT-proBNP); and (7) receiving thrombolysis before admission to the hospital.
Clinical data
Demographic and baseline characteristics, such as heart rate and systolic pressure, were collected from medical records. Deterioration was defined as the occurrence of adverse events, including PE-related shock, need for mechanical ventilation and cardiopulmonary resuscitation, life-saving hemodynamic support, and thrombolysis, within the first 30 days of admission to the hospital.[5]The date of occurrence of deterioration was also recorded.
Pulmonary embolism severity
Right ventricular dysfunction (RVD) was confi rmed by echocardiography. Risk stratification was evaluated using the s-PESI, cTn-I, NT-proBNP, and RVD.[2]Patients were divided into the intermediate-high-risk, intermediate-low risk, and low-risk groups.[2]The Bova score was evaluated according to systolic pressure, heart rate, cTn-I, and RVD.[6]Patients were then divided according to Bova score (stage I, stage II, and stage III) (supplementary Tables 1, 2, and 3).
CTPA acquisition
A 64 detector-row computerized tomography system (Aquilion KV-120; Toshiba Medical Systems Corporation, Tokyo, Japan; parameters: 380 mA, 120 kV) was used to perform pulmonary angiography with 1-mm thick sections. The iodinated nonionic contrast agent (100 mL) was injected into the antecubital vein using an automatic dual-tube highpressure injector (Ulrich REF XD 2051; Ulrich Medical GmbH, Germany) at a rate of 4 mL/second from the thoracic inlet to the upper abdomen.
MPA reconstruction and thrombus location
The MPA was reconstructed using Mimics Medical software (version 19.0, Mimics Medical software, Belgium) with CTPA data. The MPA was divided into four parts: MPA trunk, MPA bifurcation, left pulmonary artery (LPA), and right pulmonary artery (RPA).[7,8]Based on the thrombus location, the acute PE patients were divided into four types: (1) MPA embolism (thrombus at LPA, RPA, bilateral pulmonary arteries, or bifurcation); (2) saddle MPA embolism (thrombus at bifurcation, or at bifurcation and extending into the LPA and RPA); (3) non-saddle MPA embolism (thrombus at the RPA or LPA and no thrombus at bifurcation); and (4) non-MPA embolism (no thrombus at MPA, but thrombus at peripheral pulmonary artery) (supplementary Figures 1A, B, and C). The correlation among the types of thrombus locations is summarized in supplementary Figure 2.
PSM
To investigate the predictive ability of MPA embolism and saddle MPA embolism for deterioration, baseline characteristics were normalized by age, sex, Bova score, and risk stratification, and four subgroups of PSM individuals were developed: (1) to evaluate whether MPA embolism was a sign for a high risk of deterioration, MPA embolism and non-MPA embolism patients were matched; (2) after excluding the interference of saddle MPA embolism, to evaluate whether non-saddle MPA embolism was still a sign for a high risk of deterioration, non-saddle MPA embolism and non-MPA embolism patients were matched; (3) to evaluate whether saddle MPA embolism was a sign for a high risk of deterioration in MPA embolism patients, saddle MPA embolism and non-saddle MPA embolism patients were matched; (4) to evaluate whether saddle MPA embolism was a sign for a high risk of deterioration compared with non-MPA embolism, saddle MPA embolism and non-MPA embolism patients were matched (Figure 1).
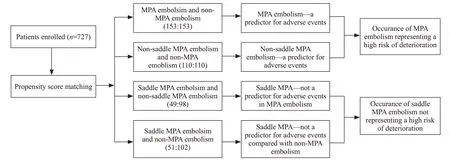
Figure 1. Flowchart of propensity score matching. MPA: main pulmonary artery.
