Long-term complete response in metastatic poorly-differentiated neuroendocrine rectal carcinoma with a multimodal approach: A case report
Silvia Della Torre, Germana de Nucci, Pietro Maria Lombardi, Samuele Grandi, Gianpiero Manes, Roberto Bollina
Silvia Della Torre, Roberto Bollina, Oncology Unit, ASST Rhodense, Rho 20017, Italy
Germana de Nucci, Department of Gastroenterology, Garbagnate Milanese Hospital, ASST Rhodense, Garbagnate Milanese 20024, Italy
Pietro Maria Lombardi, Minimally Invasive Surgery Division, Niguarda Hospital, Milan 20110,Italy
Samuele Grandi, Robotic and Emergency Surgery, General Surgery Division, Manzoni Hospital, Lecco 23900, Italy
Gianpiero Manes, Gastroenterology Unit, ASST Rhodense-Garbagnate Milanese, Garbagnate Milanese 20054, Italy
Abstract BACKGROUND Neuroendocrine gastrointestinal tumors (NETs) are rare and have different natural behaviors. Surgery is the gold standard treatment for local disease while radiotherapy has been demonstrated to be ineffective. Poorly differentiated neuroendocrine carcinomas (NECs) represent only 5%-10% of digestive NETS.Due to aggressive growth and rapid metastatic diffusion, early diagnosis and a multidisciplinary approach are mandatory. The role of surgery and radiotherapy in this setting is still debated, and chemotherapy remains the treatment of choice.CASE SUMMARY A 42-year-old male with an ulcerated bleeding rectal lesion was diagnosed with a NEC G3 (Ki67 index > 90%) on May 2015 and initially treated with 3 cycles of first-line chemotherapy, but showed early local progressive disease at 3 mo and underwent sphincter-sparing open anterior low rectal resection. In September 2015, the first post-surgery total-body computed tomography (CT) scan showed an early pelvic disease relapse. Therefore, systemic chemotherapy with FOLFIRI was started and the patient obtained only a partial response. This was followed by pelvic radiotherapy (50 Gy). On April 2016, a CT scan and 18F-fluorodeoxyglucose positron emission tomography imaging showed a complete response (CR)of the pelvic lesion, but pathological abdominal inter-aortocaval lymph nodes were observed. Due to disease progression of abdominal malignant nodes, the patient received radiotherapy at 45 Gy, and finally obtained a CR. As of January 2021, the patient has no symptoms of relapse and no late toxicity after chemotherapy or radiotherapy.CONCLUSION This case demonstrates how a multimodal approach can be successful in obtaining long-term CR in metastatic sites in patients with high grade digestive NECs.
Key Words: Neuroendocrine tumor; Multimodal therapy; Rectal carcinoma; Surgery;Radiotherapy; Case report
INTRODUCTION
Neuroendocrine gastrointestinal tumors (NETs) are rare and have different natural behaviors. Prognostic factors are tumor differentiation, Ki-67 index and the presence of distant metastases. Most of these tumors are well differentiated NETs[1]; even in the presence of metastasis their prognosis is good with a 5-year overall survival (OS) of 60%-90%. Surgery is the gold standard treatment for local disease and often in metastatic cases, while radiotherapy has been demonstrated to be ineffective[2]. Poorly differentiated neuroendocrine carcinomas (NECs) represent only 5%-10% of digestive NETs and among these rectal NECs account for less than 1% of colorectal malignancies. Relative survival at 5 years is 16.3% overall and 57.4%, 56.4%, 26.3%, and 3.0%for stages I, II, III, and IV cancer[3]. Due to aggressive growth and rapid metastatic diffusion, early diagnosis and a multidisciplinary approach are mandatory. The role of surgery and radiotherapy is still debated, and chemotherapy is the main treatment choice[4]. Based on these data, long-term survivors are rarely described in the literature in the metastatic setting. Here we report a patient with metastatic rectal NEC who maintained a complete response (CR) after 5 years using a different treatment approach.
CASE PRESENTATION
Chief complaints
On May 2015, a 42-year-old male attended our Emergency Department due to acute rectal bleeding.
History of present illness
An urgent colonoscopy showed the presence of an ulcerated lesion 12 cm distant from the anal verge (Figure 1). Endoscopic histological sampling revealed a NEC G3 (Ki67 index > 90%).

Figure 1 Endoscopic view of rectal neuroendocrine carcinoma.
History of past illness
He had no previous health problems, only an allergy to nickel.
Personal and family history
No familial history of gastrointestinal disease or tumors.
