Impact of community-based exercise program participation on aerobic capacity in women with and without breast cancer
Jordan T Lee, Chad W Wagoner, Stephanie A Sullivan, Dean J Amatuli, Kirsten A Nyrop, Erik D Hanson, Lee Stoner, Brian C Jensen, Hyman B Muss, Claudio L Battaglini
Jordan T Lee, Chad W Wagoner, Stephanie A Sullivan, Dean J Amatuli, Erik D Hanson, Lee Stoner,Claudio L Battaglini, Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, United States
Kirsten A Nyrop, Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, United States
Brian C Jensen, Department of Medicine, Division of Cardiology, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, United States
Hyman B Muss, Lineberger Comprehensive Cancer Center, University of North Carolina,Chapel Hill, NC 27599, United States
Abstract BACKGROUND Evidence for exercise as an efficacious strategy to improve aerobic capacity of breast cancer survivors (BCS) has come largely from intervention studies conducted in laboratory settings. There is an increasing need to translate to community-type settings, but the efficacy of those interventions using gold standard evaluation is not well-established.AIM To investigate whether similar improvement in aerobic capacity (maximal oxygen consumption [VO2]) measured with gold standard testing can be achieved through a community-based setting in BCS.METHODS A peak cardiopulmonary exercise test (VO2peak), 6-min walk test (6MWT), and timed up and go test (TUG) were assessed pre- and post-16 wk of progressive intensity aerobic and strength training exercise at a community center.RESULTS The sample consisted of 31 early BCS (< 1 year since treatment completion) and 15 controls (CTLs). Both groups significantly improved VO2peak (+1.2 mL/kg/min; P= 0.030), 6MWT (+35 meters; P < 0.001), and TUG (-0.44 s; P < 0.01) following training. Both groups improved peak cycling power during the cardiopulmonary exercise test with BCS improving by +10 watts more than the CTLs (P = 0.020).Average exercise attendance was 71% (34 of 48 possible days), but compliant days averaged only 60% of total days for aerobic, and < 40% for strength in both groups.CONCLUSION Community-based exercise programs can be an effective strategy to improve aerobic capacity and physical function for early-stage BCS but potentially not to the same extent observed in laboratory-based randomized controlled trials.Further research is needed to explore barriers and facilitators of exercise engagement in community-based centers to maximize training benefits for adults with cancer.
Key Words: Aerobic capacity; Breast cancer; Community-based; Exercise; Physical function
INTRODUCTION
Cardiorespiratory fitness describes the ability to use oxygen to produce energy for physical work and can be quantified as aerobic capacity (maximal oxygen consumption [VO2]; mL O2/kg/min) using the gold standard maximal cardiopulmonary exercise testing (CPET). Breast cancer survivors (BCS) have substantially impaired aerobic capacities[1,2], with a decline in VO2similar to that experienced with a 10 year increase in age, which can be attributed to both cancer treatment-related toxicities and increased sedentary lifestyle habits[3,4]. This impairment places BCS at substantial risk of death from cardiovascular (CV) disease and loss of functional independence[5].Fortunately, exercise is a known promoter of CV health in the general population[6]and is an effective strategy for improving aerobic capacity in BCS during and posttreatment[7-9].
Multiple well-designed and controlled exercise intervention trials have demonstrated the benefits of aerobic and strength training exercise on aerobic capacity and other physical function outcomes, resulting in the development of exercise prescription guidelines for adults with cancer[10]. Guidelines were recently updated in 2019 and recommend at least 30 min of moderate intensity aerobic exercise at least 3 d/wk, and at least 2 d/wk of strength training for people with cancer[11]. Participation in exercise interventions reflecting these guidelines have demonstrated increases in aerobic capacity by 2.3-2.9 mL/kg/min (approximately 10%-15%)[7,9,12].However, these changes in aerobic capacity have been observed primarily from interventions in highly controlled laboratory randomized controlled trials (RCTs), and the efficacy of this “trial-proven” exercise prescription delivered through real-world settings such as community-based centers has not been well-studied[13]. These settings likely differ from laboratory settings because they may be more relaxed environments with the opportunity for increased socialization between participants,and may provide additional flexibility in terms of training modes and session attendance (ATT) than what laboratory-controlled trials may provide or allow,regardless that the intention to improve fitness and quality of life may be the same. Of the limited work available on evaluating outcomes in community-based settings,cardiorespiratory fitness appears to be maintained or improved but has not been evaluated using direct, gold standard exercise testing methods (i.e.maximal CPET)[14-17]. Instead, alternative indicators of functional capacity such as the 6-min walk test(6MWT), and the timed up and go (TUG) test have been used, which may offer improved utility and feasibility in clinical/community-based centers. As exercise is increasingly recommended to survivors, and as interventions transition from highly controlled laboratory based settings to more practical venues like community-based centers, it is important to precisely evaluate whether similar cardiorespiratory fitness benefits can still be achieved to properly support and accommodate a large volume of cancer survivors in need of improving or even maintaining their overall health,physical function, and quality of life through participation in regular exercise[13,18].