Thrombus splintering
To investigate differences between deterioration and non-deterioration patients with saddle MPA embolisms using CTPA data, the right and left pulmonary regions were divided into ten and eight segments, respectively, from the third stage pulmonary artery. If the thrombus was located at one pulmonary artery or at a relatively downstream pulmonary artery, 1 point was recorded, and 0 point was recorded for other locations. The scores of each pulmonary artery were added up. Thrombus splintering was evaluated by the total number of points in the 18 pulmonary arteries. This method is the Qanadli Scoring technique.[17,18]
Analysis
Quantitative variables with normal distributions were expressed as the mean±standard deviation (SD) and analyzed with Student’st-test. Categorical variables and their differences were analyzed with theχ2test. To decrease the selection bias and potential confounding factors, we estimated the propensity score by means of logistic regression analysis and performed 1:1/1:2 nearest-neighbour individual matching based on the logit of propensity score using calipers of a width equal to 0.1 by age, sex, Bove score, and risk stratifi cation.[14]A Cox model was used to analyze the correlation between the variables and deterioration in univariate and multivariate analyses, and hazard ratios (HRs) were calculated. Variables withP-value <0.10 in the univariate analysis were included in the multivariate analysis.[16]Kaplan-Meier analysis was used to compare the risk of deterioration. Receiver operating characteristic (ROC) curves were used to confirm identification ability. Two-tailedPvalues <0.05 were considered statistically significant. Statistical analyses were performed using R software version 3.3.2 (http://www.R-project.org).
RESULTS
Demographic, baseline characteristics, and pulmonary embolism severity
Of the 727 patients enrolled, 70 presented with deterioration, including 38 males and 32 females. Their average age was 59.91±15.29 years. Of the remaining 657 patients who did not present with deterioration, 328 were males, 329 were females, and their average age was 59.71±15.72 years. In terms of thrombus location, the prevalence of saddle MPA embolisms and MPA embolisms were higher in patients with deterioration than in those with non-deterioration (P<0.001 andP<0.001, respectively). There was a higher proportion of patients with Bova II and Bova III grades in patients with deterioration compared to those without deterioration (P=0.002 andP<0.001, respectively). There was also a higher proportion of patients with intermediate-high risk in patients with deterioration compared to those without deterioration (P<0.001) (Table 1).
Results of PSM
A total of 178 patients were diagnosed with MPA embolism. Among them, 51 patients were diagnosed with saddle MPA embolism (12 peripheral embolisms and 39 non-peripheral embolisms), and 127 patients were diagnosed with non-saddle MPA embolism. Totally 549 patients were diagnosed with non-MPA embolism. After PSM, the four groups were formed based on demographics, baseline characteristics, and pulmonary embolism severity (supplementary Tables 4, 5, 6, and 7).
Efficacy of MPA embolism for predicting deterioration
When 153 MPA embolism patients and 153 non-MPA embolism patients were matched, univariate and multivariate analyses revealed that MPA embolism and intermediatehigh risk were predictors of deterioration (HR1.96, 95% confidence interval [CI] 1.01-3.83,P=0.047 andHR5.85, 95%CI1.98-17.30,P=0.001, respectively) (Table 2). The Kaplan-Meier survival curve for MPA embolism revealed that MPA embolism patients had a higher risk of deterioration than non-MPA embolism patients (log-rank test=5.23,P=0.022) (Figure 2A).
To exclude the influence of saddle MPA embolism, 110 non-saddle MPA embolism patients and 110 non-MPA embolism patients were matched. The univariate and multivariate analyses revealed that MPA embolism and intermediate-high risk were independent predictors of deterioration (HR2.34, 95%CI1.07-5.15,P=0.034 andHR5.99, 95%CI1.36-26.45,P=0.018, respectively) (Table 2). The Kaplan-Meier survival curve for MPA embolism revealed that the MPA embolism patients had a higher risk of deterioration than non-MPA embolism patients (log-rank test=4.70,P=0.030) (Figure 2B).