Physical examination
On presentation, his vital signs were temperature of 36.5°C, pulse rate of 115 bpm,respiratory rate of 17 breaths/min, blood pressure of 110/60 mmHg, and oxygen saturation of 95%. On general physical examination he looked pale. Abdominal examination revealed a non-distended abdomen. Cardiovascular, pulmonary and neurological examinations were unremarkable.
Laboratory examinations
Complete blood count analysis re vealed a huge decrease in hemoglobin level (9.8 mg/mL) and decreased iron and ferritin levels (20 μg/mL and 4 μg/mL, respectively).
Imaging examinations
Magnetic resonance imaging (MRI), computed tomography (CT) scan and 18Ffluorodeoxyglucose positron emission tomography/CT (18F-FDG PET/CT) scan confirmed rectal localization with loco-regional lymph node involvement and the absence of metastatic disease. After 3 cycles of first-line chemotherapy with cisplatinum (CDDP 75 mg/m2on day 1, every 3 wk) and etoposide (VP16 100 mg/m2on days 1-3, every 3 wk), local progressive disease was shown by MRI and colonoscopy.Local symptoms rapidly worsened, with pain and bleeding.
MULTIDISCIPLINARY EXPERT CONSULTATION
After a multidisciplinary evaluation, surgery was recommended.
FINAL DIAGNOSIS
The histopathology report confirmed small-cell poorly-differentiated NEC pT3N1(6/14), G3, Ki67 98%, with negative surgical margins.
TREATMENT
In August 2015, the patient underwent sphincter-sparing open anterior low rectal resection, and fashioning of a colonic terminal stoma.
OUTCOME AND FOLLOW-UP
In September 2015, the first post-surgery total-body CT scan showed early disease relapse with a 85 mm pelvic lesion (Figure 2), without any other disease on 18F-FDG PET/CT. Thus, systemic chemotherapy with FOLFIRI (irinotecan 180 mg/m2on day 1,followed by folinic acid 400 mg/m2, a 5-FU bolus of 400 mg/m2and 5-FU 1200 mg/m2in a 44-h infusion days (1-2 cycles every 14 d), was administered, and a partial response (PR) was obtained after 12 cycles. This was followed by pelvic radiotherapy(50 Gy). On April 2016, CT scan and 18F-FDG PET/CT imaging showed CR of the pelvic lesion, but pathological abdominal inter-aortocaval lymph nodes (Figure 3 and 4). Due to early progression after systemic treatment of abdominal malignant nodes,the patient received radiotherapy at 45 Gy and obtained a CR. He was followed-up with CT scan and 18F-FDG PET/CT every 6 mo. At the last follow-up in January 2021 both examinations confirmed CR in the pelvic and metastatic disease (Figure 5). He had no symptoms and no late toxicity after chemotherapy or radiotherapy.
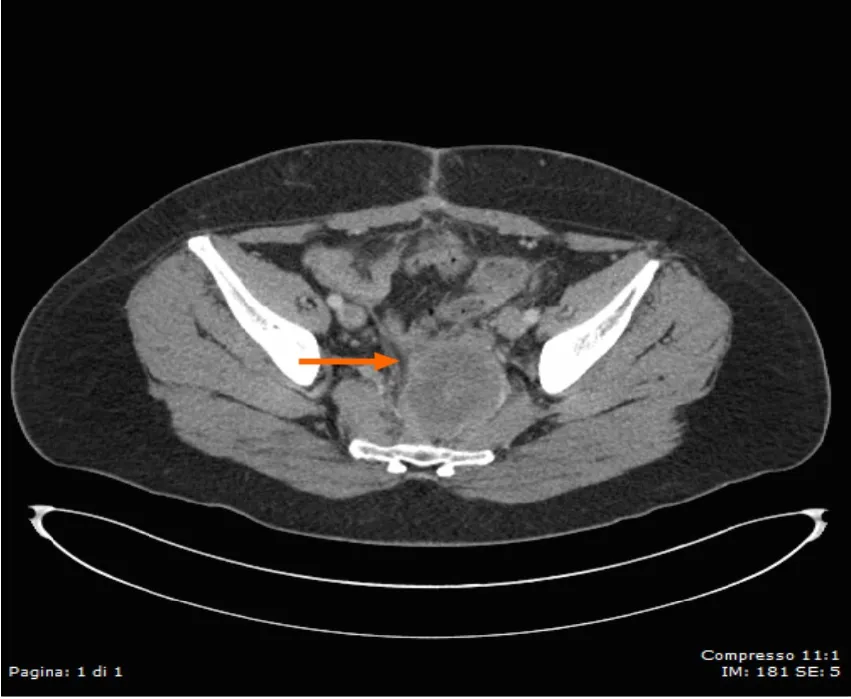
Figure 2 Computed tomography scan view of rectal neuroendocrine carcinoma.

