Cellular based treatment modalities for unresectable hepatocellular carcinoma
Konstantinos Damiris, Hamza Abbad, Nikolaos Pyrsopoulos
Konstantinos Damiris, Hamza Abbad, Department of Medicine, Rutgers New Jersey Medical School, Newark, NJ 07103, United States
Nikolaos Pyrsopoulos, Department of Medicine, Division of Gastroenterology and Hepatology,Rutgers New Jersey Medical School, Newark, NJ 07103, United States
Abstract Hepatocellular carcinoma (HCC) is the most common primary malignancy of the liver and is unfortunately associated with an overall poor prognosis and high mortality. Early and intermediate stages of HCC allow for treatment with surgical resection, ablation and even liver transplantation, however disease progression warrants conventional systemic therapy. For years treatment options were limited to molecular-targeting medications, of which sorafenib remains the standard of care. The recent development and success of immune checkpoint inhibitors has proven to be a breakthrough in the treatment of HCC, but there is an urgent need for the development of further novel therapeutic treatments that prolong overall survival and minimize recurrence. Current investigation is focused on adoptive cell therapy including chimeric antigen receptor-T cells (CAR-T cells), T cell receptor (TCR) engineered T cells, dendritic cells, natural killer cells, and tumor infiltrating lymphocyte cells, which have shown remarkable success in the treatment of hematological and solid tumor malignancies. In this review we briefly introduce readers to the currently approved systemic treatment options and present clinical and experimental evidence of HCC immunotherapeutic treatments that will hopefully one day allow for revolutionary change in the treatment modalities used for unresectable HCC. We also provide an up-to-date compilation of ongoing clinical trials investigating CAR-T cells, TCR engineered T cells, cancer vaccines and oncolytic viruses, while discussing strategies that can help overcome commonly faced challenges when utilizing cellular based treatments.
Key Words: Hepatocellular carcinoma; Immunotherapy; Immune cells; Adoptive T cell therapy; Chimeric antigen receptor-T cell; Clinical trials
INTRODUCTION
Hepatocellular carcinoma (HCC) is a malignant primary tumor of the liver, accounting for approximately ninety percent of total liver tumor cases worldwide[1]. HCC commonly occurs in patients with preexisting liver cirrhosis, chronic hepatitis B virus(HBV), chronic hepatitis C virus (HCV), heavy alcohol consumption, aflatoxin exposure and metabolic associated fatty liver disease associated with diabetes and metabolic syndrome[2]. According to the Global Cancer Observatory (GLOBOCAN) in 2020, HCC is considered the 6thmost common cancer worldwide, with the highest incidence in eastern Asia and Africa[3]. It has been estimated that by 2025, there will be more than one million individuals diagnosed with liver cancer annually[4].Worldwide incidence of HCC has shown a greater predominance among men in comparison to women, with most diagnoses made in patients over the age of 60 years old[5]. HCC risk factors in the United States have varied significantly over the last two decades, with a majority of cases currently related to chronic HCV infection[6].
Management of HCC varies depending on the staging status of the tumor according to the standardized Barcelona-Clinic Liver Cancer (BCLC) system endorsed by both the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases[7]. Locally diagnosed tumors (BCLC stages 0-A), which are small in size (≤ 3 cm), early in progression, and limited to the liver parenchyma are amendable to surgical resection, radiofrequency ablation or ideally liver transplantation[8], with a median survival rate of 60 mo[9]. Advanced HCC on the other hand is defined by a significant increase in tumor size, vascular invasion and/or metastatic disease that is not amenable to loco-regional therapy (BCLC Stage C-D)[10], warranting treatment with systemic therapy[11]. In cases necessitating liver transplantation,the Milan criteria has been adopted by The United Network for Organ Sharing in order to determine eligibility[12], however this approach is limited by organ availability[13].
For over a decade, sorafenib has been considered the first line systemic treatment for advanced HCC. More recently, other systemic treatments such as the tyrosine kinase inhibitors (lenvatinib, regorafenib, and cabozantinib), immune checkpoint inhibitors (ICIs) (atezolizumab, ipilimumab, nivolumab, pembrolizumab) and the monoclonal antibody ramucirumab have been approved as first- and second-line treatment options[14]. With only modest established improvement in overall survival(OS) and an assortment of adverse effects, there has been a recent push for the development of immunobiological treatments, which first demonstrated efficacy in the treatment of hematological cancers. Treatments include chimeric antigen receptor-T cells (CAR-T cells), T cell receptor (TCR) engineered T cells, dendritic cells (DC),natural killer (NK) cells, and tumor infiltrating lymphocyte (TIL) cellular therapies(Figure 1). In this article we will review the novel range of cellular based treatments for HCC non-amenable to loco-regional therapy and introduce readers to various preclinical and clinical trials investigating their efficacy.