Exercise programming for cancer survivors is a well-recognized challenge in exercise oncology[19-21] because survivors frequently require tailored exercise accommodations based on cancer-related treatments and associated side effects.Oncology-trained staff in community-based settings may be uniquely positioned to modify workouts, but these necessary adjustments have the potential to significantly impact exercise engagement[20,22]. Therefore, collecting and reporting exercise efficacy, ATT, and compliance in community-based intervention studies will improve understanding of how patients engage in these settings and how exercise engagement may relate to physical fitness and health outcomes[23-25].
The primary aim of this study was to evaluate the impact of a community-based exercise program on change in aerobic capacity in women with breast cancer measured using the gold standard CPET. A secondary aim was to evaluate if changes in aerobic capacity in the community-based setting differ between women with and without cancer. A third aim evaluated how exercise engagement (ATT and compliance) relates to changes in aerobic capacity. For the primary aim, we hypothesized that aerobic capacity would significantly improve following community-based training. For the second and third aims, we hypothesized that women in both groups would benefit similarly from the community-based protocol and that the observed changes in aerobic capacity would be directly related to training ATT and compliance.
MATERIALS AND METHODS
This study used a parallel-group, pre-post design. Two groups (one BCS, one noncancer control [CTL]) of women were engaged in an identical supervised exercise evaluation and intervention at Get REAL and Heel (GRH), an established, communitybased exercise facility for cancer survivors in Chapel Hill, North Carolina that has offered exercise training reflective of recommended guidelines to cancer survivors for the past 10 years. This study leveraged an associated exercise oncology lab with gold standard testing capacity to evaluate the existing community-based program as it has currently operated. For data collection, two consecutive visits to the Exercise Oncology Research Laboratory of the UNC Department of Exercise and Sport Science occurred prior to (pre-intervention) and immediately following (post-intervention) the 16-wk exercise program. Outcomes evaluated included peak aerobic capacity (VO2peak), the 6MWT, and the TUG test. Patient demographics and cancer-specific clinical data were extracted from the UNC Health Care electronic medical record by the research team.The study (NCT03760536) was approved by the Protocol Review Committee of the UNC Lineberger Comprehensive Cancer Center and the UNC Institutional Review Board. All participants provided written informed consent.
Study participants
Women ≥ 21-years-old diagnosed with early-stage (Stage 0-III) breast cancer and within 1 year of completing primary therapy (surgery, chemotherapy, radiation) were eligible for the BCS arm. Women in the CTL group were age-matched with no history of cancer. Both groups self-reported no more than 2 d of physical activity per week and not meeting recommended physical activity guidelines. Both groups self-reported no cardiovascular, metabolic, or orthopedic limitations, and were cleared by a cardiologist (both groups) and oncologists (BCS only) prior to participating. Participants in the BCS group were recruited from the Medical Oncology clinic at the North Carolina Cancer Hospital, and by word of mouth from local oncologists and cancer centers. Participants in the CTL group were residents from nearby communities and recruitedviaelectronic and paper fliers and word of mouth. The recruitment period was April 2017-2019 for BCS and February to August 2019 for CTL.
Exercise intervention
Both BCS and CTL groups participated in a 16-wk supervised, small-group (approximately 4-8 participants per session) exercise intervention including combination aerobic and strength exercise training 3 d a week for approximately 1-h total per d (48 total days of training opportunity) at the GRH facility. A variety of equipment for training was used and adapted to individual participant fitness and mobility needs,allowing trainers to maximize patient safety and exercise engagement while helping participants strive towards reaching guideline-prescribed levels of activity. Participants could choose treadmills, stationary bikes or ellipticals for aerobic work and body weight, resistance bands, dumbbells, or machine weights for strength training,depending on their abilities and preferences.
