Direct, remote and combined ischemic conditioning in liver surgery
Rafał Stankiewicz, Michał Grąt
Rafał Stankiewicz, Michał Grąt, Department of General, Transplant and Liver Surgery, Medical University of Warsaw, Warsaw 02-097, Poland
Abstract Liver ischemia-reperfusion injury is a major cause of postoperative liver dysfunction, morbidity and mortality following liver resection and transplantation.Ischemic conditioning has been shown to ameliorate ischemiareperfusion injury in small animal models.It can be applied directly or remotely when cycles of ischemia and reperfusion are applied to a distant site or organ.Considering timing of the procedure, different protocols are available.Ischemic preconditioning refers to that performed before the duration of ischemia of the target organ.Ischemic perconditioning is performed over the duration of ischemia of the target organ.Ischemic postconditioning applies brief episodes of ischemia at the onset of reperfusion following a prolonged ischemia.Animal studies pointed towards suppressing cytokine release, enhancing the production of hepatoprotective adenosine and reducing liver apoptotic response as the potential mechanisms responsible for the protective effect of direct tissue conditioning.Interactions between neural, humoral and systemic pathways all lead to the protective effect of remote ischemic preconditioning.Despite promising animal studies, none of the aforementioned protocols proved to be clinically effective in liver surgery with the exception of morbidity reduction in cirrhotic patients undergoing liver resection.Further human clinical trials with application of novel conditioning protocols and combination of methods are warranted before implementation of ischemic conditioning in day-to-day clinical practice.
Key Words: Ischemic preconditioning; Ischemia-reperfusion injury; Hepatectomy; Liver transplant; Morbidity; Mortality
INTRODUCTION
Ischemia-reperfusion injury (IRI) remains an important issue in hepatic surgery.IRI is a pathophysiological phenomenon where cellular damage is caused by reperfusion and reoxygenation following an ischemic period[1].It is the most important pathogenetic factor occurring during the surgical procedure that impairs both functional reserve through loss of remaining hepatocytes and compromising liver capacity to regenerate.Thus, IRI is a major contributor to increased morbidity and mortality following liver resection and transplantation[2,3].
Ischemic preconditioning (IPC) is an adaptive pathophysiological mechanism based on a concept of preparation of the target organ for ischemic conditions in order to decrease the magnitude of IRI[4].It was first described by Murryet al[5] in 1986.In a canine model, the authors demonstrated that short repetitive ischemic episodes protected the heart from subsequent sustained ischemic insult.
IPC can be either applied directly[5] or remotely[6].Remote IPC (RIPC) is based on a concept of brief cycles of ischemia and reperfusion applied to a distant site or organ in order to exert a protective effect on another organ or site.Considering timing of the procedure, remote ischemic perconditioning (RIPer) refers to that performed over the duration of ischemia of the target organ[7].
Potential mechanisms responsible for the protective effect of tissue conditioning remain poorly understood.Regarding direct conditioning strategies, it is postulated that IPC suppresses cytokine release, enhances the production of hepatoprotective adenosine and nitric oxide and increases ATP availability by slowing the rate of ATP depletion, thus leading to upregulation of the process of cellular ATP production and liver regeneration and reduction of the liver apoptotic response[8,9].The summary of IRI mechanism and pathways of IPC is illustrated in Figure 1[10].In remote ischemic conditioning, reduction of hepatocellular injury in the early phase of IRI is achieved by improvement of parenchymal perfusion and oxygenation[11,12].Interactions between neural, humoral and systemic pathways all lead to the protective effect of RIPC.In particular, these result in inhibition of the inflammatory response and activation of various hepatoprotective subcellular cascades[13].
In this review, we focus on clinical application of both, direct and remote, ischemic conditioning methods in hepatic surgery in humans.In the discussed papers we highlight clinical endpoints related to mortality, morbidity, intensive care unit (ICU) stay, hospital stay or intraoperative blood loss (in case of parenchymal resection).Postulated mechanisms of hepatocellular protection diminishing IRI are detailed in the referenced studies.
Hepatic steatosis has been associated with worse outcomes in liver surgery, and it is hypothesized that this is caused by a lower tolerance of steatotic livers to IRI[14,15].Therefore special emphasis is put on outcomes achieved in patients undergoing liver resection and liver transplantation in humans with steatotic livers.