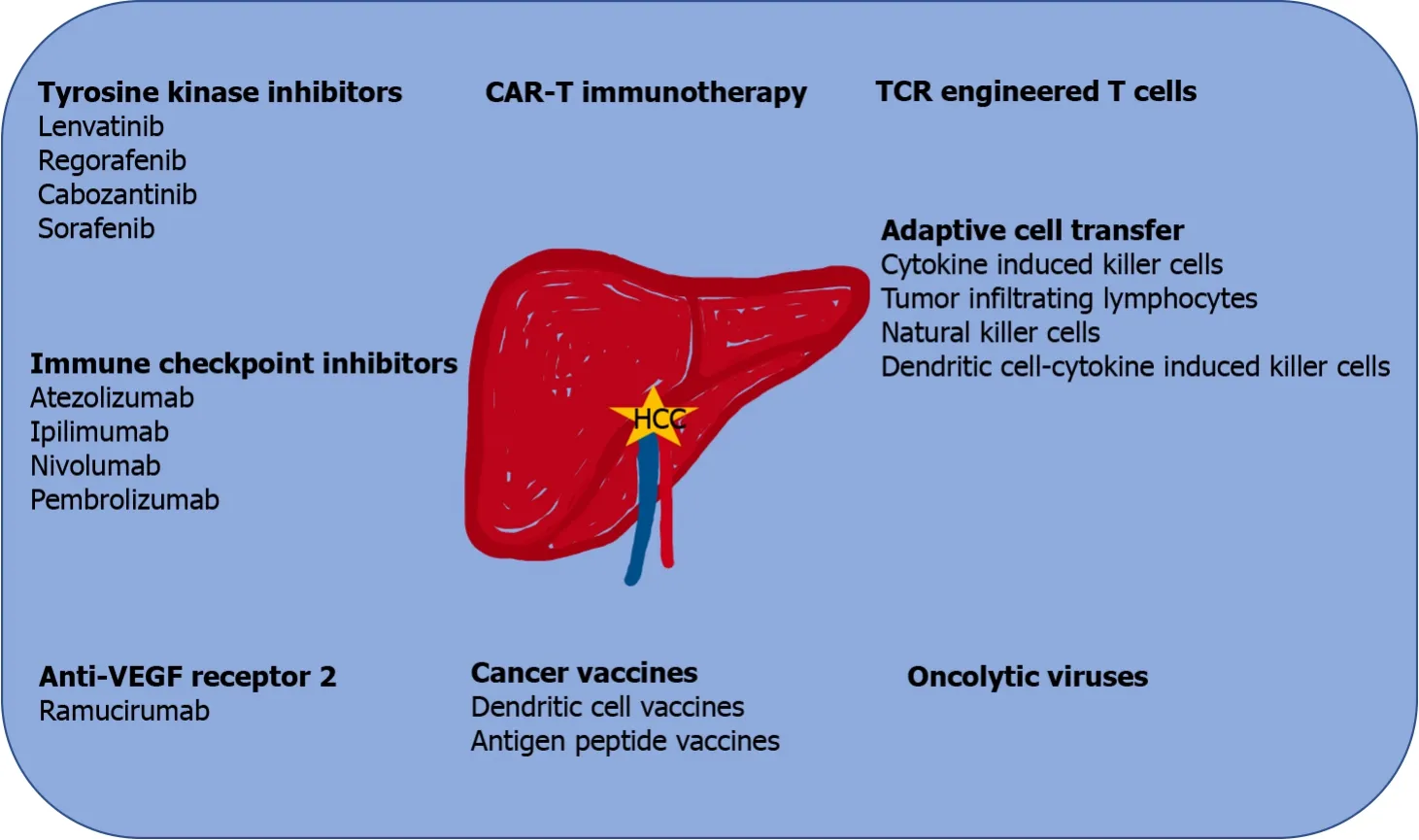
Figure 1 Treatment modalities available for unresectable (advanced) hepatocellular carcinoma, which is non-amendable to loco-regional therapies. CAR: Chimeric antigen receptor; HCC: Hepatocellular carcinoma; TCR: T cell receptor; VEGF: Vascular endothelial growth factor.
SYSTEMIC THERAPIES: APPROVED FIRST LINE THERAPIES
Sorafenib
Sorafenib is a multi-kinase inhibitor that inhibits cellular proliferation and angiogenesis through its effects on various receptor tyrosine kinases including vascular endothelial growth factor (VEGF), platelet derived growth factor (PDGF) and c-kit[15]. Its efficacy was demonstrated in two large phase III randomized controlled trials;SHARP conducted in the United States and Europe, and a similar study conducted in the Asia- Pacific focusing on patients with unresectable and advanced HCC[16]. In the SHARP trial, median OS was increased to 10.7 mo compared to 7.9 mo in placebo[17].Similar findings were demonstrated in the Asia-Pacific trial; median OS increased in the treatment group (6.5 movs4.2 mo) and time-to-progression (TTP) was also significantly greater (2.8 movs1.4 mo)[18]. These findings led to sorafenib being approved by the Food and Drug Administration (FDA) in 2007, making it the standard of care and first line treatment option of advanced HCC[15,19].
Lenvatinib
Lenvatinib is another inhibitor of multiple receptor tyrosine kinases that has recently gained much attention[20]. In the randomized, open-label, non-inferiority phase III trial (REFLECT), lenvatinib was compared to sorafenib in patients who were deemed to have non-resectable HCC. Findings indicated an improved median OS of 13.6 mo with lenvatinib, compared to 12.3 mo with sorafenib. Lenvatinib also demonstrated an increase in median progression-free survival (PFS) and overall response rate (ORR)[21]. This allowed for FDA approval in 2018 as a fist line agent for treatment of unresectable HCC[22].
SYSTEMIC THERAPIES: APPROVED SECOND LINE THERAPIES
Ramucirumab
The phase III randomized controlled trial REACH (NCT01140347) investigated ramucirumab, a monoclonal antibody against VEGF receptor 2. While the study failed to demonstrate prolonged OS in the entire cohort, patients with elevated serum alphafetoprotein (AFP) (> 400 ng/mL) had significantly longer median OS when compared to placebo (7.8 movs4.2 mo,P= 0.006)[23]. A subsequent phase III study, REACH-2(NCT02435433) reported a significantly prolonged median OS (8.5 movs7.3 mo) in sorafenib-experienced patients receiving ramucirumabvsplacebo with AFP of 400 ng/mL or greater[24]. These findings showed promise as an effective treatment option in those with elevated AFP, leading to FDA approval in May 2019.
Regorafenib
Regorafenib is a multikinase inhibitor that inhibits various molecules including VEGF receptor 2/3, PDGF receptor and fibroblast growth factor receptor 1[25]. In the randomized, double-blind, phase III clinical trial RESORCE (NCT01774344) patients who failed sorafenib therapy were assigned to receive regorafenibvsplacebo. This study determined that regorafenib significantly improved OS in individuals who experienced radiological progression of HCC during sorafenib treatment (10.6 movs7.8 mo,P< 0.0001)[26]. Based on the promising findings of the RESORCE trial and a tolerable safety profile, the FDA approved regorafenib as a second line treatment option in those who have HCC progression while on sorafenib or who are not eligible for alternative therapy[25].