The specific exercise prescription for the supervised intervention at the GRH facility is presented in Table 1. In the first 2 wk, all study participants were asked to engage in low intensity aerobic exercise for 10-15 min plus approximately 30 min of light-tomoderate strength training each day at the facility. Participants were encouraged to challenge themselves to safely engage in exercise intensity that elicited the prescribed exertion level (Borg’s Rating of Perceived Exertion[26], RPE) throughout the intervention. RPE was used as a surrogate measure of intensity in this study in place of heart rate monitoring since it has historically been used at GRH because heart rate transmitter signals tended to overlap between participants in the limited training space available. Intensity could be increased under the direction of trained exercise staff by adding grade (treadmill), resistance (cycling), or speed (mph or rpm) for aerobic training, and by progressing from body weight to resistance bands to free weights or machines for resistance training. The exercise training program has been implemented and designed to create a dose-response to help participants safely attain weekly exercise goals reflective of national guidelines[11].
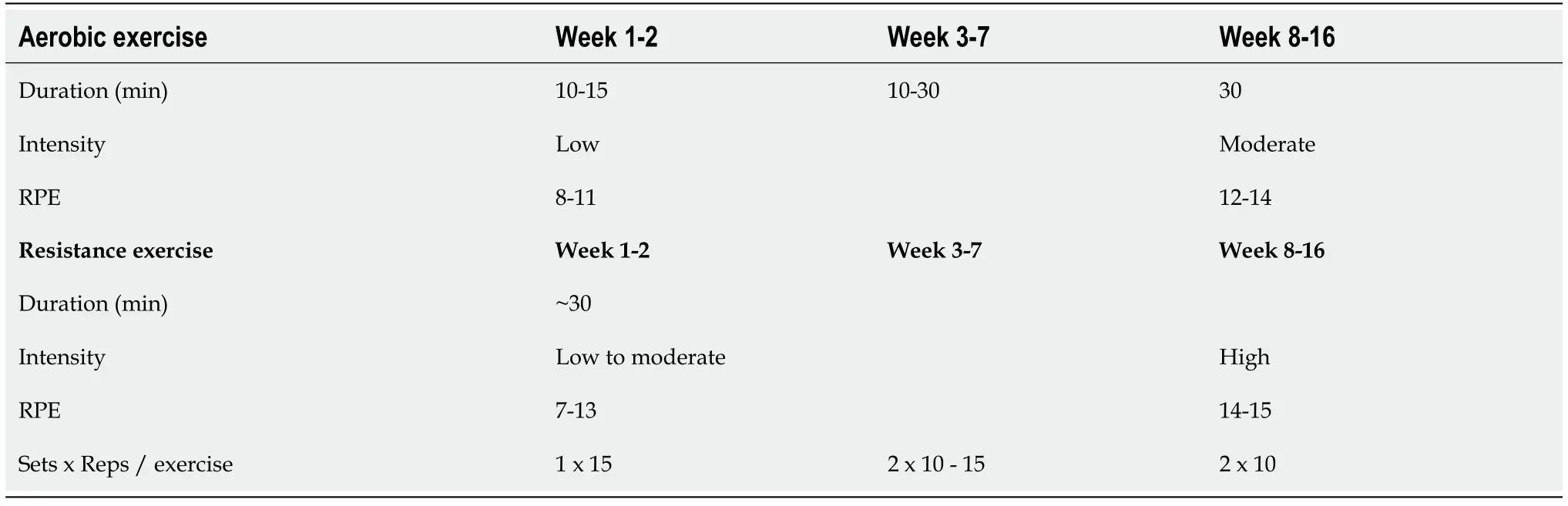
Table 1 Exercise progression in the Get REAL & HEEL Exercise Program
Data collection
Aerobic capacity:Participants completed a familiarization session for the maximal CPET on the first day of data collection using a Corival (Lode B.V., Groningen, The Netherlands) electronically-braked cycle ergometer. Participants were fitted with a Polar heart rate monitor (Polar Electro Inc., Lake Success, NY, United States) and a mask for indirect calorimetry using the ParvoMedics metabolic system. No gas was collected or analyzed on the first day but participants completed a 5-min unloaded and 20 watts loaded cycling warm-up followed by an incremental 15 watts/min with a protocol up to 75% heart rate reserve for familiarization. On day 2 of data collection,participants completed the same CPET protocol but continued until they reached volitional exhaustion or were stopped when oxygen consumption plateaued despite an increase in wattage. Testing was also terminated if cadence was < 50 rpm. Gas exchange data were exported in 5 s average bins, and VO2peakwas recorded as the average of the three highest recordings within the final minute of the maximal test.Time to test termination (TTE) was recorded as the ramp-only portion (excluding the 5-min warm up portion), and peak power was the highest wattage recorded before test termination and were used as additional descriptive data for better interpretation of testing performance. This protocol was repeated at the end of the 16-wk exercise intervention.
