Chemotherapy-induced neurotoxicity in the treatment of gynecological cancers: State of art and an innovative approach for prevention
Ester Oneda, Chiara Abeni, Laura Zanotti, Elisabetta Zaina, Sara Bighè, Alberto Zaniboni
Ester Oneda, Chiara Abeni, Laura Zanotti, Elisabetta Zaina, Sara Bighè, Alberto Zaniboni,Department of Clinical Oncology, Fondazione Poliambulanza, Brescia 25124, Italy
Abstract Chemotherapy-induced peripheral neuropathy (CIPN) is a common side effect that occurs in 20% of ovarian cancer patients treated with the combination of carboplatin/paclitaxel (CP). This toxicity is directly correlated with the dose of paclitaxel administered. Several studies have investigated whether different formulations of taxane can induce this side effect at a lower rate, but, unfortunately, no significant improvement was obtained. CIPN can be disabling in the daily lives of patients and can cause dose reduction or early termination of the treatment. Neuropathy can last for months and even years after its onset.Moreover, patients responsive to CP treatment are candidates for a reintroduction of the same drugs when disease relapse occurs, and residual neuropathy can affect the continuation of treatment. There are no approved drugs that mitigate or prevent the onset of CIPN. In this review, we summarize the evidence regarding the incidence of CIPN with different taxane formulations, regimen schedules and prevention systems. In particular, the Hilotherm® Chemo care device is a regional cooling system that lowers the temperature of the hands and feet to reduce the flow of chemotherapy into the capillaries. We used hilotherapy during chemotherapy infusion to prevent the onset of CIPN. Updated data from 44 ovarian cancer patients treated with 6 cycle of CP show that hilotherapy was well tolerated; only two patients (4.5%) stopped hilotherapy because of cold intolerance,and only one patient (2.2%) experienced grade ≥ 2 CIPN.
Key Words: Peripheral neuropathy; Ovarian cancer; Paclitaxel; Chemotherapy-induced peripheral neuropathy prevention; Hilotherapy
INTRODUCTION
Carboplatin/paclitaxel (CP) is the chemotherapy of choice for ovarian cancer, in neo/adjuvant, first-line and in platinum-sensitive recurrence, and moreover, in advance stage a reintroduction of paclitaxel (PTX) monotherapy can be considered[1].A significant proportion of recurring patients, with a platinum-free interval longer than 6-12 mo, are classified as platinum-sensitive and are candidates for retreatment with the same drugs used in first-line therapy[2]. Chemotherapy-induced peripheral neuropathy (CIPN) is one of the most life altering chemotherapy side effects[3,4] and it is frequently related to taxane treatment. The prevalence of CIPN ranges from 11% to over 87%[5]. In an online survey, 78% of 1360 women with ovarian cancer experienced CIPN 2.3 years after completing chemotherapy[6]. CIPN leads to peripheral nerve dysfunction or damage of varying intensity, duration and permanence. Symptoms range from acute transient paraesthesia or chronic pain to permanent peripheral nerve damage[4]. CIPN can occurs days after chemotherapy and gradually progresses to cumulative doses. Symptoms typically present as a “glove and stocking” neuropathy,with tingling, loss of dexterity in the fingers, hypoesthesia of the feet, and paraesthesia in the limbs. In addition, skin burns, electric shocks, as well as altered perception of pain to touch or heat may be felt[7-10]. In the worst case, sensory perception can be completely lost. CIPN can also manifest with motor symptoms with distal weakness,gait and balance disturbances, and impaired movements. Daily physical functioning can be impaired such as firmly grasping objects, unfastening jacket buttons, climbing steps or driving, it affects patient’s the quality of life (QoL)[11,12]. Health-related QoL can be impaired[6,11,13] whit psychological consequences[14] such as major depression[15].
Due to this adverse event, treatment must unfortunately be interrupted or continued at a reduced dose, limiting the effectiveness of chemotherapy. To date, none of the numerous drugs tested to prevent or relieve the symptoms of CIPN has obtained evidence of efficacy. Antidepressants (such as nortriptyline), duloxetine,gabapentin, baclofen-containing gel, amitriptyline, ketamine, lidocaine, tramadol,tapentadol, buprenorphine, and lithium were ineffective[16-25]. These agents have a record of efficacy for other common neuropathic pain conditions, but CIPN has a different pathological origin. The American Society of Clinical Oncology (ASCO) does not recommend any agent for the prevention of CIPN[16]. A number of nonpharmacologic interventions, such as acupuncture, limb hypothermia, surgical glove (SG)compression and electrocutaneous nerve stimulation, have also been investigated.However, the paucity of randomized controlled trial evidence prohibited the inclusion of those studies in this systematic review[16].