Cabozantinib
A double-blind, phase III clinical trial CELESTIAL (NCT01908426) was conducted testing cabozantinib, a multikinase inhibitor, in patients with unresectable HCC who had progressed with sorafenib. The study demonstrated a significant prolongation of OS when compared to placebo (10.2 movs8.0 mo,P= 0.005) coupled with a longer median PFS when compared to placebo[27].Based on the findings of CELESTIAL, the FDA approved cabozantinib as a second line treatment option for HCC in those who have undergone previous therapy with sorafenib.
IMMUNOTHERAPY: ICIS
Limited efficacy and undesirable side effects of traditional therapies (i.e., sorafenib)have led to further investigation of immunotherapeutic agents over the years. A recent and emerging field of treatment includes cancer immunotherapies using ICIs that target programmed cell death protein-1 and its ligand (PD-1/PD-L1) and cytotoxic Tlymphocyte-associated protein- 4 (CTLA-4), which has significantly altered treatment of various types of cancer including HCC[28].
Immune checkpoint molecules play essential roles in regulating cancer cell interactions with the host immune system; and the development of drugs that suppress these interactions used by tumor cells to evade host immunity has shown promising results. PD-1, a member of CD28, is expressed on activated immune cells including T cells, B cells, and myeloid cells; and its interaction with ligand PD-L1 negatively regulates the immune system through suppressive signals that induce peripheral tolerance[29]. In HCC tumor cells, PD-L1 is aberrantly expressed, allowing for such an escape from host immunity[30]. CTLA-4 is another member of the CD28 family, and it is induced on T cells by antigen activation leading to subsequent binding with CD80 and CD86 with more affinity compared to CD28, negatively regulating costimulatory T cell signals and allowing for peripheral tolerance[31]. Ultimately these immunotherapeutic drugs strategically suppress key checkpoints that may be used by tumor cells to evade the host immune system, hindering a hallmark for tumor progression.
Atezolizumab
Atezolizumab is a fully humanized monoclonal antibody targeting PD-L1 that has recently changed the treatment landscape of unresectable HCC. A phase-Ib study evaluating synergistic atezolizumab and bevacizumab (anti-VEGF antibody) in patients with previously untreated and unresectable HCC not only demonstrated an acceptable safety profile, but promising antitumor activity with ORR 36%, disease control rate (DCR) 71%, and a median PFS of 7.3 mo when compared to monotherapy with nivolumab or pembrolizumab[32]. These results led to IMbrave150 (NCT 03434379), an open-label, randomized phase III study assessing atezolizumab (anti-PDL1) in combination with bevacizumab (anti-VEGF antibody) compared to sorafenib in patients with untreated locally advanced or metastatic HCC. OS at 12 mo was significantly longer in the combination group when compared to sorafenib (67.2%vs54.6%) and PFS was significantly longer in atezolizumab + bevacizumabvssorafenib(6.8 movs4.3 mo, hazard ratio for disease progression or death [0.59; 95% confidence interval (CI): 0.47-0.76,P< 0.001], leading to FDA approval in May 2020 for the treatment of unresectable or metastatic HCC who have not received prior systemic therapy[33]. Currently a phase III, multicenter study of atezolizumab plus bevacizumabvsactive surveillance as adjuvant therapy in HCC at high risk of recurrence after surgical resection or ablation is recruiting (IMbrave050; NCT04102098)[34]. In addition, a phase III study evaluating the safety and efficacy of atezolizumab plus levantinib or sorafenibvslevantinib or sorafenib alone in locally advanced or metastatic and/or unresectable HCC following prior treatment with combination atezolizumab and bevacizumab was recently posted in February 2021 (IMbrave251;NCT04770896).
Ipilimumab
Ipilimumab is a monoclonal antibody targeting CTLA-4, which was recently granted accelerated FDA approval in May 2020, when used in combination with nivolumab(anti-PD-1) for HCC that has previously been treated with sorafenib. Approval was based on a single arm of the phase I/II clinical trial CheckMate 040 (NCT01658878), in which patients were treated with nivolumab 3 mg/kg plus ipilimumab 3 mg/kg every 3 wk for 4 doses. In addition to a substantial reduction in tumor burden, the overall ORR was 32%, with median OS 22.8 mo while having manageable safety profiles[35].A phase III trial of ipilimumab in combination with nivolumabvssorafenib or levantinib as first line treatment in patients with advanced HCC is currently recruiting participants (CheckMate 9DW; NCT04039607). A variety of clinical trials evaluating ipilimumab in combination with nivolumab during various treatment phases are ongoing and include; prior to liver resection (PRIME-HCC; NCT03682276), as neoadjuvant therapy (NCT03510871), and in combination with trans-arterial chemoembolization (CheckMate 74W; NCT04340193).
Nivolumab
Nivolumab is an anti-PD-1 monoclonal antibody that has shown promising results,leading to FDA approval for second-line treatment of advanced HCC. The phase I/II clinical trial CheckMate 040 (NCT01658878) investigated nivolumab in sorafenib-naïve and sorafenib-experienced patients with intermediate-advanced HCC and Child-Pugh Stage A. During the dose-expansion phase, ORR was 20%, while DCR was 64% with a median progression free survival of 4.1 mo[36]. The subsequent phase III study CheckMate 459 (NCT2576509) evaluating nivolumabvssorafenib as first line treatments for unresectable HCC failed to demonstrate statistical significance for the primary endpoint of OS[37]. Currently a phase III trial, CheckMate-9DX (NCT 03383458), is actively evaluating recurrence free survival (RFS) in those with HCC at high risk of recurrence after curative hepatic resection or ablation.