Intervention ATT and compliance:Training records were maintained by GRH staff to track participant ATT and compliance over 16 wk. ATT was calculated as the number of days participants came to the facility out of 48 total days of opportunity.Compliance was also included in our study to: help distinguish ATT from fulfillment of the workout prescription; and to quantify completed exercise load and progression,which improves the ability to evaluate effects of the intervention on VO2peakwith more granularity than ATT alone. An aerobic compliant (aCOMP) day was defined as the participant achieving ≥ 80% of the prescribed duration of aerobic exercise within the prescribed RPE range (Borg 6-20 scale[26]). A strength compliant (sCOMP) day was defined as the participant achieving ≥ 80% of prescribed strength volume (sets xrepetitions) within the prescribed RPE range. The 80% duration/volume cutoff in conjunction with RPE as an indicator of intensity was used to help quantify specific training load, not just ATT, and was determined by an experienced exercise oncology research team member as training criteria reasonable to induce changes in aerobic capacity.
Additional outcomes:6MWT and TUG. On the first day of data collection and prior to CPET familiarization, participants completed one 6MWT and two TUG tests to assess functional capacity. The fastest TUG time was recorded for analysis. This protocol was repeated at the end of the 16-wk intervention. These outcomes were included for additional context about participant performance and may be useful for reference/implementation in future work as a more clinically feasible measure of cardiorespiratory fitness and overall functionality alternate to gold standard VO2peakoutcomes,since most community-based program usually do not have the capacity to conduct maximal CPETs.
Power calculations
Published systematic reviews and meta analyses support exercise therapy to increase aerobic capacity in breast cancer survivors by approximately 2.3-2.9 mL O2/kg/min[7,9,12] in laboratory RCTs. For our analysis, power was calculated based on a primary outcome of mean difference in delta VO2peakof BCS following training. Given 80%power and an alpha of 0.05, and assuming a mean difference following training of 2.5 mL O2/kg/min and standard deviation of 3 (d= 0.83), 11 BCS participants would be required. Oversampling was performed to account for potential dropouts and missing data.
Statistical analyses
Statistical analyses were performed using Jamovi open source software (The Jamovi project, version 1.2.5). Baseline descriptive statistics were computed to summarize participant demographics, breast cancer diagnosis/treatment characteristics, and ATT and compliance with the exercise intervention. The α-level was seta priorifor all statistical procedures at < 0.05.
Aerobic capacity following training:The primary aim of this study was to evaluate the impact of a community-based exercise program on change in aerobic capacity(deltaVO2peak) in women with breast cancer measured using the gold standard CPET.
Aerobic capacity between groups following training:A linear mixed model was used to evaluate the impact of the exercise training program on change in aerobic capacity(deltaVO2peak) between women with and without cancer. The model used fixed effects of time (pre-vspost-testing) and condition (BCSvsCTL), and a random effect of subject with adjustment for age. If time-by-condition interactions were not significant,the final models estimated the main effects of condition and time on each outcome.Cohen’sdeffect size was calculated per group as the mean difference from pre- to post-testing, divided by the standard deviation (SD) of the mean difference. Fora prioriinterpretation of effect sizes, Cohen’s “rules of thumb” were used: small = 0.20,medium = 0.50, and large = 0.80[27].
Intervention ATT and compliance:Independent samplest-tests were used to compare exercise ATT and compliance between groups after the intervention. Univariate linear regression models were used to evaluate associations of deltaVO2peakwith days of exercise ATT, days of aCOMP, and days of sCOMP per group. For an exploratory analysis, the two groups were also pooled and reevaluated.