DIRECT IPC IN LIVER RESECTION
In 2000, Clavienet al[16] published the first non-randomized study on IPC in human liver[16].Patients were subjected to IPC consisting of 10 min of clamping of the portal triad (Pringle maneuver) followed by 10 min of reperfusion before anatomical left or right hemihepatectomy.Liver cirrhosis, wedge or segmental resections were considered as exclusion criteria.The authors observed lower serum aminotransferase activities and reduced endothelial cell injury in the IPC group.No differences in mortality, hospital stay or blood loss were detected.These findings were followed by another study by Clavienet al[17].In the randomized controlled trial (RCT), they confirmed previous results and highlighted younger patients and those with liver steatosis as subgroups who derived the most benefits from IPC.Nevertheless, no differences in mortality, hospital stay or blood loss were found.These promising results were followed by a number of studies exploring this field.

Figure 1 Summary of liver ischemia-reperfusion injury mechanisms and pathways of ischemic preconditioning interventions.
Cochrane meta-analysis included four RCTs published until 2008[18].It assessed IPC followed by continuous clamping (CC) of the portal triad (135 patients) compared with CC alone (136 patients).All the included trials excluded liver resections performed in cirrhotic patients.IPC was achieved by 10 min of clamping followed by 10 min of unclamping, followed by CC in three trials[17,19-21].In the fourth trial, the duration of initial clamping is likely to be 10 min, although it was not clearly stated.This was followed by 10 min of unclamping followed by CC[22].The proportion of patients requiring blood transfusion was significantly lower in the IPC group, with no differences in mortality, posthepatectomy liver failure, morbidity, hospital stay or operative time.
Another meta-analysis, conducted by O’Neillet al[23], was published in 2013[23].It comprised all the aforementioned studies and seven RCTs not included in the Cochrane Hepato-Biliary Group study, of which only one included patients with liver cirrhosis[24].Ten minutes of the Pringle maneuver for IPC with 10 min of reperfusion was the most frequent strategy.In one study, IPC lasted 5 min with 5 min of reperfusion[24] and in another, IPC lasted 10 min with 15 min of reperfusion[25].CC was used for parenchymal transection in seven studies[17,20-22,24-26], whereas intermittent clamping was used in the remaining four[27-30].Eight studies that reported blood loss during liver resection found it to be nonsignificantly lower in the IPC group both in intermittent and CC.No differences in mortality, posthepatectomy liver failure, morbidity, operating time, hospital stay, prothrombin time, bilirubin concentration, aspartate aminotransferase (AST) or alanine aminotransferase (ALT) activities were detected (with and without patients with cirrhosis).
Another meta-analysis was published in 2017[31].The authors focused only on RCTs investigating the role of IPC before CC.Pooled data were analyzed by combining the results of the 13 RCTs.Five trials enrolled both cirrhotic and noncirrhotic patients (91 in the IPC group and 90 in the control group)[21,32-35].In three trials, IPC was performed through 5 min of inflow occlusion followed by 5 min of reperfusion[32,34,35].In one study, IPC was done by inflow occlusion for 10 min followed by reperfusion for 15 min before CC[25].Ten minutes of the Pringle maneuver for IPC with 10 min of reperfusion was used in nine studies[17,19,22,27-30].In the case of underlying cirrhosis, IPC reduced postoperative morbidity.However, in patients without cirrhosis, the analysis revealed no significant association between IPC and postoperative morbidity.There were also no differences in morbidity considering ischemia-reperfusion timing (10 + 10vs5 + 5).Mortality, operative time, total bilirubin concentration, AST or ALT concentration after postoperative day 1, and hospital and ICU stay were similar regardless of IPC.
Three studies focused on patients with steatotic livers in subgroup analyses.Two studies were RCTs[17,25], and one was a prospective nonrandomized study[16].A total of 29 patients were analyzed as a subgroup (16 in IPC group and 13 in control group).Cutoff for liver steatosis was set as ≥ 30%, but the type of steatosis (micro- or macrovesicular) was not described.The protocol of IPC was 10 + 10 min in two studies[16,17] and 10 + 15 min in one study[25].Only peak AST levels were measured as an endpoint in this subgroup comparison.IPC was associated with lower activity of AST after resections in steatotic livers[16,17,25], yet no results on clinical outcomes were provided.
In conclusion, there is currently no evidence supporting direct IPC as a protective strategy against mortality in patients undergoing liver resection, although it may be beneficial for patients with liver cirrhosis with respect to postoperative morbidity.Further investigation of applicability of direct IPC in cirrhotic and steatotic livers is warranted.