Pembrolizumab
Pembrolizumab is a humanized anti-PD-1 monoclonal antibody that has been investigated across a variety of malignancies[38]. The phase II open-label clinical trial KEYNOTE-224 (NCT02702414) studied the safety and efficacy of pembrolizumab in patient with advanced HCC after having failed treatment with sorafenib. Favorable findings included an ORR of 17%, DCR of 61%, along with PFS of 4.8 mo, median OS of 12.9 mo and TTP of 4.9 mo[39]. This promising data led to FDA approval in November 2018 as a second line treatment after sorafenib. A subsequent phase III double-blind, randomized control trial, KEYNOTE-240 (NCT02702401) compared pembrolizumab to placebo, demonstrated longer OS and PFS; however, these findings were not statistically significant and failed to meet primary endpoints[40]. There are currently two-phase III trials that are ongoing at the time of this publication;KEYNOTE-394 (NCT03062358) , evaluating pembrolizumab in Asian patients with systemically treated advanced HCC and KEYNOTE-937 (NCT03867084) as an adjuvant therapy in HCC after curative treatment[29].
Ultimately, cancer uses a variety of unique mechanisms to evade host immune response and to develop drug resistance in HCC. This has sparked much interest in combining treatment modalities, particularly combination ICIs and checkpoint inhibitors with other chemotherapeutics. HIMALAYA (NCT03298451) is an openlabel, multi-center, phase III study assessing durvalumab (anti-PDL1) plus tremelimumab (anti-CTLA4) in patients with advanced HCC. Scientists and physicians alike are eagerly awaiting results of other ongoing phase III trials such as LEAP-002(NCT03713593) evaluating pembrolizumab and levantinib in combination and COSMIC-312 (NCT03755791) investigating atezolizumab and cabozantinib synergistically.
BEYOND CHECKPOINT INHIBITORS
Cell based immunotherapy
In recent years cancer therapy has begun shifting focus from the aforementioned conventional therapies, to the use of immune cell therapies, which utilize the host immune system to target and treat cancer. One such avenue of therapy includes gene modified T cell therapy, particularly TCR engineered T cells and CAR-T cells, which have shown promise in various malignancies and continue to be tested in clinical trials targeting HCC. Below we will discuss the concept of gene modified T cell therapies,and other modalities of adoptive cell transfer while reporting the results of recent and ongoing clinical trials where applicable.
When engineering T-cell based immune cell therapies targeting HCC, identification of tumor-associated antigens (TAAs) that can allow for appropriately mediated immune response is critical. AFP is a glycoprotein composed of 591 amino acids,identified as the first oncofetal biomarker for patients with HCC allowing for quantitative estimation of tumor burden and response to therapy[41]. Elevated levels of AFP have been found in approximately 70% of patients diagnosed with HCC,however elevations can also be found in other pathological conditions including cirrhosis, various hepatic disorders, germ cell tumors, lung cancer, gastric cancer, and pancreatic cancer[42]. Pre-clinical models have demonstrated the potential of AFP in the development of cellular immunotherapies[43,44]. Glypican-3 (GPC-3) belongs to the transmembrane heparan sulfate proteoglycan family, that regulates cellular division and growth[45]. GPC-3 expression is elevated in HCC, and recent studies have demonstrated that elevated levels correlate with an overall worse prognosis[46].Therefore GPC-3 has been investigated in pre-clinical studies as a target for adoptive cell immunotherapy[47,48]. Melanoma antigen gene proteins (MAGE) was first identified in melanoma patients and has been found to be almost exclusively expressed in a variety of cancer tissues. Aberrant expression of MAGE has been demonstrated to significantly correlate with clinical characteristics of HCC, however functions of the multitude of MAGE proteins have yet to be thoroughly understood[49]. New York esophageal squamous cell carcinoma (NY-ESO-1) is a member of the cancer testis antigen family expressed in a variety of cancer cells including HCC[50].NY-ESO-1 has been deemed as the most promising cancer testis antigen for the development of cancer immunotherapy with a multitude of studies demonstrating promising results across a variety of malignancies[51]. When examining HCC caused by viral infection (HBV or HCV) there is prospect in targeting viral antigens as a strategy to etiologically treat HCC. Targets include HBV S or L protein (envelope proteins), which have shown promise by eliminating HBV positive hepatocytes when targeted by antigen specific T cells[52]. Targeting of hepatitis B surface antigen has also shown efficacy in mouse models utilizing CAR-T cell therapy as well[53]. Other tumor antigens that are of particular interest include epithelial cell adhesion molecules(EpCAM)[54], mucin 1 glycoprotein (MUC1)[55] and human telomerase reverse transcriptase (hTERT)[56].
CAR-T and TCR engineered T cells: The basics
Gene modified T cell therapy is a method used to deliver T cells that are genetically engineered to produce TCRs that recognize specific tumor associated antigens and their epitopes. There are currently two methods of developing gene modified T cells,CAR-T cells and TCR transgenic T-cells (engineered T-cells), which have both shown efficacy and promise in a variety of solid and hematological malignancies[57]. CAR is composed of three basic elements: (1) the extracellular antigen recognition domain, (2)the transmembrane domain and (3) the intracellular signaling domain. The extracellular portion is a single chain antigen recognition receptor composed of heavy and light chains of a monoclonal antibody specific to the tumor surface antigen, allowing for no restrictions of target antigen recognition by major histocompatibility complex (MHC)molecules. The intracellular portion is formed by combining co-stimulatory molecules to the intracellular portion of TCRs[58]. The basic process of CAR-T generation includes: (1) T cell isolation from peripheral blood mononuclear cells using immunoselective beads and activation with anti-CD3 and Il-2, (2) genetic modification of CAR-T,(3) expansion of T cellsin vitro, (4) evaluation ensuring CAR expression and T cell viability, and (5) CAR-T infusion back into the patient[59]. TCR transgenic T cells possess a TCR on the surface consisting of two distinct protein chains; alpha and beta,which bind to the MHC of antigen presenting cells, allowing for a highly specific interaction which is not limited to membrane bound antigens[60,61]. As previously described the selection and validation of target antigens is of utmost importance when designing both TCR-T cells and CAR-T cells that are efficacious and minimize on target/off-tumor side effects[62].
