Exploration of transmission chain and prevention of the recurrence of coronavirus disease 2019 in Heilongjiang Province due to inhospital transmission
Qi Chen, Yang Gao, Chang-Song Wang, Kai Kang, Hong Yu, Ming-Yan Zhao, Kai-Jiang Yu
Qi Chen, Chang-Song Wang, Department of Critical Care Medicine, Harbin Medical University Cancer Hospital, Harbin Medical University, Harbin 150081, Heilongjiang Province, China
Yang Gao, Department of Critical Care Medicine, The sixth Affiliated Hospital of Harbin Medical University, Harbin Medical University, Harbin 150028, Heilongjiang Province, China
Kai Kang, Ming-Yan Zhao, Kai-Jiang Yu, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin Medical University, Harbin 150001,Heilongjiang Province, China
Hong Yu, Department of Critical Care Medicine, The Second Hospital of Harbin, Harbin 150056, Heilongjiang Province, China
Kai-Jiang Yu, Institute of Critical Care Medicine, The Sino Russian Medical Research Center of Harbin Medical University, Harbin 150081, Heilongjiang Province, China
Kai-Jiang Yu, Key Laboratory of Hepatosplenic Surgery, Ministry of Education, Harbin 150001,Heilongjiang Province, China
Kai-Jiang Yu, The Cell Transplantation Key Laboratory of National Health Commission, Harbin 150001, Heilongjiang Province, China
Abstract The coronavirus disease 2019 (COVID-19) epidemic is a major public health emergency characterized by fast spread, a wide range of infections, and enormous control difficulty. Since the end of December 2019, Wuhan has become the first core infection area of China's COVID-19 outbreak. Since March 2020, the domestic worst-hit areas have moved to the Heilongjiang Province due to the increased number of imported COVID-19 cases. Herein, we reported the major COVID-19 outbreak, which caused a rebound of the epidemic in Harbin, China. After the rebound, different levels of causes for the recurrence of COVID-19, including citylevel, hospital-level, and medical staff-level cause, were investigated. Meanwhile,corresponding countermeasures to prevent the recurrence of the epidemic were also carried out on the city level, hospital level, and medical staff level, which eventually showed the effect of infection control function in a pandemic. In this study, we described the complete transmission chain, analyzed the causes of the outbreak, and proposed corresponding countermeasures from our practical clinical experience, which can be used as a valuable reference for COVID-19 control.
Key Words: Transmission chain; Prevention of the recurrence; COVID-19; Heilongjiang Province; In-hospital transmission
INTRODUCTION
With the continuous decline in the number of newly confirmed and existing coronavirus disease 2019 (COVID-19) patients in China, the epidemic can be considered as successfully conquered. Consequently, the current focus is on the strict control of imported cases from overseas and the prevention of their spread. In April 2020, a clustering severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)infections occurred in two general tertiary hospitals in Harbin city, resulting in 66 newly confirmed patients and 21 asymptomatic patients, among whom 8 patients were the medical staff. These confirmed and asymptomatic COVID-19 patients have come in contact with other patients, family caregivers, and medical staff as they were treated in the same ward with the other patients. The recurrence of the epidemic led to the complete closure of the Second Hospital of Harbin on April 20, and even caused the inter-provincial transmission to Liaoning Province and the Inner Mongolia Autonomous Region. In these two hospitals, the in-hospital infection seriously affected residents' normal lives and disrupted the plan for the resumption of work and production. This study aimed to describe the complete transmission chain, analyze the causes of the outbreak, and propose corresponding countermeasures based on our practical clinical experience that can, later on, be used for reference.