TTE, peak power, 6MWT, and TUG:Separate linear mixed models were used to evaluate the effects of time (pre-vspost-testing) and condition (BCSvsCTL) on time to test termination, peak power, 6MW, and TUG. If time-by-condition interactions were not significant, the final models estimated the main effects of condition and time on each outcome. These analyses were completed to provide supplemental information about the performance changes from participating in a real-world community-based program; programs that provided BCS with flexible opportunities to engage in regular supervised exercise training.
RESULTS
Thirty-five women with breast cancer were enrolled, of which 31 completed all study assessments. Twenty-one non-cancer CTLs were enrolled, of which 15 completed all study assessments (Figure 1). Those who did not complete post-testing were excluded from the analyses due to missing data but were otherwise very similar to women with complete data. At baseline (Table 2), BCS participants were taller (P= 0.035) and had worse TUG performance (P< 0.01) than CTL participants.
Aerobic capacity between settings
Women with breast cancer improved VO2peakfollowing community-based exercise training by 1.2 (3.3) mL O2/kg/min.
Aerobic capacity between participants
There was no significant time x group interaction for VO2peakbut women in both the BCS and CTL groups had significantly improved aerobic capacity by approximately 1.2 mL O2/kg/min (95%confidence interval [CI]: 0.15-2.27, Cohen’sd= 0.36;P= 0.03)from pre- to post-testing (Figure 2A).
Intervention ATT and compliance
Both groups attended the same mean number of training sessions (approximately 34 d of 48 planned;P= 0.420) for an average ATT of 71% (Table 3). Differences in days of aerobic compliance between groups did not reach statistical significance but demonstrated a medium to large effect size (Cohen’sd= 0.63;P= 0.06) with CTL exhibiting more days of aerobic compliance than BCS - 32 (9)vs26 (10) d. Control participants also completed a greater number of compliant strength training days compared to BCS - 18 (3)vs14 (5) d (Cohen’sd= 1.0;P= 0.011). The total number of compliant strength training days was < 40% total days in both groups. There were no significant associations found in univariate analyses between deltaVO2peakand ATT or compliance for either group, independently or in the pooled sample (data not shown).

Table 3 Attendance and compliance (out of 48 total days of training opportunity)
TTE, peak power, 6MWT, and TUG
There was a significant time x group interaction for peak power with both groups demonstrating increased power at post-testing similar to other studies[23], but BCS increased by approximately 10 more watts than the CTLs (95%CI: 1.8-17.5;P= 0.02)(Figure 2B). A significant main effect of time was observed for TTE and 6MWT. Both groups completed almost a minute more of exercise during the peak test (95%CI: 0.60-1.29;P< 0.001) (Figure 2C) and walked approximately 35 meters more in 6 min(95%CI: 21.5-49.1;P< 0.001), which is considered clinically meaningful in clinical populations[28,29], at post-testing. Significant main effects of time and group were observed for TUG with both groups improving time by approximately 0.4 s (95%CI: -0.72-(-0.17);P< 0.01) with an approximately 0.8 s difference between groups at baseline sustained after exercise training (95%CI: 0.21-1.5;P= 0.012).

Figure 1 Recruitment and retention.

Figure 2 Maximal testing results (standard error bars). A: Aerobic capacity; B: Peak Power; C: Time to Exhaustion in breast cancer survivors and controls before and after 16-wk of training. aP < 0.05 for time; cP < 0.05 for group time interaction.
