Combination of type IV collagen 7S, albumin concentrations, and platelet count predicts prognosis of non-alcoholic fatty liver disease
Miwa Kawanaka, Ken Nishino, Katsunori Ishii, Tomohiro Tanikawa, Noriyo Urata, Mitsuhiko Suehiro, Takako Sasai, Ken Haruma, Hirofumi Kawamoto
Miwa Kawanaka, Ken Nishino, Katsunori Ishii, Tomohiro Tanikawa, Noriyo Urata, Mitsuhiko Suehiro, Takako Sasai, Ken Haruma, Hirofumi Kawamoto, Department of General Internal Medicine, Kawasaki Medical School, Okayama 700-8505, Japan
Abstract BACKGROUND Non-alcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease and affects approximately 25% of the general global adult population.The prognosis of NAFLD patients with advanced liver fibrosis is known to be poor.It is difficult to assess disease progression in all patients with NAFLD; thus, it is necessary to identify patients who will show poor prognosis.AIM To investigate the efficacy of non-invasive biomarkers for predicting disease progression in patients with NAFLD.METHODS We investigated biomarkers associated with mortality in patients with NAFLD who visited the Kawasaki Medical School General Medical Center from 1996 to 2018 and underwent liver biopsy and had been followed-up for > 1 year.Cumulative overall mortality and liver-related events during follow-up were calculated using the Kaplan-Meier analysis and compared using log-rank testing.We calculated the odds ratio and performed receiver operating characteristic curve analysis with logistic regression analysis to determine the optimal cut-off value with the highest prognostic ability.RESULTS We enrolled 489 patients who were followed-up for a period of 1-22.2 years.In total, 13 patients died (2.7% of total patients enrolled); 7 patients died due to liverrelated causes.Poor prognosis was associated with liver fibrosis on histological examination but not with inflammation or steatosis.Blood biomarkers associated with mortality were platelet counts, albumin levels, and type IV collagen 7S levels.The optimal cutoff index for predicting total mortality was a platelet count of 15 × 104/μL, albumin level of 3.5 g/dL, and type IV collagen 7S level of 5 mg/dL.In particular, only one-factor patients with NAFLD presenting with platelet counts ≤ 15 × 104/μL, albumin levels ≤ 3.5 g/dL, or type IV collagen 7S ≥ 5 mg/dL showed 5-year, 10-year, and 15-year survival rates of 99.7%, 98.3%, and 94%, respectively.However, patients with two factors had lower 5-year and 10-year survival rates of 98% and 43%, respectively.Similarly, patients with all three factors showed the lowest 5-year and 10-year survival rates of 53% and 26%, respectively.CONCLUSION A combination of the three non-invasive biomarkers is a useful predictor of NAFLD prognosis and can help identify patients with NAFLD who are at a high risk of all-cause mortality.
Key Words: Non-alcoholic fatty liver disease; Non-alcoholic steatohepatitis; Platelet count; Albumin; Type IV collagen 7S; All-cause mortality
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease and affects approximately 25% of the general global adult population[1].The development of NAFLD is associated with lifestyle-related diseases, such as obesity, type 2 diabetes, hypertension, and dyslipidemia.Cardiovascular disease is the leading cause of death among NAFLD patients[2,3].However, liver-related diseases are also a major cause of death among patients with NAFLD, and liver-specific and all-cause mortality rates are higher for these patients than for the general population NAFLD, and liver-specific and all-cause mortality rates are higher for these patients than for the general population[1].The incidence of liver-specific and all-cause mortality among patients with NAFLD is generally 0.77 and 11.77 per 1000 years, respectively, while it is 15.44 and 25.56 per 1000 years, respectively, for patients with non-alcoholic steatohepatitis (NASH)[1].
The prognosis of NAFLD patients with advanced liver fibrosis is known to be poor[1,4-8].Progression of liver fibrosis in patients with NAFLD is associated with mortality from various non-liver-related causes[6].