Reducing the penetration of chemotherapeutic agents into the capillaries of hands and feet and lowering the temperature of the patient’s extremities can be a way to slow blood circulation and cell metabolism in order to prevent the onset of CIPN. In fact,the tissue metabolic rate can be reduced by 50% dropping the tissue temperature by up to 10 °C. Hilotherapy is an effective method to constantly cool the temperature of the hands and feet during treatment and prevents the development of CIPN and polyneuropathy, giving patients a better QoL. In this review, we will discuss the incidence of CIPN in gynecologic cancer patients, the clinical features related to the treatment and the way to minimize or to prevent its onset.
TAXANE-RELATED CIPN
Taxane-induced CIPN is predominantly sensory (SPN) and rarely presents with motor and autonomic changes[4]. Symptoms may arise early and even after the first administration, they are dose dependent, but tend to improve after discontinuation of treatment. However, the onset and severity are highly variable from individual to individual; no anticipatory signal can suggest a dose reduction, and there are no indications of a de-escalation of therapy to mitigate the symptoms once they arise.Furthermore, CIPN even after the end of chemotherapy can persist for months or years afterwards and in rare cases be permanent[9]. The only certain risk factor is the dose administered, with increases in risk proportional to the cumulative dose[4]. Pignataet al[26] found that approximately three fourths of patients treated with CP experienced peripheral neuropathy, and 7% had ≥ grade 3 CIPN. Residual neurotoxicity occurs frequently in patients after completion of CP, with a long-lasting pattern of recovery and 14% of patients still suffer residual neuropathy 1 year after treatment[27]. Such toxicity still persists in a significant proportion of patients who experience relapse and therefore, affects second-line treatment choice.
The Gynecologic Oncology Group (GOG) reported that approximately 20% of ovarian cancer, patients treated with the combination of carboplatin and PTX at 175 mg/mq every 3 wk in first-line therapy experienced grade 2 or higher neuropathy,and this percentage was increased among older patients[4]. Considering a similar total dose, the MITO-7 study showed that in patients with advanced ovarian cancer the regimen with carboplatin area under the curve (AUC) 2 mg/mL per min plus weekly PTX at 60 mg/mq was less neurotoxic than carboplatin AUC 6 mg/mL per min plus PTX at 175 mg/mq every 3 wk (grade 2 or higher neuropathy of 6%vs17%, respectively). However, despite the better toxicity profile and the incremented QoL, the weekly regimen did not prolong progression free-survival (PFS)[28]. The Japanese Gynecologic Oncology Group (JGOG) randomized patients to receive carboplatin AUC 6 mg/mL per min every 3 wk plus dose dense PTX at 80 mg/mq (on days 1, 8,15) or plus PTX at 180 mg/mq every 3 wk. The study showed that the 7% of patients treated with the dose-dense scheme had grade 3 or higher SPN and 5% had grade 3 or higher motor peripheral neuropathy (MPN), while 6% of patients treated with the standard regimen reported grade 3 or higher SPN and 4% grade 3 or higher MPN[29].Despite a better median PFS benefit of 28.0 movs17.2 mo and an overall survival benefit at 3 years of 72.1%vs65.1% in the dose-dense treatment group compared to the conventional treatment group, more patients in the dose-dense group discontinued the treatment due to hematologic toxicity[29]. In contrast, in the JGOG-3016[30] and GOG-0262[31] studies, patients in groups 2 and 3 of ICON8[32] received up to 80 mg/mq of PTX per week and showed worse SPN in the weekly treatment group than in the every 3-wk treatment group. These findings suggest that SNP could be caused by cumulative PTX exposure rather than its dosing intensity[32]. The Scottish Ginecological Cancer Trials Group suggested that docetaxel could be less neurotoxic than PTX, and they reported a rate of 11% grade 2 or higher SPN with carboplatin AUC 5 mg/mL per min plus docetaxel 75 mg/mqvsa rate of 30% with carboplatin AUC 5 mg/mL plus PTX 175 mg/mq every three weeks in first-line ovarian cancer; however, this research did not demonstrate any survival benefit[33]. Unfortunately, platinum-sensitive patients who relapse are candidates for retreatment with CP, so residual peripheral neuropathy can be a limiting factor. However, studies that have evaluated the incidence of neuropathy in this setting report a 20% incidence of CIPN > 2 grade[2,34]. This proportion is lower than expected, which is a bias that is due to poor recruitment of patients with residual CIPN[2].