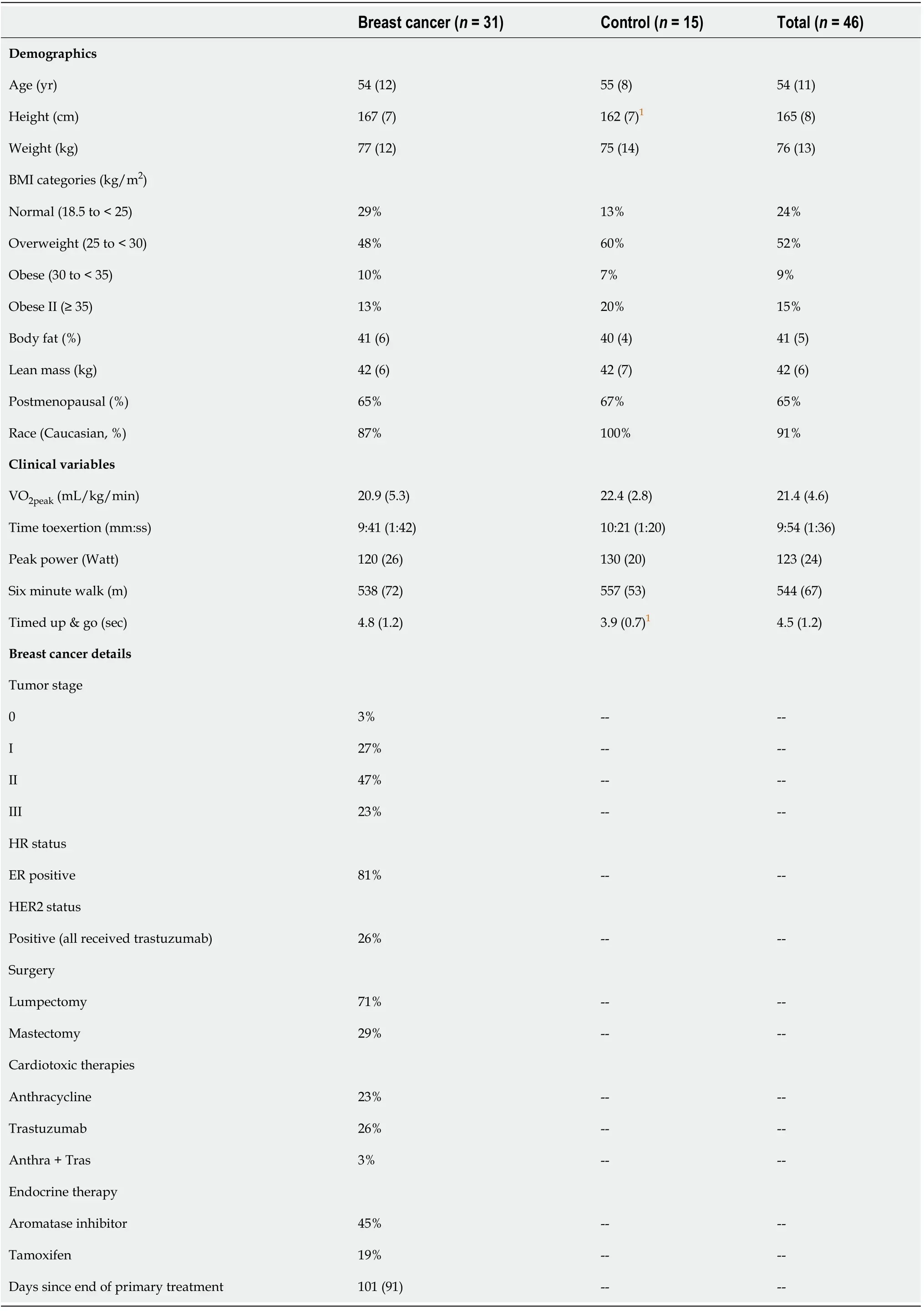
TabIe 2 BaseIine characteristics - mean (SD)
DISCUSSION
Participation in community-based exercise training reflective of recommended guidelines increased aerobic capacity in women with breast cancer in our study, but not to the extent observed in laboratory RCT settings. The 1.2 mL O2/kg/min (+6%)improvement following community-based training is less than the 2.3-2.9 mL/kg/min(approximately 10%-15%) improvement reported in recent meta-analyses; however,the latter interventions were completed in laboratory RCT settings[7,9,12]. Changes in VO2peakfollowing training in non-RCT settings have been only minimally evaluated using gold standard methodology[13] in contrast to alternatives such as submaximal VO2peaktesting, 6MWT, and/or TUG[14,16,17,30] but have nonetheless supported beneficial changes. However, while the transition of interventions from laboratory settings to community settings is increasing[13,31,32], it is important to evaluate outcomes with gold standard testing to ensure survivors are receiving effective intervention in this newer setting. While the aerobic capacity improvement in our study may be small, substantial decline in aerobic capacity is a known manifestation of cancer survivorship[1,3,33]. Therefore, maintenance or even slight improvement is encouraging especially in conjunction with the observed improvements in peak cycling power and cycling endurance. Furthermore, while functional capacity (6MWT and TUG) of BCS in our study is not equivalent to non-cancer population norms[34], it reflects improvement commonly observed for women with breast cancer[35], which is of clinical relevance[28,29] and underscores the beneficial impact of exercise for demands of daily life.