DIRECT IPC IN LIVER TRANSPLANTATION
In 2016, a meta-analysis on IPC in liver transplantation was published by Robertsonet al[36].Data from ten studies were analyzed (286 patients in IPC group and 307 patients in control group), four nonrandomized[37-40] and six RCTs[41-46].Only transplantations of grafts procured from donors after brain death were included in these studies, and no grafts underwent machine perfusion.Grafts were preconditioned in the donor by portal triad clamping for 10 min in all but one study.In one study, IPC lasted for 5 min[46].Time of reperfusion varied among studies from 10 to 39 min.Authors reported that IPC was associated with lower postoperative mortality, lower incidence of primary graft nonfunction and lower rate of retransplantation.None of these findings were statistically significant.Additionally, AST activity on the third postoperative day, length of ICU stay, length of hospital stay and incidence of acute rejection were all nonsignificantly lower in transplantations with IPC.
In living related liver transplantation, two prospective nonrandomized studies were published[47,48].The protocol of IPC was 10 + 10 min in both studies.Only right lobes were procured from the donors (32 in IPC group and 32 in control group).There were no differences in graft survival, patient survival, morbidity, hospital stay, histological findings and liver function tests between recipients of IPC and non-IPC liver grafts.
Three studies focused on patients with steatotic donor livers in subgroup analyses.All donors were after brain death (25 in IPC group and 29 in control group).Two studies were RCTs[43,46], and one was a retrospective study[39].The protocol of IPC was 10 + 10 min in one study[39], 10 + 30 min in second study[43], and in the remaining study IPC lasted for 5 min with ongoing reperfusion[46].Definitions of significant steatosis varied among studies and comprised presence of any steatosis[39], > 15% of macrovesicular steatosis[43] and no specific definition[46].None of the studies reported results on patient mortality.Clear conclusions cannot be drawn from these studies in terms of impact of IPC on steatotic liver grafts.Morbidity, graft survival, hospital stay, ICU stay and liver function tests seemed to be similar between IPC and non-IPC groups.However, there was a lack of uniform description of severity of hepatic steatosis, and the analyses were limited by small numbers.
In conclusion, there is currently no evidence that direct IPC decreases mortality after deceased and living donor liver transplantation.However, no trial provided data on recipient outcomes after more than 1 year postoperatively, and as such, the long-term effect of IPC on post-transplant outcomes remains to be elucidated.Also, there is insufficient data on IPC impact on steatotic grafts.Therefore, further analysis of this subgroup is warranted.
REMOTE IPC IN LIVER RESECTION
Only scarce data on remote IPC in liver resection in humans are available (Table 1).In five studies, the total number of 155 patients underwent RIPC with 160 patients serving as controls.Two studies had a third arm, direct IPC, including a total 52 patients.In two studies, liver resection was performed due to colorectal metastases[49,50] and due to primary liver cancers in the others[51-53].The most common protocol for ischemia-reperfusion was 5 min of upper limb ischemia followed by 5 min of reperfusion in 3 cycles in three studies[50,52,53] and 4 cycles in one study[51].In the first published pilot randomized feasibility trial, authors applied 2 cycles of 10 min of the lower limb ischemia followed by 10 min of reperfusion[49].Primary endpoints varied, with serum transaminase activities being the most common.Two studies found significant differences in the early postoperative ALT and AST activities in favor of RIPC[49] and IPC/RIPC over control[50].In one study, significant differences in postoperative ALT and AST activities on days 1 and 3 in favor of ischemia group (either remote or direct) over control group were observed, but these were absent on postoperative day 7[53].Analysis of the subgroup of patients with liver cirrhosis was performed in a single study pointing towards no effect of RIPC on ALT activity 24 h posthepatectomy[51].Mortality, morbidity, blood loss and hospital stay were assessed in three trials, and no differences were found between groups[49,51,52].