Symptom improvement or resolution after 3-6 mo at the end of standard treatment can be achieved by most of patient; however, in some cases, symptoms can last years,with a probability of 15% of patients still having neuropathy 6 mo after completion of chemotherapy and an 11% probability of still experiencing neuropathy at 2 years after completion of chemotherapy[4]. In the secondary analyses of the ROGY care trial among ovarian cancer patients, the course of SPN among chemotherapy-treated patients remained stable over the course of 2 years, while MPN symptoms declined at 12 mo. Furthermore, at 2 years, 13% still reported high levels of SPN[3]. Similar findings were seen in the previous PROFILE study with a prevalence of 6%-9% of SPN and 14% of MPN at 2-12 years after treatment, and a decreased in CIPN symptoms three years after the end of treatment[6] (Table 1).
MECHANICAL SYSTEMS OF CIPN PREVENTION
Many studies have investigated the potential use of non-invasive approaches to prevent CIPN. The different mechanical systems tested include: acupuncture,scrambler therapy, hypothermia and compression therapy which aim to reduce damage to the peripheral nerves of the extremities. Acupuncture technique showed grade 3 symptom regression or stability in patients experiencing grade > 2 CIPN with weekly PTX for breast cancer[35]. Transcutaneous electrical nerve stimulation(scrambler therapy) was observed to relieve CIPN symptoms in several trials[36-41](53% reduction in pain, 44% reduction in tingling and 37% reduction in numbness[37]), and these effects were maintained for 3 mo of follow-up[40]. The use of SG compression therapy was investigated by Tsuyukiet al[42] the reduction of microvascular flow to the hands during PTX administration allows to reduce the incidence of grade 2 or higher CIPN. The incidence of grade 2 or higher sensory CIPN, according to Common Terminology Criteria for Adverse Events (CTCAE), with SG compression therapy was low at 13.8%vsthe incidence in the historical control group (44.1%)[42].
Cold temperature is known to reduce tissue microvascular perfusion, “therapeutic regional hypothermia” or “cryotherapy” using different limb cooling modalities (e.g.,direct application of ice or frozen gloves) and has been use in attempt to prevent chemotherapy-induced nail and skin toxicity, but the mechanism of the large cooling gradients of these modalities permits only intermittent coolant application and are limited by substantial intolerance and sometimes frostbite[43,44]. Rosenbaeket al[45]demonstrated that cryotherapy associated with PTX treatment in the adjuvant treatment of breast cancer reduces the risk of dose-limiting CIPN, and increases the number of patients receiving the full chemotherapy dose (77% of patients). However,the comparison study between cryotherapy and preventive compression therapy during treatment with nab-PTX showed no benefit for either system[46]. A recent randomized controlled trial that investigated the effect of cryotherapy administered on all four limbs during PTX treatment among early and locally advanced breast cancer patients did not decrease the incidence and severity of sensory symptoms[47]. This study was unable to conclude that cryotherapy prevents sensory neuropathy probably because of the high rates of cryotherapy interruption[47].
HILOTHERAPY A NEW PREVENTIVE APPROACH
The Hilotherm®Chemo care device is a regional cooling system that uses cuffs and piping for the hands and feet through which the coolant flows at a temperature of 10°C. The insulators were fitted on both the hands and feet for 30 min before the start to 60 min after chemotherapy administration. A recent study in Germany evaluated the use of this device in 20 cancer patients treated with taxane-based chemotherapy as a preventative method. No patients developed grade 2 or 3 symptoms of CIPN. Four weeks after their chemotherapy ended, 70% of patients who used hilotherapy had no symptoms at all. The other 30% of patients were found to have grade 1 symptoms.Although cooling from the start of treatment achieved the best outcome, the group of patients (n= 36) who started hilotherapy when CIPN symptoms occurred showed a reduction in severe symptoms of CIPN. The use of hilotherapy was found to be comfortable and safe[48].