CAR-T immunotherapy
CAR-T cell therapy has been tested both preclinically and clinically when targeting HCC. Below we will discuss findings of completed and ongoing clinical studies that seek to demonstrate safety and efficacy of cellular therapy. Shiet al[63] recently published results from two prospective phase I trials involving GPC-CAR-T cells(NCT02395250 and NCT03146234) in patients with advanced GPC3 positive relapsed or refractory HCC following chemotherapeutic induced lymphodepletion. A total of 13 patients received CAR-T cell infusion, with two partial responses and one patient with sustained stable disease after 44.2 mo. OS rates at 3 years, 1 year, and 6 mo were 10.5%, 42% and 50.3% respectively with median OS duration of 278 d according to the Kaplan-Meier method. Unfortunately, toxic effects were noted with major concern as one patient developed cytokine release syndrome (CRS) leading to death from multiorgan failure[63]. A recently completed, open-label, phase I-II study by Daiet al[64]demonstrated efficacy of CD133-CAR-T cell therapy in patients with biopsy proven HCC (BCLC stage C) not amenable to curative treatment. One patient demonstrated a partial response, while 66.7% of patients had stable disease after infusion with an overall PFS of 6.8 mo and median OS of 12 mo (NCT02541370). Currently an openlabel, single center, phase I-II study is underway investigating CAR-T/TCR-T cell immunotherapy targeting a variety of different malignancies including hepatoma(NCT03638206). A list of currently ongoing clinical trials investigating CAR-T cells for the treatment of HCC is listed in (Table 1).

Table 1 Ongoing clinical trials investigating chimeric antigen receptor-T cell therapy in the treatment of hepatocellular carcinoma according to ClinicalTrials.gov
Improving CAR-T delivery and efficacy
Proven clinical efficacy of CAR-T across a variety of hematological malignancies has led to the investigation of its use in solid tumors. However, treatment of solid tumors poses many challenges to clinical investigators, one of which includes access to the tumor site. Many cases of HCC occur on the background of a fibrosed and cirrhotic liver, and the presence of such fibrotic extracellular matrix (ECM) poses a barrier for CAR-T cell penetration. In order to overcome such a challenge, CAR-T cells coexpressing heparinase, which degrades ECM heparan sulfate proteoglycans were developed. These newly engineered CAR-T cells improved cellular ability to degrade the ECM and displayed antitumor activity, suggesting a feasible strategy for the development of CAR-T cells targeting stroma-rich solid tumors[65]. Similar strategies are being investigated with the use of matrix metalloproteinase 8, which can allow CAR-T cells to overcome physical barriers[66]. Local administration of immunotherapy directly into tumors has shown promising results for organ selective delivery.In a study conducted by Katzet al[67], not only were CAR-T cells detected in biopsies of liver metastasis, but effective CAR-T cellular response was noted within the tumor following deliveryviahepatic artery infusion. Such results have paved light into the investigation of direct tumor inoculationviaa variety of local administration techniques including hepatic artery infusion in a multitude of clinical trials. Novel delivery platforms including nanoparticles, scaffolds and other biomaterials are also being investigated as a safe and effective way to deliver immunotherapy to tumor cells while avoiding off-target adverse effects[68]. Recent findings from the 2020 study conducted by Maet al[69], demonstrated superior targeting and anti-tumor capabilities of CAR-T cell membrane coated nanoparticles bothin vivoandin vitro.
In addition to tumor location being inaccessible, the tumor microenvironment has been found to be detrimental to CAR-T cells in regard to their survival and proliferation. The consumption of glucose by malignant cells renders the surrounding environment hypoxic, acidic, and low in nutrients leading to oxidative stress; leaving glycolytic T cells unable to adequately function, ultimately hindering the immune response[70,71]. In order to help eliminate reactive oxygen species (ROS) accumulation, CAR-T cells co expressing catalase were designed, and were subsequently able to survive and function in such unfavorable environments[72]. However, oxidative stress with release of compounds such as ROS and hydrogen peroxide, not only prevents recruitment and adequate function/persistence of immune cells, it also allows for recruitment of immune suppressor cells that lead to CAR-T cell exhaustion[73]. Strategies to help overcome such exhaustion include the use of ICIs that target PD-1, PD-L1, CTLA-4 in conjunction to CAR-T cells administration[74], and by genetically deleting T-cell PD-1 protein with the use of CRISPR-CAS9 gene editing[75]. There is optimism that these findings coupled with continued advance-ments in biomedical engineering will allow for new delivery and tumor microenvironment altering capabilities that can help amplify immunotherapeutic response in thetreatment of HCC.
Improving CAR-T safety
When utilizing cellular immunotherapy with CAR-T cells, a number of important safety concerns are to be noted including CRS, central nervous system toxicity (CNS)and the “on target-off tumor” effect. CRS is characterized by flu like symptoms including fever, fatigue and headache, which can progress to hypotension and organ dysfunction secondary to uncontrolled systemic inflammatory response associated with elevated serum cytokines; particularly interleukin (IL)-6, IL-10, tumor necrosis factor α (TNF-α) and interferon (IFN)-γ[76]. Symptoms of CNS toxicity can range from headache and dizziness, to memory loss and delirium, and can be found along with CRS or after the resolution of CRS. Although the exact etiology remains unclear at this time, it is speculated that various cytokines may alter the blood brain barrier[77], in conjunction with an increase in protein, white blood cells, IFN-γ, TNF-α, and IL-6 within cerebrospinal fluid[78].