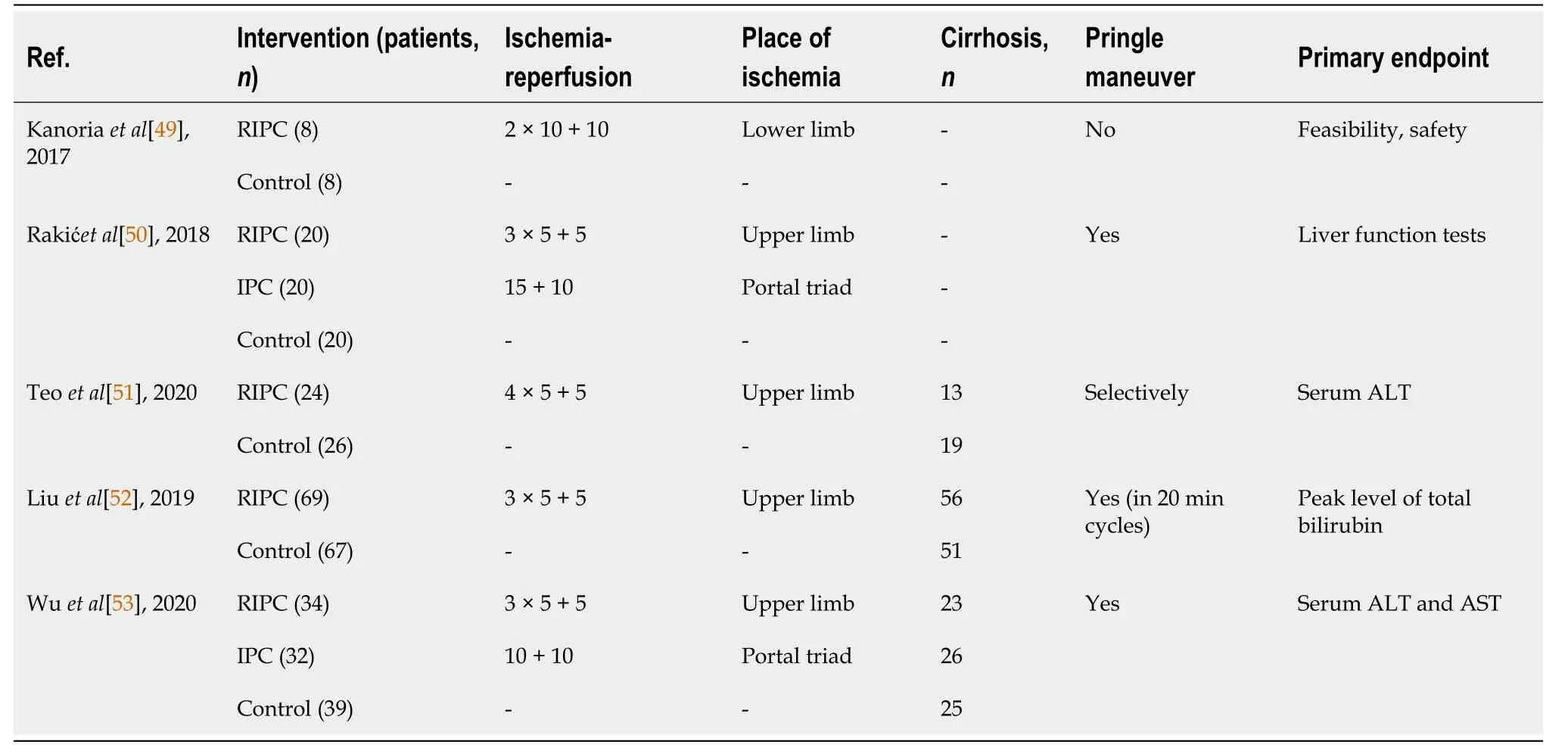
Table 1 Randomized controlled trials on remote ischemic preconditioning in liver surgery
Data on hepatic steatosis were provided in only two studies.In one trial, all specimens were evaluated for degree of steatosis[49], with minimal liver steatosis found in both groups.In the second study, etiology of liver cirrhosis was nonalcoholic fatty liver disease in 4 patients (2 in the study group and 2 in the control group)[51].No further information was given.
In conclusion, there is still insufficient data supporting the use of RIPC in liver resection as protection against IRI in order to improve clinical outcomes.
REMOTE IPC IN LIVER TRANSPLANTATION
To the authors knowledge, only two studies addressed remote IPC in liver transplantation.In 2017, Robertsonet al[54] published a pilot randomized controlled feasibility study on orthotopic liver transplantation from deceased donors (after either brain or cardiac death)[54].Forty patients were randomized to a sham control group (20 patients) or an RIPC group (20 patients).The protocol for ischemia-reperfusion was 5 min of donor lower limb ischemia followed by 5 min of reperfusion in three cycles.Implantation of the liver graft was performed by standard piggy-back and caval replacement techniques.No differences in 90-d mortality, 90-d graft loss, complications, AST activity on the third postoperative day and hospital and ICU stay were detected.