Liver biopsy is typically performed for diagnosing advanced fibrosis in patients with other liver diseases, such as NASH; however, it is not a practical tool for the diagnosis of NAFLD.In addition, the limitations of liver biopsies, such as invasiveness, poor patient tolerance, sampling variability, and high costs, are well known.Thus, there is increasing interest in developing and validating non-invasive methods for measuring liver stiffness, such as imaging and elastography techniques based on ultrasonography or magnetic resonance imaging[3,4,9-14].However, a limitation of these methods is that the images are visualized using an instrument that is not available in many institutions.Therefore, serum biomarkers that can assess the progression of liver fibrosis in patients with NAFLD may serve as important tools for identifying patients with advanced fibrosis.Some biomarkers of interest, such as procollagen type III N-terminal propeptide, type IV collagen 7S, hyaluronic acid, and Mac-2 binding protein [WFA(+)-M2BP] levels, and cytokeratin-18 have been used for identifying patients with NAFLD with advanced fibrosis.Other studies have used different biomarker scores, such as the BARD score, NAFLD fibrosis score, FIB-4 (fibrosis-4) index, aspartate aminotransaminase (AST) to alanine aminotransaminase (ALT) ratio, AST to platelet ratio index, FibroTest, and Enhanced Liver Fibrosis score, for the assessment of liver fibrosis[3,4,11,13,14-24].However, none of these scores predict the prognosis of NAFLD patients.Hence, we aimed to investigate the efficacy of non-invasive biomarkers for predicting disease progression in patients with NAFLD.
MATERIALS AND METHODS
Patients
We retrospectively identified patients with NAFLD who underwent liver biopsy at the Kawasaki Medical School General Medical Center from 1996 to 2018 (Table 1).The exclusion criteria were as follows: history of other liver diseases including hepatitis B virus or hepatitis C virus infections, autoimmune liver diseases, drug-induced liver injury, metabolic liver diseases, or history of alcohol intake (men, ≥ 30 g/d and women, ≥ 20 g/d).Blood tests were performed before the liver biopsy, and we examined the prognostic factors based on the blood test results.The study protocol complied with the guidelines of the 1975 Helsinki Declaration and was approved by the Institutional Research Ethics Committee.Written informed consent was obtained from all the patients.
Clinical, biochemical, and histological parameters
We investigated the mortality rate and causes of death among the enrolled patients.We also investigated the development of any complications during the follow-up period.The start date of the follow-up period was defined as the date of liver biopsy and the end date of the follow-up period was defined as the date of last follow-up for surviving patients or the date of death for patients who died during the follow-up period.All NAFLD patients visited our hospital once every 3-6 mo.The following clinical parameters were included in the analysis: age at diagnosis of NAFLD; sex; body mass index calculated as weight (in kg) divided by height (in meters squared); and the presence of diabetes mellitus, hyperlipidemia, and dyslipidemia.We also included the following biochemical parameters in the analysis: platelet count, levels of albumin, total bilirubin, AST, ALT, gamma glutamyl transpeptidase, total cholesterol, cholinesterase, serum iron, ferritin, leptin, adiponectin, and high-sensitivity C-reactive protein, and homeostasis model assessment insulin resistance.The FIB-4 index was calculated as follows: age (years) × AST (U/L)/platelet count (× 104/μL) × √AST (U/L)[13,16,17].Type IV collagen 7S and procollagen III peptide (P-III-P) were used as indicators of liver fibrosis.
Liver biopsy and histological analysis
All liver biopsies were performed using 16G or 17G biopsy needles with ultrasound guidance or using 14G needles with laparoscopic guidance.The histological examinations were performed by two experienced liver pathologists who were blinded to the patient details.The histological parameters included fibrosis, inflammation, steatosis, hepatocyte ballooning, and the NAFLD activity score (NAS) system[25].The individual histological features of NAFLD were assessed using the following NAS system proposed by the NASH Clinical Research Network (NASH CRN): lobular inflammation (0-3), steatosis (0-3), and hepatocellular ballooning (0-2)[26,27].The liver fibrosis stages were assessed according to Brunt’s criteria.