COMPLETE TRANSMISSION CHAIN DESCRIPTION
This transmission chain's core patient was an 87-year-old male with a stroke who was admitted to the Second Hospital of Harbin (Hospital 1 in the Figure 1) from April 2 to April 6. The patient was transferred to the respiratory department in the First Affiliated Hospital of Harbin Medical University (Hospital 2 in the Figure 1) due to fever during hospitalization. He came in contact with a number of people 4 d before admission during dinner, including passer B. There was a clear contact history between passer B and passer A, who was later on diagnosed as COVID-19 confirmed patient. Passer A was a neighbor of a United States returned compatriot who tested positive for the two consecutive serum immunoglobulin G (IgG) antibody against SARS-CoV-2. The schematic diagram of the complete transmission chain is shown in Figure 1.
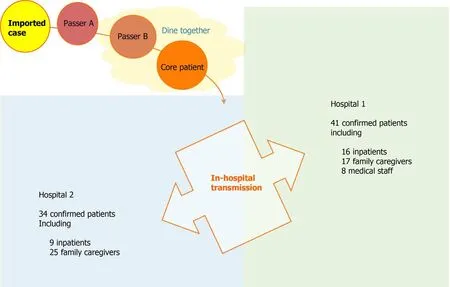
Figure 1 The schematic diagram of the complete transmission chain. The schematic diagram of complete transmission chain shows that in-hospital infections occurred in two hospitals. Hospital 1 had a total of 41 confirmed patients, including 16 inpatients, 17 family caregivers, and 8 medical staff. Hospital 2 had a total of 34 confirmed patients, including 9 inpatients and 25 family caregivers.
The returned compatriot, a neighbor of passer A, returned from the epidemic area in the United States and underwent detection of SARS-CoV-2 nucleic acids two times within 14 d after entry, each time testing negative. At present, the main detection method for SARS-CoV-2 includes the detection of viral nucleic acids on oropharyngeal and/or nasopharyngeal swabs[1,2]. However, in practice, false-positives and negatives have been reported to occur[3-5]. This imported case provided further support for the premise that if two consecutive negative results of viral nucleic acid on respiratory samples were taken as the exclusion criterion, they would still lead to about 10%missed diagnosis, eventually resulting in the spread of the epidemic[6]. On the 22ndday after entry, the third detection of SARS-CoV-2 nucleic acids was still negative, but the serum IgG antibody was positive and remained to be positive on the next day.Therefore, this United States returned compatriot was identified as being previously infected with COVID-19. Dr. Zhang, the president of Harbin Medical University,pointed out that the whole genome sequence of SARS-CoV-2 in 21 patients from two batches of samples was 99.99% identical and thus from the same transmission chain.Furthermore, the genome sequence of SARS-CoV-2 in this transmission chain was different from that previously detected in the Chinese population through gene sequencing analysis. Considering the evidence of genome sequencing analysis and epidemiological investigation, the returned compatriot from the United States was identified as the outbreak's infection source.
SARS-CoV-2 has been defined as a highly pathogenic human coronavirus. Humanto-human spreadviadroplets, aerosol, contaminated hands, or surfaces contact among close contacts has been identified as the main transmission way[7-20],especially in closed environments. The aforementioned returned compatriot, identified as the infection source in this transmission chain, shared the same elevator with passer A,and may have the possibility of engaging in face-to-face contact.
DIFFERENT LEVELS OF CAUSES FOR THE RECURRENCE OF COVID-19
City-level cause
The emergency response level of epidemic prevention and control in Heilongjiang Province had been adjusted from the second-level response to the third-level response from 18:00 on March 25. The gradual improvement in the COVID-19 epidemic and the urgent desire to normalize life and resume work and production reduced people's vigilance against the recurrence of the epidemic. Social dining, which included core patient and passer B, took place on March 29. In addition, the returned compatriot in the transmission chain returned to Harbin from the United States on March 19. The quarantine measure of entry personnel implemented at that time was home quarantine for 14 d. On the 8thand 9thd after suspending home quarantine, the serum IgG antibody was positive two consecutive times. This occurrence suggests the quarantine measure of entry personnel at that time was worth discussing and improving.