Both women with and without breast cancer in our study demonstrated similar improvements in aerobic capacity (+1.2 mL/kg/min;P= 0.03) following the community-based exercise program. Interestingly, VO2peakof both groups reflected that of published norms for women with breast cancer who are post-treatment (21.5 mL O2/kg/min)[2]. For CTL participants, this is substantially lower than conventional standards[36]. Recently, our laboratory has consistently observed impaired VO2peakin both BCS and middle-aged, sedentary women without cancer[37,38]. We speculate that this may reflect a regional fitness characteristic but warrants further investigation.In terms of training response for non-cancer populations, interventions similar to our study have generally elicited up to a 15% improvement in VO2peak[39,40]. Therefore, the approximate 6% improvement observed in our study is also less than what is considered clinically significant in non-cancer populations[41,42]. The relatively poor compliance observed in our study indicates that prescribed training progression was not followed and may provide a partial explanation for the relatively modest improvements observed in VO2peak. Exercise dosing and progression are important components related to the FITT principle[20,21,43] and are important factors for impacting patient physical and functional outcomes[8,11,44]. Furthermore, while ATT in our study (71%, attending about 2 of 3 training days per week) is similar to other exercise oncology interventions (approximately 70%-75%)[19,20,45], it reflects less than that recommended by national guidelines (≥ 3 d/wk, ≥ 30 min/d)[11]. It is reasonable to consider that improved exercise ATT closer to or matching the established,recommended guidelines in addition to improved compliance (which considers progressing intensity) would lead to more optimal physiological changes. However,despite modest intervention engagement, participants in our study still demonstrated positive/beneficial training adaptations which reiterates the need to investigate the fundamental question of what is the optimal training prescription for this population[9,23,43,46].
The ability to provide a community-based program that may improve physical and functional health and that survivors enjoy is paramount, especially when a survivor needs to prioritize aspects of work, life, and family around exercise[20,46]. Documenting exactly why patients missed sessions was not specifically recorded in this study but were anecdotally related to job, family, or general life obligations. Survivors also frequently expressed enjoyment with study participation and the GRH program,and many women regretted not having started their exercise journey earlier in treatment process. With respect to our generally positive findings, community-based programs such as GRH appear to have a place in cancer survivorship. Continued focus and conversations with survivors to better understand challenges around exercise compliance may help identify targets to improve engagement, and should remain a priority.
Difficulties with exercise engagement and compliance reflect the well-recognized challenges of exercise programming for clinical populations[19-21,47,48]. Based on the observations of our exercise staff and research team, participant compliance was primarily hindered by not achieving prescribed intensity, as measured by self-reported RPE. This method has the inherent weakness of subjectivity; however, it was the most feasible option in our relatively small community-based setting where, historically,heart rate monitor transmitter signals have overlapped between participants,displayed incorrectly, and caused unnecessary worry/confusion to an otherwise upbeat and positive environment. In our study, it was observed that while participants would and could complete both prescribed duration (aerobic) and volume (sets x reps,strength), there was reluctance to increase intensity (grade/speed/weight,etc.)especially in the second half of training when intensity targets increased. Strength training intensity targets were achieved less frequently than aerobic for both groups,leading to fewer strength compliant days than aerobic (Table 3), which has been observed previously in this population[20,49,50]. GRH training staff encouraged and guided participants how to safely reach more difficult intensities and no adverse events were documented during training; therefore, lack of training support, injury, or unnecessary discomfort were unlikely contributors to sub-optimal compliance, yet successfully increasing intensity remained a challenge. While participants were reminded how to contextualize and use the RPE scale, it is possible there was misunderstanding or concern from participants that reporting a higher RPE somehow suggested they were less capable of completing the prescribed exercise.
The primary limitation of our study is that it was a small, self-selected sample of mostly White women willing who were able to engage in exercise training for 4 consecutive months. This is not representative of the majority of women with breast cancer, especially younger women who may have acute family and job demands. The greatest strength of this study was the well-established, long-standing communitybased exercise oncology program with veteran training staff, but we recognize that this experienced environment is difficult to replicate[13,51-53] especially in partnership with facilities capable of gold standard testing.