Statistical analysis
The cumulative all-cause mortality and liver-related events during follow-up were assessed using the Kaplan-Meier method and compared using the log-rank test.The Kaplan-Meier analysis included the following variables: steatosis grade, ballooning grade, NAS category, fibrosis stage, albumin, platelet counts, type IV collagen 7S levels, and FIB-4 index.We also calculated the odds ratio and performed receiver operating characteristic (ROC) curve analysis with logistic regression analysis to determine the cutoff values with the highest predictive ability.The optimal cut-off value was determined based on the Youden index.The prognostic performance of the optimal cutoff value was expressed as the diagnostic specificity, sensitivity, positive predictive value, and negative predictive value, using area under the ROC (AUROC) curve analysis.In univariate (unadjusted) and multivariate (adjusted) analyses, the hazard rate ratio estimates (relative risk) for outcomes were calculated using Cox proportional hazard regression analysis to control for the effect of potential risk factors (confounders) while considering the different follow-up durations.APvalue < 0.05 was considered significant.All statistical analyses were performed using JMP (version 14.2, SAS system, United States).The statistical methods of this study were reviewed by Akiyoshi Izumi from Asahigawaso Rehabilitation and Medical Center, Okayama.
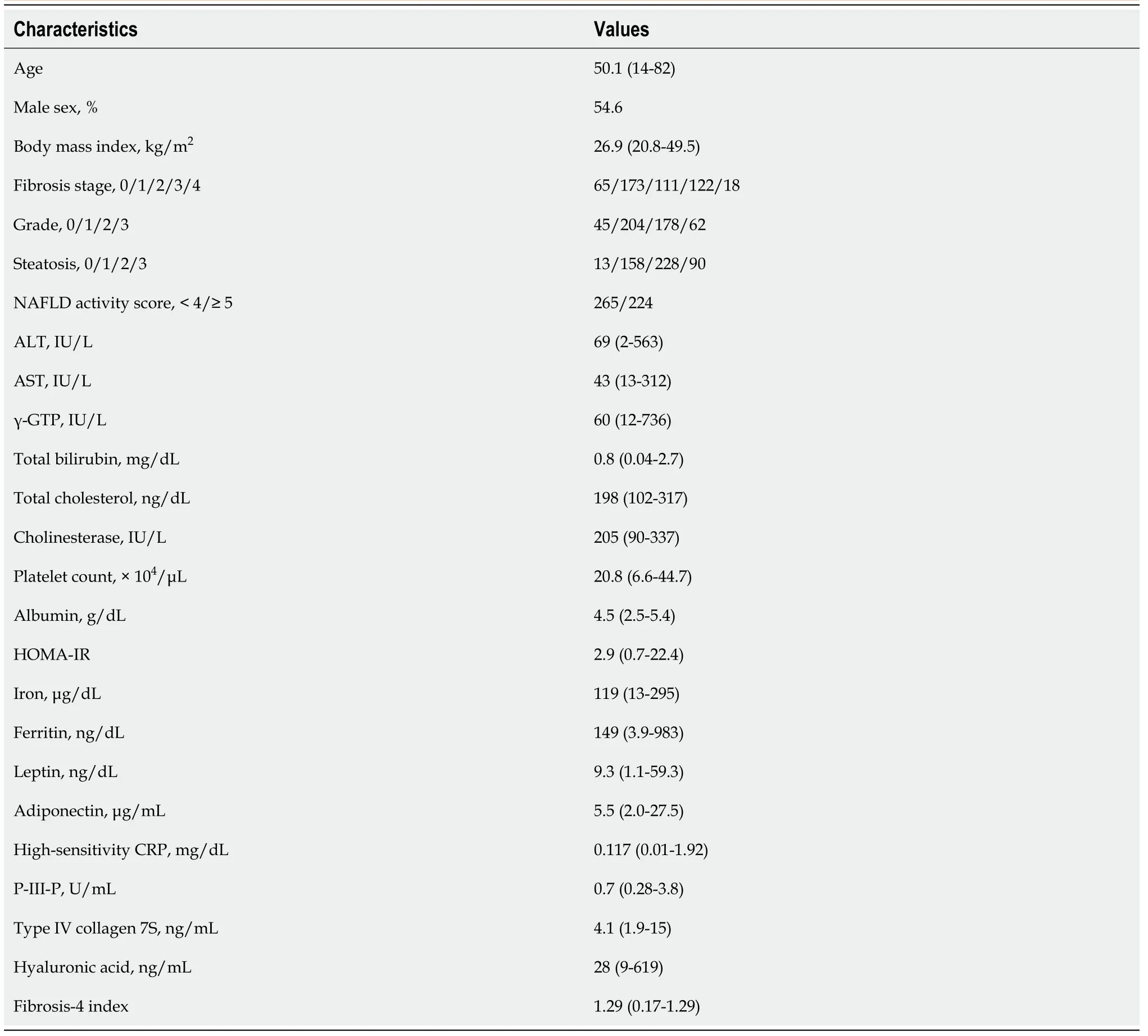
Table 1 Clinical and histological characteristics of the patient population (n = 489)
RESULTS
Survival rate
In total, 489 patients were enrolled in the present study; the 5-year survival rate was 98.5%, and the 10-year, 15-year, and 20-year survival rates were 95.4%, 91.9%, and 91.9%, respectively.The follow-up period varied between 1 and 22.2 years (Figure 1).In total, 13 (2.7%) patients died; of these, 7 patients died of liver-related causes [hepatocellular carcinoma (HCC) was observed in 1 patient; Table 2].The complications that developed during the follow-up period were HCC (n= 12), other organ cancers (n= 13), and cerebrovascular disorders (n= 9).
Liver histological findings