Hospital-level cause
Hospitals, especially general tertiary hospitals, are the first place for COVID-19 patients to seek medical support. Consequently, they are highly populated and with the highest risk of in-hospital infection spread[11], which is consistent with previous reports on SARS-CoV and Middle East respiratory syndrome CoV[12-14]. Still, this was not reflected in the management policy of the two hospitals at that time due to insufficient awareness and lack of vigilance. First of all, when the core patient developed a fever and was transferred to the First Affiliated Hospital of Harbin Medical University, there was no timely detection of SARS-CoV-2 nucleic acid.Consequently, this resulted in the failure to identify COVID-19 patients as early as possible and to prevent timely in-hospital infection spread. Moreover, there was no strict limit on the number of admitted patients and their family caregivers, which further facilitated the outbreak of the epidemic and propagation out of the hospital.Also, the mobility of admitted patients and their family caregivers across different rooms and wards was not strictly controlled. Finally, undiagnosed patients with fever and pulmonary imaging changes were not arranged in a single isolation area similar to the buffer zone. Obviously, the kind of confined space in the hospital ward is highly susceptible to cause the spread of in-hospital infection. Numerous omissions in hospital management policies have resulted in the disastrous consequence of 1-to-87.
Medical staff-level cause
Like most other people in Harbin city, most medical staff believed that the COVID-19 epidemic was over at that time and lacked vigilance against the recurrence of the epidemic. Therefore, when the core patient with fever and pulmonary imaging changes was transferred from another hospital and admitted to our hospital, the patient's symptoms were considered to be associated with other conditions as the possibility of COVID-19 was arbitrarily ruled out. Moreover, medical staff did not have enough knowledge of COVID-19 or the hospital's relevant rules and regulations,especially those in the departments with low correlation with COVID-19.
CORRESPONDING COUNTERMEASURES TO PREVENT THE RECURRENCE OF EPIDEMIC
City-level countermeasures
To date, there is no available and effective antiviral treatment for COVID-19 patients other than supporting care[15].Controlling population mobility and thus cutting off the transmission route is still the most effective way to prevent and control the spread of the epidemic, which has been effectively confirmed in the early battle against COVID-19[16]. Therefore, following the recurrence of epidemic, moderate crowd control policies were again restored, such as banning eating in restaurants, closing public places, and taking new quarantine and detection measures of entry personnel,also known as “14 + 7 + 14”. The latter stands for 14 d of centralized isolation and 2 times of nucleic acid detection, and 7 d of centralized isolation and one time of nucleic acid detection, which should be carried out at the entry place and the local region,respectively, followed by 14 d of home isolation and observation that should be implemented and incorporated into the grid management of the local community.Home isolation was based on the principle “one person, one house”, and those who did not meet the requirements were required to continue centralized isolation for 14 d.The supervision was jointly conducted by the local public security and the community.
Hospital-level countermeasures
Close contacts of the core patient were immediately isolated and subjected to related tests, including temperature, whole blood cell analysis, pulmonary computed tomography (CT) scan, nucleic acid, and antibodies of SARS-CoV-2. The inpatient building where the in-hospital infection had occurred was completely emptied, sealed off, and disinfected. In addition to inquiring on epidemiological history and initial symptoms, “five tests”, namely temperature, whole blood cell analysis, pulmonary CT scan (except for special groups, such as pregnant women and children), nucleic acid,and antibodies of SARS-CoV-2, were necessary for admission of all patients and their family caregivers. If emergency patients did not complete “five tests”, they needed to be admitted to a single room in the buffer zone and could be transferred to the general ward only after COVID-19 was excluded. Three-grade prevention measures are quite indispensable in the buffer zone to avoid SARS-CoV-2 infection in clinical practice.The detection ability of SARS-CoV-2 nucleic acid in our hospital has been greatly enhanced, and the results could be obtained in only 6 h. Therefore, the buffer zone had sufficient capacity to receive emergency patients.