These adverse reactions stem from CAR-T cells recognizing TAAs, which are not only heterogenous amongst tumors, but can also be present in normal tissues,elevating the risk of off target toxicity[71]. Such toxic effects have been reported following administration of anti-ERBB2 CAR-T cells for the treatment of metastatic malignancy, which led to CRS with subsequent respiratory distress and death due to low levels of ectopic ERBB2 in lung epithelium[79]. In order to help overcome such toxicities, a variety of strategies are being investigated. One such strategy includes the controlled removal of CAR-T cells with the use of suicide genes. There has been promise with the use of a drug inducible caspase 9 system (pro-apoptotic molecule that activates downstream pro-apoptotic caspase 3 when chemically induced) leading to apoptosis of CAR-T cells on demand[80] and with a system utilizing a truncated epidermal growth factor receptor, which allows for elimination following administration of a receptor specific antibody[81]. More recently, Amatyaet al[82] developed CAR-T cells with a caspase 9 suicide gene for the treatment of multiple myeloma.Following administration of a dimerizing agent, CAR-T cells underwent apoptosis and were no longer active.
As previously mentioned, identification of a suitable TAA is imperative in the development of efficacious CAR-T cells, however highly specific TAAs are rarely identified, leading to investigation of dual- targeted CAR-T cells. Chenet al[83]developed dual-target CAR-T cells (targeting GPC3 and Asialoglycoprotein receptor 1)for the treatment of HCC. Not only did these cells demonstrate superior anticancer activity coupled with higher cytokine secretion when compared to single target CAR-T cells, but their specificity toward cellular targets may reduce the risk of on target- off tumor toxicity[83]. Recent developments have shown efficacy of a novel, split anti-GPC3 CAR-T, into two components with the use of SpyCatcher (extracellular 116 amino acid sequence linked to the intracellular domain) and SpyTag (13 amino acid peptide linked to single chain variable fragment). Such dual component delivery of CAR-T cells not only suppressed tumor growth, but displayed decreased cytokine release, representing a safer alternative when compared with conventional CAR-T cells[84]. Other perspectives include formation of a split, universal and programmable CAR system that allows for enhancement of specificity, safety and programmability of CAR delivery systems[85].
TCR engineered T cells
TCR engineered T cells are modified T cells that are able to precisely recognize tumor surface antigen peptides and MHC, rendering a response only effective when tumor cells express both antigen epitopes and MHC molecules[57]. TCR engineered T cells specific to NY-ESO-1 have demonstrated significant antitumor effects in the treatment of multiple myeloma[86] and synovial sarcomas[87]. The presence of NY-ESO-1 overexpression in HCC has made it an investigated target when developing engineered T cells in one phase II study (NCT01967823), and two phase I studies (NCT02869217)and (NCT03159585), for which we eagerly await results. In addition, TCR engineered T cells targeting hepatitis B viral antigens in HBV related HCC have been of interest in both preclinical and clinical models[88,89]. Recently in November 2020, Chenet al[90]presented an abstract at the 2020 Society for Immunotherapy of Cancer, demonstrating safety and efficacy of HBV specific TCR T-cells in recurrent HBV related HCC patients post liver transplant (NCT02719782).
There are currently five ongoing trials investigating TCR engineered cells targeting various TAAs in HCC (Table 2). All trials are investigating efficacy in advanced,unresectable HCC, with the exception of (NCT03899415), which is evaluating the safety and clinical benefit of TCR engineered T cells in HBV positive HCC patients post hepatectomy or radiofrequency ablation.

Table 2 Ongoing clinical trials investigating T cell receptor engineered T cells in the treatment of hepatocellular carcinoma according to ClinicalTrials.gov
Cytokine induced killer cells
Cytokine induced killer (CIK) cell therapy is a form of adaptive cell transfer that has been investigated as adjuvant therapy in patients with HCC. CIK cells are isolated from the patient’s peripheral mononuclear cells, at which point they are grownex vivowith the addition of cytokines such as recombinant human IFN-γ, anti-CD3 monoclonal antibody, and recombinant human IL-2 prior to transfusion back into the patient;allowing for recognition and subsequent death of tumor cells[91]. In a multicenter,randomized phase III trial conducted in Korea, 230 patients were assigned to receive adjuvant CIK or no adjuvant therapy (control) following treatment with surgical resection, radiofrequency ablation or percutaneous ethanol injection (NCT00699816).Median RFS was significantly prolonged in the immunotherapy group (44 movs30 mo,P= 0.01), coupled with lower hazard ratios for all cause death (P= 0.08) and cancer-related death (P= 0.02)[92]. A 5-year follow-up study demonstrated continued efficacy of autologous CIK immunotherapy without any repeated injections(NCT01890291). After an average 68.5 mo follow up, RFS was 44.8% in the immunotherapy group and 33.1% in the control group, coupled with a significantly lower risk of all-cause death (hazard ratio 0.33, 95%CI: 0.15-0.76,P= 0.006)[93]. Similar results were demonstrated in a meta-analysis and systemic review conducted by Caiet al[94]examining adjuvant CIK after invasive treatments for HCC. Pooled analysis demonstrated a significant improvement of RFS, PFS and OS in patients receiving autologous CIK immunotherapy. Although many studies have been conducted examining the safety and efficacy of CIK as an adjuvant treatment for HCC with mixed results; research is limited when examining CIK therapy as a sole treatment for unresectable HCC.
TILs
TIL therapy is an immunotherapeutic technique that involves isolation and subsequent cell culture followed by autologous administration of tumor specific T cells present in infiltrated tumors. Success of adoptive cell therapy using TIL is based on the diverse antigenic specificity displayed by TIL cells toward the tumor and the lytic capabilities possessed allowing for eradication of malignancy[95]. TILs play an essential role in cancer progression[96] and even as a predictive biomarker of response to neoadjuvant chemotherapy in a variety of malignancies[97]. After the recognition of tumor associated antigens[98], various types of TILs infiltrate to the tumor site; including NK cells,NK T cells, mucosal-associated invariant T cells, and gamma delta T cells[99]. CD4+ T helper cells on the other hand further differentiate in the periphery into a variety of subsets (i.e., Th1, Th2, Th9, Th17, Th22, regulatory T cells, and T follicular helper cells)[100]. CD8+ and NK cells contribute to a direct cytotoxic antitumor effect induced by a cascade of activating and inactivating receptors[99].