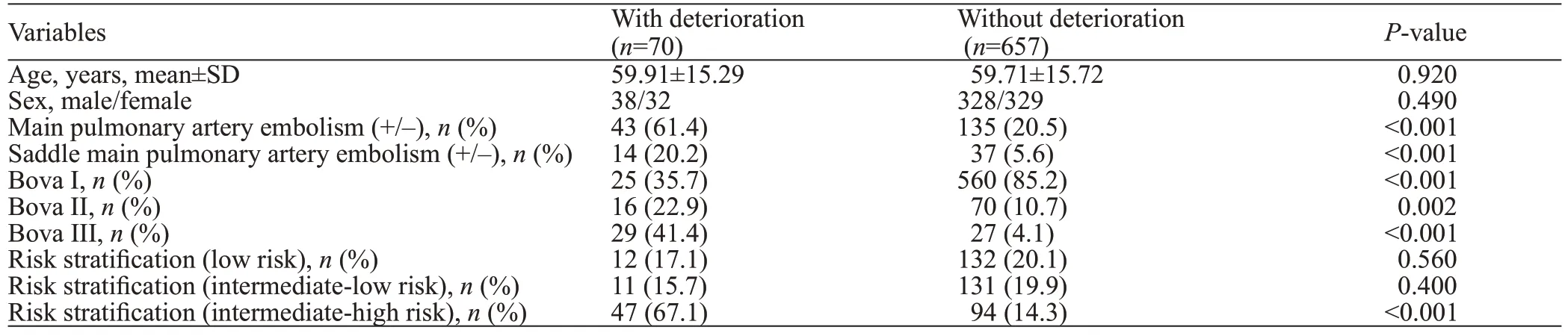
Table 1. Baseline and other characteristics before propensity score matching (n=727)

Table 2. Prognostic factors associated with deterioration
Efficacy of saddle MPA embolism for predicting deterioration
To evaluate whether saddle MPA was an independent predictor of deterioration in MPA embolism patients, 49 saddle MPA embolism patients were matched with 98 nonsaddle MPA embolism patients. We found that saddle MPA embolism was not an independent predictor of adverse events in MPA embolism patients (Table 2). There was no statistical significance between saddle MPA embolism and non-saddle MPA embolism patients on the Kaplan-Meier survival curve (log-rank test=1.20,P=0.729) (Figure 2C).
To evaluate whether saddle MPA patients had a higher risk of deterioration compared to non-MPA embolism patients, 51 saddle MPA patients and 102 non-MPA patients were matched. There was no statistical signifi cance between the groups in either the univariate or multivariate analysis (Table 2). There was no statistical significance between saddle MPA embolism and non-MPA embolism patients (log-rank test=3.17,P=0.077) (Figure 2D).
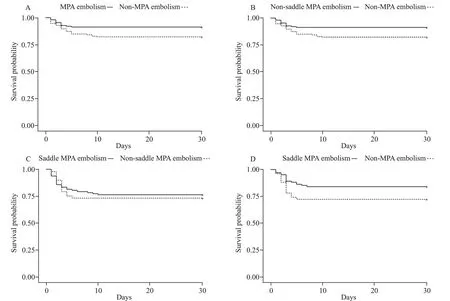
Figure 2. Kaplan-Meier curves. A: following PSM, MPA embolism and non-MPA embolism patients were compared (log-rank test=5.23, P=0.022); B: following PSM and exclusion of saddle MPA embolism patients, non-saddle MPA embolism and non-MPA embolism patients were compared (log-rank test=4.70, P=0.030); C: following PSM, saddle MPA embolism and non-saddle MPA embolism patients are compared (log-rank test=1.20, P=0.729); D: following PSM, saddle MPA embolism and non-MPA embolism patients were compared (log-rank test=3.17, P=0.077); MPA: main pulmonary artery; PSM: propensity score matching.