In principle, family caregivers are not allowed in our hospital during this special period. In case of need, one family caregiver, who is designated as a fixed caregiver,must complete “five tests” before admission. All general wards have been transformed into single rooms with independent toilets. Patients or their family caregivers can pay online bills, order meals, and purchase daily necessities through a phone app without leaving a room. These items are delivered and distributed by hospital staff. Patients without special needs are not allowed to leave the room,and visitors are refused.Each general ward is under 24-h closed management, and the access of personnel is strictly controlled and supervised by security guards. The auxiliary inspections are carried out in different time periods by an appointment system. All of the above measures are implemented to limit the mobility of admitted patients and their family caregivers across different rooms and wards and to avoid personnel aggregation in public places.The public areas in the hospital are regularly and thoroughly disinfected. After admission to the general wards, the temperature is daily measured, while whole blood cell analysis, pulmonary CT scan, nucleic acid, and antibodies of SARS-CoV-2 are regularly performed in all patients to further exclude COVID-19. All medical staff in our hospital underwent screening on nucleic acid and antibodies of SARS-CoV-2,which were conducive to exclude asymptomatic carriers and prevent further inhospital transmission[17,18]. All these efforts were made with the aim to break the transmission chain in the hospital and make a trade-off between resuming work and preventing in-hospital infection. Looking carefully from the history of human coronaviruses, we may have found the answers we were searching from existing experiences and lessons, which might give us some hint on future studies[14,18-20].
Medical staff level countermeasures
The 1-to-87 in-hospital infection has led medical staff to attach great importance to the recurrence of the COVID-19 epidemic. Adequate learning, training, and assessment enable medical staff to understand fully COVID-19 and master the relevant rules and regulations so as to avoid the recurrence of similar in-hospital infections. The learning,training, and assessment should be periodically repeated. Although there is vaccination hesitancy in the early clinical application of the vaccine, universal vaccination will be the most effective measures to prevent large COVID-19 outbreaks again in the future. At the moment, studies on effectiveness, timeliness, and safety of SARS-CoV2 vaccine are needed, because the most promising incentives for improving the likelihood of vaccination uptake is the vaccine proved to be effective and available[21]. It is necessary for medical staff to be vaccinated with SARS-CoV2 vaccine to protect themselves and prevent hospital transmission.
CONCLUSION
This in-hospital recurrence of COVID-19 in Heilongjiang province further deepens our understanding and knowledge of SARS-CoV-2 and infectivity of COVID-19. A detailed and accurate understanding of different causes for the recurrence of the epidemic at different levels, including city, hospital, and medical staff, can help to improve the prevention and control of COVID-19 and be used as a valuable reference for other medical staff.
Taking the possibility of long co-existence of SARS-CoV-2 with human beings into consideration, this work should be continuously carried out and improved. More practices and experiences are needed to achieve a perfect balance between resuming work and preventing in-hospital infection recurrence.
ACKNOWLEDGEMENTS
We are grateful to all colleagues who worked with us in the coronavirus disease 2019 treatment center of Heilongjiang Province and all those who provided selfless advice and help for this article. We pay tribute to the medical staff who lost their lives in the national fight against the epidemic. Data and information in this article mainly came from the official website of the Health Commission of Heilongjiang Province.http://wsjkw.hlj.gov.cn/.
 World Journal of Clinical Cases2021年20期
World Journal of Clinical Cases2021年20期
- World Journal of Clinical Cases的其它文章
- Obesity in people with diabetes in COVID-19 times: Important considerations and precautions to be taken
- Revisiting delayed appendectomy in patients with acute appendicitis
- Detection of short stature homeobox 2 and RAS-associated domain family 1 subtype A DNA methylation in interventional pulmonology
- Borderline resectable pancreatic cancer and vascular resections in the era of neoadjuvant therapy
- Esophageal manifestation in patients with scleroderma
- Effects of nursing care in fast-track surgery on postoperative pain,psychological state, and patient satisfaction with nursing for glioma