In a study conducted by Chewet al[101], examining immune gene expression profiles of resected tumor, HCC patient survival was positively correlated to higher expression of inflammatory immune genes. In conjunction, there was an increased presence of NK cells and T cells promoting apoptosis and reducing proliferation in thetumors of patients with longer survival, suggesting that TILs can be used as a specific immunotherapy for treatment of HCC[101]. In a hallmark randomized trial, patients who had undergone curative resection for HCC were assigned to receive adoptive immunotherapyvsno adjuvant therapy. Administration of lymphocyte infusion led to a reduced frequency of recurrence by 18%, significantly longer time to first recurrence(P= 0.008), longer RFS (P= 0.01) and disease- specific survival (P= 0.04) when compared to controls[102]. A phase I trial (NCT01462903) examined the use of autologous TILs in HCC patients post resection. Results demonstrated that 80% of patients remained disease free after 14-mo follow-up, while displaying a favorable side effect profile, further suggesting TIL therapy as a safe treatment method for HCC[103].Currently an active clinical trial is investigating the safety and efficacy of autologous TILs in patients with high-risk recurrent HCC (NCT04538313). Research is limited on the use of TIL immunotherapy for unresectable HCC, and we hope that further studies can be initiated using TILs alone or in combination with other therapies such as chemotherapy or ICIs.
NK cells
NK cells play an active and critical role in the innate and adaptive immune defense against viral infections and hepatocellular malignancy[104], forming as much as 50%of innate immunity cell infiltrate within the liver[105]. Several clinical studies have demonstrated the safety and efficacy of allogenic NK cell adoptive immunotherapy in the treatment of various malignancies[106,107] including HCC[108]. In a study conducted by Linet al[108], patients were enrolled to receive cryoablation alonevsallogenic NK cell therapy for the treatment of unresectable HCC. Results demonstrated synergistic effects of combination therapy leading to enhanced immune function, reduction in AFP, and improved quality of life in addition to an increased median PFS (9.1 movs7.6 mo,P= 0.01), higher response rate (60%vs46.1%,P< 0.05)and DCR (85.7%vs69.2%,P< 0.01) when compared to cryoablation alone. Similar results were demonstrated in a study conducted by Alnaggaret al[109], which investigated allogenic NK cell immunotherapy in combination with irreversible electroporation for Stage IV unresectable HCC. Efficacy of treatment was synergistic, with statistically significant lower AFP levels at 1 and 3 mo after treatment (P< 0.01),coupled with a higher median OS (10.1 movs8.9 mo,P= 0.0078) when comparing combo therapiesvselectroporation alone. Currently a phase I/II study investigating allogenic NK cell therapy in patients with advanced HCC (NCT04162158) is underway, as well as a phase II/III study examining the effects of autologous NK therapy when coupled with transcatheter arterial chemoembolization (TACE) for the treatment of advanced HCC (NCT04011033). Combination therapy of “off the shelf”FT500 NK cells with ICIs is also being investigated in subjects with advanced solid tumors including HCC (NCT03841110).
The advent of genetic modification techniques has led to the use of CAR technology to develop CAR-NK cells to improve specificity and efficacy of NK cell cytotoxi-city[110]. Yuet al[111] developed a GPC3-specific NK cell for the treatment of HCC, which demonstratedin vitrocytotoxicity and cytokine production in addition to potent antitumor activities in HCC xenografts. Similar treatment benefits were noted with the development of c-MET specific CAR-NK cells, which demonstrated specific cytotoxicity against malignant hepatic cellsin vitro[112]. While there are many ongoing clinical trials investigating CAR-NK immunotherapy for the treatment of hematological malignancies; investigation of treatment efficacy in solid tumors remains scarce.
DC-CIK cells
DC are antigen presenting cells that bridge the gap between innate and adaptive immunity, allowing for activation of naïve T cells that promote tumor-specific T cell immune response and adaptive immunity[113]. The use ofin vitrogenerated DC combined with CIK cells has shown to be an effective and promising immunotherapy technique when used alone or in combination with other treatment options for a variety of malignancies[114]. In a study conducted by Zhouet al[115], advanced HCC patients were assigned to receive sorafenib alonevsa combination of sorafenib and DC-CIK immunotherapy. Results not only demonstrated a significant reduction in AFP levels when using combination therapy, but a significant increase in clinical benefit rate (41.9%vs88.6%,P< 0.05) and prolonged median survival time (13.8 mvs18.6 m,P< 0.05) while maintaining safety. Examination of combined therapy of TACE with DC-CIK therapyvsTACE alone has shown statistically prolonged OS time in HCC patients with HBV[116]. A meta-analysis of 22 studies, conducted in 2019 by Caoet al[117], has shown a prolonged survival and reduced recurrence rate of HCC when combining conventional clinical treatment and immunotherapy with DC and/or CIKs.There are currently studies recruiting participants for treatment of various solid tumors (including HCC) with DC-CIK combination immunotherapy (NCT04214717,NCT04476641, NCT03190811).
HCC vaccines
Current advancements in medicine and immunobiology have demonstrated promising treatment strategies of cancer vaccines and oncolytic immunotherapy in patients with advanced stage cancer, leading to a variety of studies under clinical investigation[118]. Modalities include DC vaccinations, vaccines that target the antigens on tumor cells which in return activate cellular and humoral immunity causing a phagocytic activity towards the tumor cells, and oncolytic viruses that can attack and destroy tumor cells. These vaccines have both prophylactic and therapeutic aspects that can aid in the treatment of advanced cases of HCC. An up-to-date list of cancer vaccines and oncolytic virus therapies under current clinical investigation is provided (Table 3).