OUR PERSONAL EXPERIENCE
In the published small retrospective trial from our center we enrolled 64 patients with breast, gynecologic and pancreatic cancer to wear Hilotherm cuffs and piping on their hands and feet. Fifty-four (84%) of these patients completed all cooling cycles during their taxane-based chemotherapy. Continuous cooling was well tolerated by all patients. No patients had grade > 2 CIPN or had serious or lasting side effects as a result of hilotherapy. The median time to CIPN onset was 77 d for the entire population[49].
The updated data in the subgroup of patients with gynecological cancer treated with the combination of carboplatin AUC 5 mg/mL per min plus PTX at 175 mg/mqevery 3 wk show that 35 of 44 patients (79.5%) completed all the planned cycles of chemotherapy with the cooling system. The severity of PN was evaluated by a nurse using the CTCAE (2017). Statistical analyses were performed using STATA 13.0(StataCorp LP, Collage Station, TX, United States). Only 1 patient (2.2%) had grade ≥ 2 CIPN after 4 cycles of CP and completed the last cycle with carboplatin monotherapy;2 patients (4.5%) stopped hilotherapy due to excessive coldness; 3 patients (6.8%)stopped treatment due to disease progression and 2 patients (4.5%) stopped the treatment due to PTX allergic reaction; 3 patients (6.8%) had PTX reduction/interruption that was due to PTX hematologic toxicity and completed the cycles with carboplatin monotherapy and 3 patients (6.8%) concluded the treatment after 3/4 cycles due to hospitalization for planned surgery. Follow-up data are premature at the time of writing this review. Tables 2-4 show patient characteristics and results.

Table 1 Incidence of chemotherapy-induced peripheral neuropathy
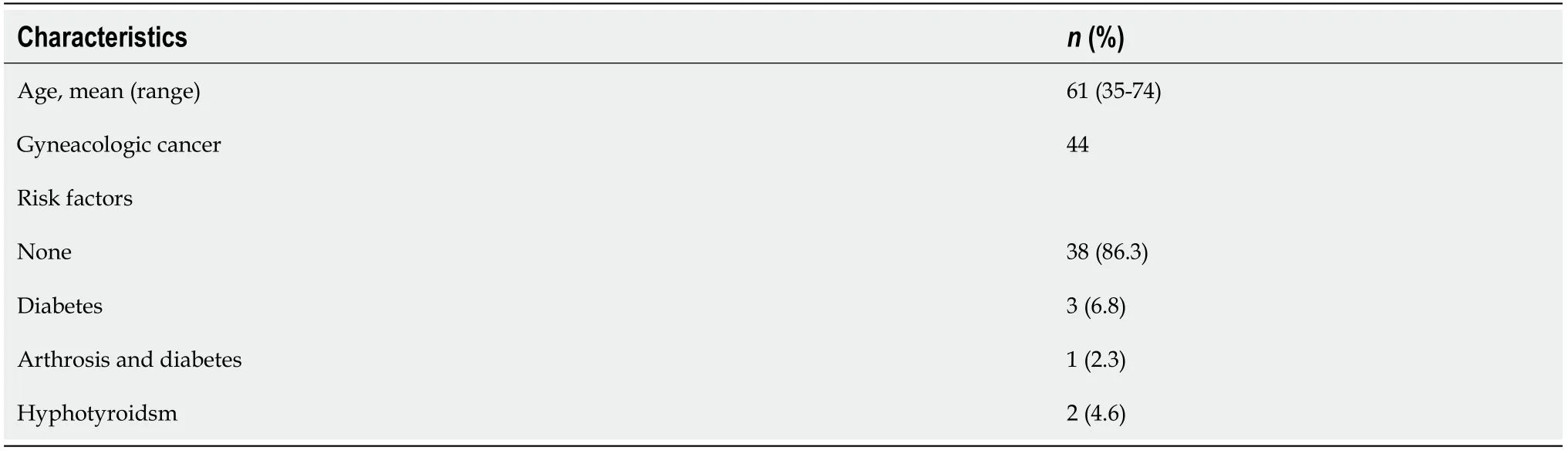
Table 2 Patient characteristics

Table 3 Chemotherapy-induced peripheral neuropathy per cycle, according to Common Terminology Criteria for Adverse Events(version 4.0)

Table 4 Chemotherapy (paclitaxel) dose changes during hilotherapy treatment
DISCUSSION
Neuropathy is an important, dose-limiting, painful, and often irreversible toxicity associated with taxane therapy. Approximately 20% of women treated for ovarian cancer show CIPN, and this toxicity impairs their QoL and can persist for months or even years after the end of treatment. Instead, for recurrent disease the established treatment is a reintroduction of the first-line scheme in sensitive patients, with a with a higher probability of developing toxicity or worsening of pre-existing toxicity with a consequent limitation of the duration of treatment. The only prophylactic therapy for CIPN suggested by the guidelines of the ASCO 2014[16] is duloxetine, but it has limited efficacy in chemotherapy-induced neuropathic pain and has no benefit on paraesthesia and functional disability. Recently, ganglioside monosialic acid has shown promising effects on the prevention of neuropathic symptoms with a lower incidence of grade> 1 on the CTCAE v4.0 scale (14.3%vs100.0%,P< 0.001) both sensory (26.4%vs97.8%,P< 0.001) and motor (20.9%vs81.5%,P< 0.001) in patients with breast cancer treated with PTX[50]. Previous studies suggested positive effects of physical activity on CIPN with a higher CIPN in patients who do not meet recommended activity levels[51,52]. Moderate to vigorous activity was associated with lower CIPN in taxane-treated patients[53]. Patients who followed physical activity guidelines reported