Patients presenting with progression of advanced liver fibrosis after liver biopsy had increased mortality.The 5-year and 10-year survival rates of patients with NASH CRN Stage 4 disease were 81% and 41%, respectively.However, the degree of inflammation or steatosis was not associated with poor prognosis.The optimal area under the curve for albumin was 3.8 and 3.5 with specificities of 47% and 39%, sensitivities of 95% and 99%, positive predictive values of 98% and 98%, and negative predictive values of 21% and 56% (Figure 2).
Blood test factors
A univariate Cox hazard model was used for analyzing factors associated with mortality at the time of diagnosis of the NASH Clinical Research Network.We found that the ALT levels, platelet counts, albumin levels, and levels of liver fibrosis markers (P-III-P, type IV collagen 7S and FIB-4 index) were significantly associated with mortality (Table 3).
Survival curves were created using the following biomarkers: type IV collagen 7S, platelet count, albumin, and FIB-4 index.ALT was not included as a biomarker because the levels frequently varied.To investigate the predictive performance of these biomarkers with respect to NAFLD mortality, an optimal COI for type IV collagen 7S level, platelet count, albumin level, and FIB-4 index was determined based on the ROC curve analysis of all 489 patients with NAFLD.As shown in Figure 3A-D, the cutoff values for the platelet count, albumin level, type IV collagen 7S concentration and the FIB-4 index were set at 15 × 104, 3.8 g/dL, and 3.5 mg/dL, 5.0 ng/mL, and 1.3 and 2.61, respectively.
At the time of NASH diagnosis, patients with albumin levels < 3.5 mg/dL, platelet counts < 15 × 104, type IV collagen 7S levels ≥ 5 ng/dL, and FIB-4 indexes ≥ 2.67 clearly showed reduced survival (Figure 4A-D).Furthermore, we investigated the prognosis by combining type IV collagen 7S, which had a high AUROC among liver fibrosis markers (type IV collagen 7S, P-III-P, and FIB-4 index), the albumin level, and platelet count.Albumin level < 3.5 mg/dL, platelet count < 15 × 104/µL, and type IV collagen 7S levels ≥ 5 ng/dL were examined individually and in combination.The 5-year, 10-year, and 15-year survival rates for patients with only one factor were 99.7%, 98.3%, and 94%, respectively.However, survival rates were low for patients who presented with more than one factor.For these individuals, the 5-year and 10-year survival rates were 98% and 43%, respectively.For those who presented with two factors, the 5-year and 10-year survival were 53% and 26%, respectively, and for those presenting with three factors (Figure 5).