Thrombus stability of saddle MPA embolism
The thrombus splintering was 4.02±3.83 points in all saddle MPA embolism patients, 7.50±3.06 points in saddle MPA embolism patients with deterioration, and 2.70±3.20 points in saddle MPA embolism patients without deterioration. These differences were statistically significant between deterioration and non-deterioration patients (P<0.001). Thrombus splintering was a discriminatory factor for deterioration (the area under the ROC curve 0.866, 95%CI0.735-0.997,P<0.001) and the optimal cut-off value was 5.5 points (sensitivity 85.7% and specifi city 86.5%) (Figure 3).
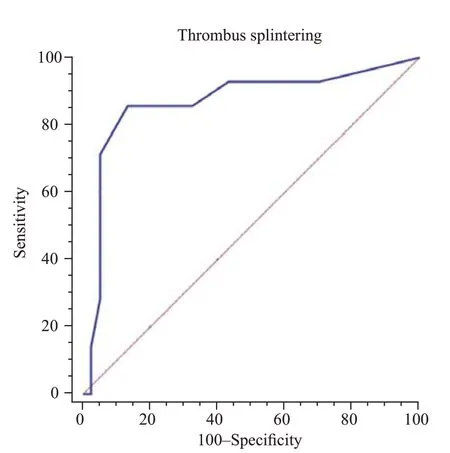
Fi gure 3. ROC curve of thrombus splitting for prediction of deterioration in saddle MPA embolism patients (the area under the ROC 0.866, 95% CI 0.735-0.997, P<0.001). MPA: main pulmonary artery; ROC: receiver operating characteristic; CI: confi dence interval.
DISSCUSION
Deterioration is related to circulation collapse in nonhigh-risk patients with acute PE.[19]Heart rate, systolic pressure, RVD, cTn-I, and NT-proBNP are all recognized as predictors of such circulation collapse.[2]A combination of several predictors is useful for identifying patients at a high risk of deterioration, including Bova scores[6]and risk stratifi cation.[2]If a novel method could improve the predictive ability of deterioration in non-high-risk acute PE patients in conjunction with these two methods above, it would be a beneficial supplement for the management of acute PE patients. Identification of thrombus location meets this requirement. Therefore, we designed this study to evaluate the correlation between thrombus location and deterioration using PSM for age, sex, Bova scores, and risk stratification. The results of our study revealed that MPA embolism was a sign of a high risk of deterioration, regardless of the inclusion or exclusion of saddle MPA embolism. Saddle MPA embolism may not be a sign of a high risk of deterioration. Al though there is no diff erence between saddle MPA embolism and non-MPA embolism in the risk of deterioration, this statistically non-significant difference is not enough to say saddle MPA embolisms are as safe as non-MPA embolisms. We suggest that the saddle MPA embolism should be considered at a similar risk of deterioration as MPA embolism, but it is not necessary to consider it as a special subtype with a higher risk of deterioration than MPA embolism.
Previous studies have shown a poor short-term prognosis in MPA embolism patients.[7,8]Our study supported this view. Regardless of the inclusion or exclusion of saddle MPA embolism, patients with MPA embolism had a higher risk of deterioration than those with non-MPA embolism in our study. In regards to anatomy, it was in series between MPA and relative peripheral pulmonary arteries, and it was in parallel among the peripheral pulmonary arteries. MPA embolism occurs only if its downstream pulmonary artery provides the resistant point. This resistant point is provided by the bifurcation of the pulmonary artery in different grades of the pulmonary artery or the peripheral pulmonary artery with a similar size to the thrombus.[8,13]Based on the physiopathology above, in general, MPA embolism is combined with peripheral pulmonary embolism (non-MPA embolism). If the thrombus was located at the MPA, dominantly subsegment pulmonary arteries would also be blocked[8]and severe inflammation[20]would be activated, causing the peripheral pulmonary artery to constrict and aggravate the severity.[21]This is why MPA embolism presents a higher risk of deterioration than non-MPA embolism.