Figure 3 Computed tomography image of rectal lesion downstaging after chemotherapy.

Figure 4 Positron emission tomography/computed tomography images of periaortic lymph nodes. A: Positron emission tomography image; B:Computed tomography image.

Figure 5 Positron emission tomography/computed tomography images showing complete response after radiotherapy. A: Positron emission tomography image; B: Computed tomography image.
DISCUSSION
Rectal NECs are rare entities and there is no consensus on their treatment especially local disease[5]. As there are no guidelines based on prospective studies, oncologists normally use modalities extrapolated from colonic adenocarcinomas or small-cell lung cancer or based on retrospective analysis[6]. The efficacy of systemic chemotherapy for treating digestive metastatic NEC has been largely demonstrated and the role of radiation therapy (RT) and/or surgery is still debated, both in the early stage and metastatic disease[7]. Our case highlights several issues related to the possible clinical treatment of rectal NECs, especially how to treat local primary tumors in patients without metastatic disease. Some retrospective studies agree that there are no differences between surgery and chemoradiotherapy in terms of progression-free survival and OS in local rectal NECs, with disease control in approximately 93% of patients treated exclusively with chemoradiotherapy[8]. These results and the knowledge of high risk of metastatic dissemination for NECs suggest that surgery is not indicated. Moreover, if resection is performed, it has been demonstrated that neoadjuvant, pre-surgery or adjuvant chemotherapy administration is associated with improved rates of survival[9]. As in our case, probably resection is justified in the case of symptomatic or relapse disease.
In the metastatic setting, the gold standard first-line treatment is the combination of platinum and etoposide[10]. Even if there is a high response rate (60%) with this schedule, median OS is poor, ranging from 10 mo to 15 mo[11]. The role of second-line treatment is debated. Some schedules have been tested, which have also included irinotecan. The use of this drug is suggested due to its efficacy demonstrated in both small-cell lung cancer and in colorectal cancer in several studies[12]. After surgery, to treat local early disease relapse we used second-line chemotherapy with FOLFIRI, as the efficacy of FOLFIRI has already been demonstrated in a French study of 39 patients who failed etoposide and platinum combination[13-15]. After obtaining a PR with systemic treatment, pelvic RT was performed, with a long-term local CR. Two months after the end of second-line chemotherapy, metastatic disease was identified in intraaortocaval lymph nodes, which showed no response to systemic treatment. The efficacy of radiotherapy in metastatic patients with NECs has been proved in bone and brain metastasis, but there are no data about its use in other metastatic sites[16,17]. An anecdotal approach with radiosurgery was applied with success in one case of visceral metastasis from rectal MANEC (Mixed Adenoneuroendocrine Carcinoma). Considering the good previous response to radiotherapy, the limited prospects of therapy and the site of oligo-metastasis we decided to treat the patient with another course of RT and obtained a CR.
CONCLUSION
Our case demonstrates how a multimodal approach and continuous follow-up restaging can be successful in obtaining a long-term CR in local and metastatic sites;thus, improving 5-year survival in patients with high grade digestive NEC as confirmed by the last total body CT scan in January 2021 in our patient. Therefore,based on our experience, chemotherapy, RT and surgery should be considered together in the management of rectal NEC even in presence of systemic spread. The treatment for each patient, in the absence of prospective studies and considering the rarity of the disease, need to be accurately tailored.
 World Journal of Clinical Oncology2021年6期
World Journal of Clinical Oncology2021年6期
- World Journal of Clinical Oncology的其它文章
- Phytochemically rich dietary components and the risk of colorectal cancer: A systematic review and meta-analysis of observational studies
- Impact of community-based exercise program participation on aerobic capacity in women with and without breast cancer
- Chemotherapy-induced neurotoxicity in the treatment of gynecological cancers: State of art and an innovative approach for prevention
- Imaging diagnosis of bronchogenic carcinoma (the forgotten disease) during times of COVID-19 pandemic: Current and future perspectives
- Review of 10 years of research on breast cancer patients: Focus on indoleamine 2,3-dioxygenase
- Breast cancer: Muscarinic receptors as new targets for tumor therapy