DISCUSSION
To the best of our knowledge, this study is the first study to evaluate the predictors of the prognosis of NAFLD based on the results of a blood test.We found that a combination of three non-invasive biomarkers, namely, platelet count, albumin level, and type IV collagen 7S level, is a useful predictor of NAFLD prognosis.The major causes of death in patients with NAFLD are cardiovascular events, organ cancers other than liver cancer, and liver-related disease.Among Japanese patients with NAFLD, the reported mortality rates associated with NAFLD are low during the follow-up period.The causes of death are more likely to be cancers of other organs and cerebral cardiovascular events than liver-related pathologies[28].
The most important predictor of outcomes among patients with NAFLD is the progression of liver fibrosis[1,5-7].Anguloet al[6] retrospectively analyzed the longterm outcomes of 619 patients diagnosed with NAFLD in the United States, Europe, and Thailand during 1975-2005[6] and reported that only liver fibrosis, among various longitudinal histological features, was associated with disease prognosis.Only liver fibrosis was independently associated with long-term all-cause mortality, liver transplantation, and liver-related events.Meta-analyses have also reported that liver fibrosis is an important risk factor for liver-related mortality[1,7].Compared with NAFLD patients without fibrosis, NAFLD patients with fibrosis were at an increased risk of all-cause mortality, and the risk increased as fibrosis progressed[7].In our study, patients with advanced liver fibrosis, especially cirrhosis, also showed poor prognosis; however, an association with inflammation, steatosis, or ballooning was not noted.Our findings further confirm that the progression of fibrosis markedly affects the prognosis of patients with NAFLD.
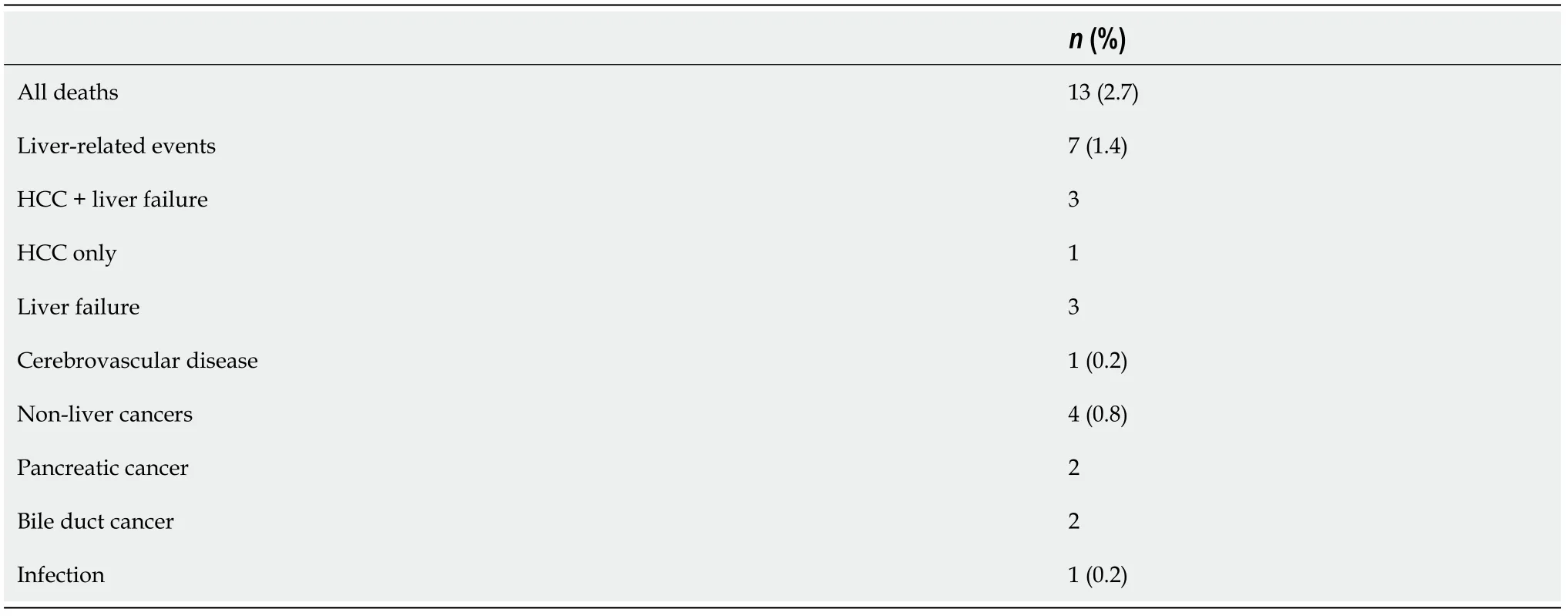
Table 2 Summary of the causes of death

Table 3 Factors associated with mortality among the patients with non-alcoholic fatty liver disease (n = 489)
Several biomarkers can be used to evaluate liver fibrosis in patients with NAFLD[3,4,11,13,14-25,29]; however, previous studies have not examined disease prognosis using blood biomarker levels recorded at the time of NAFLD diagnosis using liver biopsy.

Figure 1 Survival of the 489 patients with non-alcoholic fatty liver disease.

Figure 2 Survival rates according to the grading of fibrosis, inflammation, and steatosis.
NAFLD may progress rapidly in some patients and slowly in other patients.Singhet al[5] performed a systematic review and meta-analysis of 11 paired biopsy cohort studies that included 411 patients with > 2145 person-years of follow-up data and reported that approximately 30% of the patients developed advanced fibrosis and 70% of the patients remained stable or the stage of fibrosis in these patients improved.Furthermore, the annual fibrosis progression rates were 