There has been no consensus on the correlation between saddle MPA embolism and deterioration in non-high-risk acute PE. A study has revealed that saddle MPA embolism represents a poor short-term prognosis,[22]but in our study, saddle MPA was not a sign of a high risk of deterioration. Several factors may have led to diff erent conclusions. First, the diversity of enrolled patients can cause diff erent conclusions. Most studies, including ours, chose non-high-risk patients as the study population. These studies may underestimate the incidence rate of saddle MPA embolism because some highrisk acute PE patients with saddle MPA embolism might have a quick death and not be able to complete the CTPA for diagnosis.[13]In high-risk patients with acute PE, shock is the first distinguishable characteristic for making a clinical decision regarding where the thrombus is located in the pulmonary artery. Therefore, identification of the thrombus location is clinically significant only in non-high-risk acute PE patients. Second, due to the low incidence of saddle MPA embolism, previous studies could not compare saddle MPA embolism to other thrombus locations at the same baseline and PE severity. To avoid this imbalance, we used PSM to evaluate the correlation between saddle MPA embolism and deterioration to estimate the risk of deterioration. Alth ough the saddle MPA embolism represents clot location both in MPA and MPA bifurcation, MPA bifurcation section is larger than other section.[23]If a thrombus is mainly located at the MPA bifurcation and only spitted into a few fragments, it would only mildly impede pulmonary circulation. Meanwhile, if the thrombus is located at the MPA bifurcation, combining many fragments, it would seriously impede pulmonary circulation. We inferred only saddle MPA embolism with many fragments, which leads to multi-pulmonary artery blockages and presents a high risk of deterioration. To test this hypothesis, we calculated the accumulated amount of peripheral pulmonary arteries with the thrombus as a measure of thrombus splintering. This revealed that most saddle MPA embolisms showed low thrombus splintering and only a few fragments in the peripheral pulmonary artery. Saddle MPA embolisms with a large number of thrombus fragments showed a high risk of deterioration.
There were several limitations to our study. Although we matched saddle MPA embolism patients with others, the number of patients with saddle MPA embolism remained small. Furthermore, this study was retrospective. These factors may limit the generalizability and statistical strength of the results. Although we did attempt to minimize selection bias using PSM for age, sex, Bova score, and risk stratification, larger studies are needed to reduce this potential bias.
CONCLUSIONS
In non-high-risk acute PE patients, the presentation of MPA embolism is associated with a higher risk of deterioration compared to non-MPA embolisms. Saddle MPA embolism is not a sign of a high risk of deterioration unless combined with thrombi blockage in multi-peripheral pulmonary arteries.
Funding:The study was supported by the 345 Talent Project, Shengjing Hospital of China Medical University.
Ethical approval:This research was approved by the Institutional Review Board of Shengjing Hospital of China Medical University and the requirement for informed consent was waived owing to the retrospective nature of the research (202PS292K).
Confl icts of interests:There is no confl ict of interest.
Contributors:MZ: conception and design; DJ: provision of study materials, collection and assembly of data, and manuscript writing; CJ: data analysis and interpretation; all authors: fi nal approval of manuscrip.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2021年4期
World journal of emergency medicine2021年4期
- World journal of emergency medicine的其它文章
- Fatal and non-fatal injuries due to suspension trauma syndrome: A systematic review of defi nition, pathophysiology, and management controversies
- Two-point compression ultrasonography: Enough to rule out lower extremity deep venous thrombosis?
- High-fl ow nasal cannula oxygen therapy and noninvasive ventilation for preventing extubation failure during weaning from mechanical ventilation assessed by lung ultrasound score: A single-center randomized study
- Comparison of clinical characteristics in patients with coronavirus disease and infl uenza A in Guangzhou, China
- Development of septic shock and prognostic assessment in critically ill patients with coronavirus disease outside Wuhan, China
- Protective eff ect of extracorporeal membrane pulmonary oxygenation combined with cardiopulmonary resuscitation on post-resuscitation lung injury