Future research would benefit from the inclusion of more diverse participants and from continued efforts to explore barriers and facilitators of exercise engagement.Calculation of both ATT and compliance in community-based settings similar to the methods presented in our study would improve the ability to quantify exercise load,progression, and dose responses more precisely. Heart rate monitoring in addition to self-reported RPE may also help better communicate and indicate training intensity,especially as technology for self-monitoring progresses. Directly collecting more information from participants about missed sessions and live feedback during training sessions would help provide better understanding of participant barriers, concerns,and potential limitations to engagement. These improvements would help contribute to the development of more specific future exercise prescriptions that are both suitable and effective in community-based settings. Furthermore, a third group of BCS who did not exercise for 16-wk, or who completed prescriptions with differing levels of exercise volume (days/reps/time) and/or undulating intensity progression (highvslow intensity) would help clarify specific findings from the current study and enhance future designs.
CONCLUSION
A community-based exercise program such as GRH can improve aerobic capacity and overall physical function in women with breast cancer, potentially not to the extent of an exercise oncology laboratory based RCT setting but similar to that of women without a cancer diagnosis participating in a similar program. Survivors may not meet recommended physical activity guidelines immediately, but proper training accommodations may help facilitate and encourage the integration of exercise as a daily routine. This is an important first step to life-long exercise commitment and provides the foundation to achieve recommended guidelines. Community-based venues offering exercise oncology programs have the potential to augment long term cancer care[13], will be essential for accommodating the growing number and needs of survivors[18], and should be continually evaluated as interventions are implemented in new settings.
ARTICLE HIGHLIGHTS
Research background
Exercise is an efficacious strategy to improve aerobic capacity of breast cancer survivors (BCS) but has not been consistently evaluated with gold standard testing in community-based settings.
Research motivation
As a growing number of BCS are in need of community-based exercise access,providing effective interventions is paramount to their long term health and functionality.
Research objectives
The objective was to use gold standard testing to determine whether breast cancer survivors exhibit similar improvement in aerobic capacity (maximal oxygen consumption [VO2]) following community-based exercise compared to interventions in laboratory settings.
Research methods
A peak cardiopulmonary exercise test (VO2peak), 6-min walk test (6MWT), and timed up and go test (TUG) were assessed pre- and post-16 wk of progressive intensity aerobic and strength training exercise at a community center.
Research results
Both BCS (n= 31) and CTL (n= 15) groups significantly improved physical and functional capacity following training (VO2peak+1.2 mL/kg/min,P= 0.030; 6MWT +35 meters,P< 0.001; TUG -0.44 s;P< 0.01). Peak cycling power improved in both groups with BCS exhibiting 10 watts more improvement than CTL (P= 0.020). Average exercise ATT of 71%, 34/48 possible days) is in accordance with previous work, and the modest compliance (60% aerobic, < 40% resistance) emphasizes the challenges of exercise engagement in clinical populations.
Research conclusions
A community-based exercise program can effectively improve aerobic capacity and physical function for early stage breast cancer survivors but potentially not to the same extent observed in laboratory-based randomized controlled trials. Further research is needed to explore barriers and facilitators of exercise engagement in community-based centers to maximize training benefits for adults with cancer.
Research perspectives
Providing BCS with accessible and effective exercise interventions is a critical component in survivorship and should be continually evaluated with gold standard outcomes, especially because it is not yet a standard intervention of oncology practice.
 World Journal of Clinical Oncology2021年6期
World Journal of Clinical Oncology2021年6期
- World Journal of Clinical Oncology的其它文章
- Long-term complete response in metastatic poorly-differentiated neuroendocrine rectal carcinoma with a multimodal approach: A case report
- Phytochemically rich dietary components and the risk of colorectal cancer: A systematic review and meta-analysis of observational studies
- Chemotherapy-induced neurotoxicity in the treatment of gynecological cancers: State of art and an innovative approach for prevention
- Imaging diagnosis of bronchogenic carcinoma (the forgotten disease) during times of COVID-19 pandemic: Current and future perspectives
- Review of 10 years of research on breast cancer patients: Focus on indoleamine 2,3-dioxygenase
- Breast cancer: Muscarinic receptors as new targets for tumor therapy