In 2020, Junget al[55] published an RCT on the application of RIPC in living donor liver transplantation[55].In total, 148 donors were randomized to a sham control group (73 donors) or an RIPC group (75 donors).The protocol for ischemiareperfusion was 5 min of donor upper limb ischemia followed by 5 min of reperfusion in 3 cycles.For the recipients, the medical records were retrospectively analyzed.In the donors, no differences in complications, AST, ALT, total bilirubin and international normalized ratio within 7 postoperative days, incidence of delayed recovery of hepatic function and liver regeneration index depending on the use of RIPC were found.However, recipients who received preconditioned grafts had lower AST activity on postoperative day 7 and the maximal AST activity during the first postoperative week.No differences in other laboratory variables, early graft dysfunction, acute kidney injury, graft failure after 12 mo post-transplantation or hospital and ICU stay were detected.
In conclusion, there is no evidence supporting the use of RIPC in deceased and living donor liver transplantations as protection against IRI in order to improve clinical outcomes.
REMOTE ISCHEMIC PERCONDITIONING, ISCHEMIC POSTCONDITIONING AND COMBINED METHODS OF ISCHEMIC CONDITIONING IN LIVER SURGERY
In search of effective protection against liver IRI, novel concepts are being adapted from experience with other organs.Ischemic postconditioning (IPOS) applies brief episodes of ischemia at the onset of reperfusion following a prolonged ischemia and was first introduced in a rodent heart model[56].Advantage of IPOS over IPC is that it can be easily applied with precisely controlled timing.Modification of the RIPC technique is RIPer, first applied by Schmidtet al[7] in the context of myocardial ischemia[7].In a porcine model, alternating periods of occlusion and perfusion of the limb while the myocardium was under ischemia was examined.Little data exists on the efficacy of these methods alone or in combination in hepatoprotection against IRI.
In 2012, a mice liver resection study by Songet al[57] compared IPC, RIPC (hind limb), IPOS and the combination of IPC with IPOS[57].The authors found that the combination of direct IPC with IPOS offered additional protection over the solo treatment.In contrast, no additive protection of IPOS was found when applied with RIPer in rat liver resection model[58].In this study, the authors identified RIPer as the most promising technique to avoid hepatic IRI, in comparison with IPOS and combination of RIPer with IPOS.This was in accordance with other studies on rodent liver resection or transplantation, which confirmed a protective effect of RIPer against IRI[59-61].Combination of different ischemic conditioning techniques in a mouse liver transplantation model was reported by Liet al[62].By comparing IPC and RIPC with a combination of both methods, they found both techniques effective in hepatic IRI protection but no synergistic and additive effect of IPC and RIPC.Another study designed by this group assigned mice to direct IPC (donor), RIPer (recipients) and IPC + RIPer (donors and recipients were subjected to IPC and RIPer, respectively)[63].By double protection of the graft, first by IPC in donor then by RIPer before reperfusion in recipient, they showed that combined treatment brought enhanced attenuation in IRI through additive effects on antioxidation, antiapoptosis, modulation of microcirculation disturbance and inhibition of innate immune response.
The aforementioned protocols have only been tested in animal models.No studies on humans have been published researching the possible application of IPOS, RIPer or combined ischemic conditioning.There are currently no ongoing clinical trials on that subject[64].
CONCLUSION
Direct IPC was not found effective in terms of decreasing mortality after liver resection or transplantation.Its role in specific subgroups of patients remains to be elucidated.Studies on remote IPC in liver resection pointed toward either no beneficial effects or effects limited to moderate reduction of IRI as indicated by serum transaminases and bilirubin concentration.Most studies used protocols with 5 min ischemic periods, which may indicate that this is an insufficient period.
In terms of liver transplantation, RIPC was found to be beneficial only in early graft function from living donors.Those were young, nonsteatotic grafts with relatively short periods of cold and warm ischemia.Other techniques of ischemic conditioning are yet to be assessed in human clinical trials.
 World Journal of Hepatology2021年5期
World Journal of Hepatology2021年5期
- World Journal of Hepatology的其它文章
- COVID-19 and the liver: What do we know so far?
- Bile acid indices as biomarkers for liver diseases II: The bile acid score survival prognostic model
- Gut dysbiosis is associated with poorer long-term prognosis in cirrhosis
- Combination of type IV collagen 7S, albumin concentrations, and platelet count predicts prognosis of non-alcoholic fatty liver disease
- Surgical treatment outcomes of primary hepatic sarcomas: A singlecenter experience
- Endoscopic retrograde cholangiopancreatography drainage for palliation of malignant hilar biliary obstruction — stent-in-stent or side-by-side? A systematic review and meta-analysis