Table 3 Ongoing clinical trials investigating cancer vaccines and oncolytic viruses in the treatment of hepatocellular carcinoma according to ClinicalTrials.gov
Antigen peptide vaccines
Targeting these unique antigens can contribute to a significant approach in the development of vaccines in cases of HCC. Foremost antigens include AFP, GPC3, NYESO-1, hTERT, and hepatocellular and melanoma antigen gene-A (MAGE-A) as previously mentioned[119]. GPC3 peptide, a heparan sulfate glycoprotein and member of the GPC proteoglycan group, functions through attaching to the cell membrane by a glycophosphatidylinositol anchor, further regulating several growth factors through the Wnts, hedgehog, and the BMP signaling pathways[120]. This peptide can be an ideal target for HCC vaccine development, as GPC3 is detected in the vast majority of HCC cases[121]. In a phase I trial conducted on 33 patients to ensure the safety of the GPC3-derived peptide vaccine for advanced HCC, results indicated a well-tolerated vaccine with significant immune response, and an improvement in the median OS rate, 12.2 mo (95%CI: 6.5-18.0) in patients with high GPC3-specific cytotoxic T-lymphocytes frequencies, as compared with 8.5 mo (95%CI: 3.7-13.1) in those with low GPC3-specific cytotoxic lymphocyte frequencies (P= 0.033)[122].However, it was not determined if these tumor-infiltrating lymphocytes detected after vaccination were GPC3 peptide-specific cytotoxic lymphocytes, prompting the initiation of a phase II trial (UMIN000005093) in patients with advanced HCC having failed sorafenib, which demonstrated induction of GPC3 peptide specific cytotoxic lymphocytes capable of infiltrating tumors[123].
DC vaccines
DCs have a potent effect on the T cell responses in HCC and other malignancies by acting as antigen presenting cells towards cytotoxic T lymphocytes[124]. Prior to administration of these vaccines to subjects, allogenic DCs are loaded with tumor antigensex vivo, and then stimulated with cytokines such as granulocyte-macrophage colony-stimulating factor for further expansion[125]. In a recent 2016 study, DC vaccines loaded with autologous tumor cell lysate (Hepa1-6 cells) were studied using an orthotopic murine model of HCC. Treatment using this combination not only inhibited progression of murine HCC, but results were promising with a 90% survival rate compared to survival rate lower than 5% in untreated mice, suggesting alteration of the immunosuppressive tumor microenvironment as measured by lymphocyte andcytokine analysis[126]. Although DCs seem to be an attractive treatment modality,further research is required to establish betterin vitrohandling of DCs, better methods of cellular delivery as well as further adaptation to the in-vivo environment following cellular administration.
Oncolytic virus therapy
The use of exogenously administered viruses has paved way as a new and promising modality of targeting cancer cells and promoting neoplastic destruction following replication and subsequent lysis of tumor cells. Such actions allow for the release of antigens after lysis, which triggers antitumor activity[29]. One such virus is Pexa-Vec(pexastimogene devacirepvec, JX-594), a modified pox virus expressing granulocytemacrophage stimulating factor that activates both innate and adaptive immune responses, remaining as the leading oncolytic virus of interest when combating HCC[127,128]. A randomized phase II trial conducted in patients with advanced HCC,demonstrated dose-related significant improvement in OS at high doses (14.1 mo)compared to low-dose treatment (6.7 mo), coupled with tumor regression involving one complete response[129]. Current interest has sparked trials with combination of common therapies. We eagerly await the results of Pexa-Vec with nivolumab(NCT03071094), and Pexa-Vec with sorafenib (PHOCUS; NCT02562755) for treatment of patients with advanced HCC.
CONCLUSION
Treatment of HCC has made significant strides over the past decade since the approval of sorafenib as the first line, standard of care, molecular based treatment in 2007. More recently over the past few years four novel drugs: lenvatinib, ramucirumab, regorafenib, cabozantinib, have proven to be both safe and efficacious leading to approval for clinical use as an alternative or in addition to sorafenib. Clinical trials investigating the check point inhibitors atezolizumab, ipilimumab, nivolumab, and pembrolizumab have proven efficacy and identified new treatment modalities for HCC. As discussed in the paper adoptive immunotherapy including CAR-T cells, TCR engineered T cells,CIK cells, TIL cells, NK cells, DCs, and various vaccines have proven to be a promising therapeutic strategy for the treatment of HCC, however there are still many obstacles that need to be overcome prior to clinical application. Such challenges include identification of the ideal targeted antigen, overcoming the heterogenous and immunosuppressive environment of HCC, ensuring adequate delivery and persistence of immune cells, avoiding toxicity, and continued development of safe and cost-effective measures for cellular based treatment production and subsequent delivery to patients. The differences displayed between hepatic tumors amongst individuals across various stages of liver disease can possibly explain the difference in both clinical effects and adverse outcomes of immunotherapies studied. Therefore, we believe that the future of HCC treatment lies in the prospect of combined treatment modalities to exhibit synergistic effects, which have already entered various clinical trials as described within this paper. While most completed and ongoing studies focus on individuals with adequate underlying hepatic function (Child-Pugh Class A), it is imperative to expand studies to other patient subgroups including those with early-stage disease and those undergoing palliative treatment. We believe that continued investigation over the coming years will overcome current barriers and lead to the development of novel and multifactorial immunotherapeutic strategies allowing for great advances in the treatment of HCC.
 World Journal of Clinical Oncology2021年5期
World Journal of Clinical Oncology2021年5期
- World Journal of Clinical Oncology的其它文章
- COVID-19: Where is the treatment?
- Immune response evaluation criteria in solid tumors for assessment of atypical responses after immunotherapy
- Hepatic Langerhans cell histiocytosis: A review
- Thymoquinone anticancer activity is enhanced when combined with royal jelly in human breast cancer
- Prognostic role of sarcopenia in metastatic colorectal cancer patients during first-line chemotherapy: A retrospective study
- Reduction of muscle contraction and pain in electroporation-based treatments: An overview