0.07 stages for patients with NAFLD and 0.14 stages for patients with NASH.Nasret al[30] conducted a biochemical, clinical, and histological analysis of 129 patients with NAFLD who were enrolled between 1988 and 1993 in a prospective cohort study and followed them for 19.8 years.They reported that end-stage liver disease developed in 12 (9.3%) patients and advanced fibrosis developed in 34% of the patients.Furthermore, among the 113 patients with low baseline fibrosis (stage 3), 16% of the patients developed advanced fibrosis.No differences in clinical, histological, or biochemical variables were observed between patients who developed liver fibrosis and those who did not.These studies did not examine the association ofPNPLA3polymorphisms with menopause.Although the difference in the progression of NASH and NAFLD is not clear, racial differences and genetic factors, includingPNPLA3expression[31], weight gain, onset and deterioration of diabetes[32], sex differences, and menopausal factors, affect prognosis[33].

Figure 3 Receiver-operating characteristic curves for survival among patients with non-alcoholic fatty liver disease.
It is necessary to consider the various factors that affect disease progress in each case of NAFLD.Although several studies have reported on the evaluation of biomarkers and elastography methods that can predict the progression of liver fibrosis[3,4,11,13,14-25], non-invasive biomarkers that can easily predict the prognosis of NAFLD have not been identified to date.
Our results indicate that patients with NAFLD who present with a combination of albumin level < 3.5 g/dL, platelet count < 15 × 104/µL, and type IV collagen 7S level ≥ 5 ng/mL show poor prognosis.In particular, the 10-year survival rate was only 43% for patients who presented with all three factors.We observed that type IV collagen 7S was a more useful indicator of advanced liver fibrosis than other biomarkers (Table 3).Yonedaet al[24] reported that the type IV collagen 7S level is a more useful marker of prognosis for patients with advanced fibrosis associated with NASH than for patients with mild fibrosis.Furthermore, a scoring system that uses type IV collagen 7S and AST levels, named the CA index, has been reported to predict NASH and fibrosis associated with NAFLD with sufficient accuracy, thus allowing for convenient diagnosis and screening of NASH and associated fibrosis[21].The same index was found to be useful in 400 Japanese patients from 18 institutes with biopsy-proven NAFLD and advanced liver fibrosis due to CA or FA fibrosis.The CA index is a combination of AST and type IV collagen 7S levels, and the FM fiber index includes type IV collagen 7S and hyaluronic acid levels and vascular cell adhesion[25].The type IV collagen 7S level is useful for determining advanced fibrosis in patients with NASH and was found to be more sensitive and specific than other fibrosis markers assessed in our study.