a longer time to the onset of CIPN since completing chemotherapy, potentially suggesting adaptation to neuropathic symptoms over time,enabling the return to physical activity[53]. Conveying PTX using lipid-based nanoformulations represents a potential strategy to overcome PTX side effects. In a recentstudy, this formulation was tested on lung tumor cells andin vivoand showed a very low concentration in the dorsal root ganglia, where PTX accumulates and causes damage to the somas of peripheral sensory neurons[54]. This approach could lead to a reduction in the incidence of peripheral neuropathy and be the subject of study in gynecological cancers.
Different mechanical system of CIPN prevention were tested and founded that vasoconstriction and cold reduce drug exposure during chemotherapy infusion[55],but the limits of cooling systems are primarily the cold intolerance and cold-related injuries. The small single-arm trial from our center that investigated the effects of hilotherm cooling system demonstrate to prevent CIPN[49]. The advantages of continuous cooling are a more tolerable and controlled temperature reduction for the duration of chemotherapy instead of ice or frozen gloves. Continuous cooling whit a coolant temperature of 10 °C continued for the duration of chemotherapy and was well tolerated. In the ovarian cancer subgroup only one patient showed CIPN ≥ 2, and only two patients (4.5%) stopped halotherapy for cold intolerance. Published data showed that no patients reported the appearance of CIPN symptom at a follow-up time of 6 mo[49]. We expect to maintain these follow-up results also from the new enrolled patients.
CONCLUSION
The prevalence of CIPN was approximately 68% within the first month following the end of taxane chemotherapy treatment and 30% after 6 mo or more[4]. In a survey of ovarian cancer patients, CIPN symptoms were associated with lower functioning and greater health-related worry[5]. Additionally, a survey covering various cancer types found that patients reporting neurotoxicity had higher symptom burden and stress,and poorer QoL[56]. Reducing the incidence of neuropathy to improve the patient’s QoL and avoiding discontinuation or dose reduction of anticancer treatment is of primary importance. Unfortunately, comprehensive knowledge of the mechanisms leading to CIPN is still lacking and no drug has been approved to prevent or cure it.Hilotherapy has proven to be a safe, well tolerated and effective method of preventing and treating CIPN. To validate the use of hilotherapy as a preventive method a largescale trial and a longer follow up are necessary.
 World Journal of Clinical Oncology2021年6期
World Journal of Clinical Oncology2021年6期
- World Journal of Clinical Oncology的其它文章
- Long-term complete response in metastatic poorly-differentiated neuroendocrine rectal carcinoma with a multimodal approach: A case report
- Phytochemically rich dietary components and the risk of colorectal cancer: A systematic review and meta-analysis of observational studies
- Impact of community-based exercise program participation on aerobic capacity in women with and without breast cancer
- Imaging diagnosis of bronchogenic carcinoma (the forgotten disease) during times of COVID-19 pandemic: Current and future perspectives
- Review of 10 years of research on breast cancer patients: Focus on indoleamine 2,3-dioxygenase
- Breast cancer: Muscarinic receptors as new targets for tumor therapy