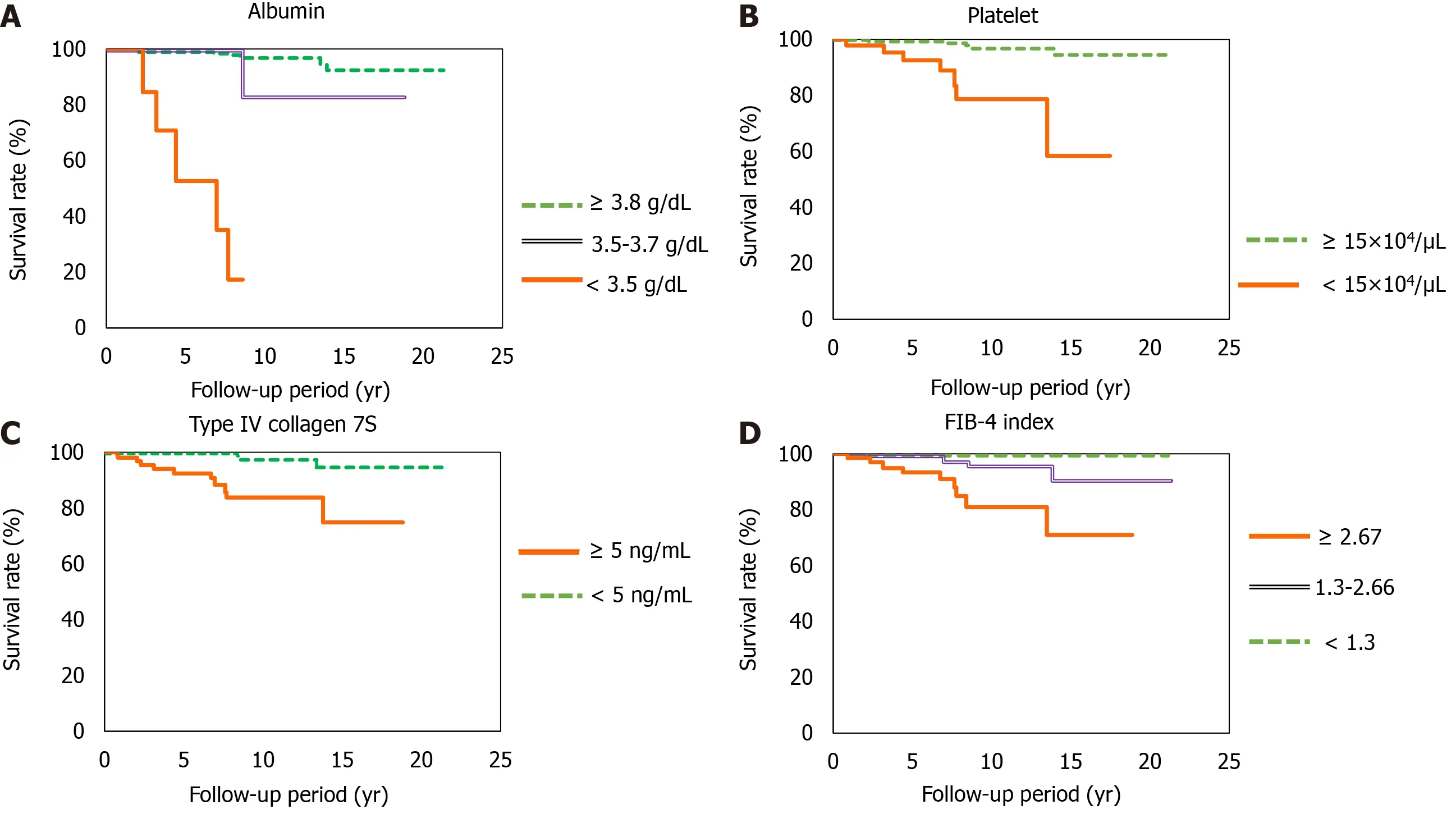
Figure 4 Survival rates.

Figure 5 Survival rates according to positivity for the different biomarkers.
Albumin is also an important biomarker for predicting the prognosis of HCC in patients with NAFLD.Kawaguchiet al[34] analyzed the factors affecting survival by performing a random forest analysis for 247 NAFLD-HCC patients diagnosed between 2000 and 2014 and recruited from 17 medical institutions in Japan.The results showed that the best prognostic profile for patients with NAFLD-HC comprised treatment for HCC and serum albumin levels > 3.7 g/dL.
There are some limitations of this study.We did not classify prognosis according to all-cause mortality; moreover, the study population comprised patients from at a single center.Nevertheless, it is significant that the study followed a long-term course of up to 20 years.
In our study, the platelet count, albumin level, type IV collagen 7S level, and the FIB-4 index were important prognostic factors at the time of diagnosis of NAFLD.Our findings suggest that these factors should be recorded in patients with NAFLD at the time of diagnosis to determine future treatment strategies.
Studies conducted in the future should focus on assessing these biomarkers further and examining long-term prognosis using Fibroscan and magnetic resonance elastography.Further research is also needed to confirm these findings in other populations.
CONCLUSION
This study may prove useful in clinical practice because simple predictors of NAFLD progression, namely, albumin level, platelet count, and type IV collagen 7S level, were identified; all these parameters are can be easily assessed in daily practice.
ARTICLE HIGHLIGHTS
Research background
Non-alcoholic steatohepatitis has few symptoms until it progresses; thus, it is necessary to identify non-alcoholic fatty liver disease (NAFLD) patients who will show poor prognosis.
Research motivation
The limitations of liver biopsies, such as invasiveness, poor patient tolerance, sampling variability, and high costs, are well known.Thus, there is increasing interest in developing and validating non-invasive methods for measuring liver stiffness.However, many current methods involve instruments that are not available in many institutions.
Research objectives
Serum biomarkers that can assess the progression of liver fibrosis in patients with NAFLD may serve as important tools for identifying patients with advanced fibrosis.We aimed to investigate the efficacy of non-invasive biomarkers for predicting disease progression in patients with NAFLD.
Research methods
We investigated biomarkers with predictable prognosis for NAFLD patients who underwent liver biopsy.All patients were followed-up for > 1 year.
Research results
The combination of three non-invasive biomarkers involved in NAFLD prognosis comprised platelet counts, albumin levels, and type IV collagen 7S.Our results indicate that patients with NAFLD who present with a combination of albumin levels< 3.5 g/dL, platelet counts < 15 × 104/μL, and type IV collagen 7S levels ≥ 5 ng/mL show poor prognosis.In particular, the 10-year survival rate was only 43% for patients who presented with all three factors.
Research conclusions
The combination of platelet count, albumin level, and type IV collagen 7S was useful in further predicting the prognosis of NAFLD.
Research perspectives
Studies conducted in the future should focus on assessing these biomarkers further and examining long-term prognosis.
 World Journal of Hepatology2021年5期
World Journal of Hepatology2021年5期
- World Journal of Hepatology的其它文章
- COVID-19 and the liver: What do we know so far?
- Direct, remote and combined ischemic conditioning in liver surgery
- Bile acid indices as biomarkers for liver diseases II: The bile acid score survival prognostic model
- Gut dysbiosis is associated with poorer long-term prognosis in cirrhosis
- Surgical treatment outcomes of primary hepatic sarcomas: A singlecenter experience
- Endoscopic retrograde cholangiopancreatography drainage for palliation of malignant hilar biliary obstruction — stent-in-stent or side-by-side? A systematic review and meta-analysis
