The evolution of minimally invasive surgery in liver transplantation for hepatocellular carcinoma
Georgios S. Sioutas, Georgios Tsoulfas
1School of Medicine, Democritus University of Thrace, Alexandroupolis 68100, Greece.
2First Department of Surgery, Papageorgiou University Hospital, Aristotle University of Thessaloniki, Thessaloniki 54622,Greece.
Abstract Hepatocellular carcinoma (HCC) is a malignant neoplasm associated with significant mortality worldwide. The most commonly applied curative options include liver resection and liver transplantation (LT). Advances in technology have led to the broader implementation of minimally invasive approaches for liver surgery, including laparoscopic, hybrid, hand-assisted, and robotic techniques. Laparoscopic liver resection for HCC or living donor hepatectomy in LT for HCC are considered to be feasible and safe. Furthermore, the combination of laparoscopy and LT is a recent impressive and promising achievement that requires further investigation. This review aims to describe the role of minimally invasive surgery techniques utilized in LT for HCC.
Keywords: Minimally invasive surgery, liver transplantation, laparoscopic hepatectomy, laparoscopic donor hepatectomy
INTRODUCTION
Hepatocellular carcinoma (HCC) is a malignant neoplasm, typically arising in the setting of cirrhosis and chronic liver disease[1]. Globally, HCC leads to approximately 800,000 deaths every year[2], being the fifth most common malignant neoplasm and the third cause of death related to cancer worldwide[3]. It is usually diagnosed in advanced stages, with a median survival after diagnosis of 6-20 months[4]. Although locoregional therapy may lead to cure for small lesions in selected patients, complete surgical resection is the most commonly implemented curative option for patients diagnosed with HCC limited to the liver, with preserved liver function, and without portal hypertension.
Laparoscopy can be used to diagnose, stage, and treat HCC[5]. According to the Louisville Statement (2008),the indications for laparoscopic liver resection (LLR) should be: solitary lesions ≤ 5 cm in diameter, in segments 2-6; laparoscopic left lateral sectionectomy should be standard practice; and major liver resections should be performed by experienced surgeons[5]. In 2014, the Second International Consensus Conference on Laparoscopic Liver Resection was held in Morioka, Japan, to establish further guidelines[6]. The experts concluded that LLR is not inferior in terms of overall survival, mortality, negative margins, and cost compared to the open approach, while they also concluded that it is probably superior regarding length of hospital stay and intraoperative transfusions[6].
However, only approximately 15% of patients present with resectable tumors[7]. Since liver transplantation(LT) was established as the optimal treatment for end‐stage liver disease, its indications have expanded to include non-metastatic unresectable HCC (Milan criteria)[8,9]. Actually, among well-selected patients undergoing LT for HCC, the overall survival was found to be comparable to that of LT for non-malignant etiology[10,11]. Following resection, HCC patients may exhibit a recurrence rate of 40%-90%, especially in the case of underlying chronic liver disease, and in certain cases salvage LT can be a reasonable option[5,9,12]. As LT may be more complicated in the case of adhesions after previous abdominal surgery[13], LLR may have an additional advantage over its open counterpart in that scenario[14].
Considering the benefits of laparoscopic approaches and the curative potential of LT, we aim to review the role of minimally invasive surgery in LT for HCC.
LAPAROSCOPIC LIVER RESECTION FOR HEPATOCELLULAR CARCINOMA
Technique and positioning for laparoscopic liver resection
The most common position for the patient is the supine one[15]. The trocar for the laparoscope is inserted through an umbilical incision, while four additional trocars are usually used: at the epigastrium, abdomen bilaterally, and at the right hypochondrium[15,16]. Transthoracic or intercostal trocars are used when operating on the superior part of the liver[17]. Notably, single-incision LLR has also been described[18]. The Pringle maneuver is used to control intraoperative bleeding, and selective inflow occlusion is used to avoid ischemia-reperfusion injury during anatomical major LLR[19]. To reduce intraoperative bleeding, a low central venous and airway pressure should be maintained[15]. In addition, pneumoperitoneum should be ideally kept to 8-10 mmHg to reduce the risk of gas embolism[15].
Apart from the standard method, hybrid or hand-assisted liver resection may also be used in challenging cases[20]. Additionally, technological advancement has led to the incorporation of the surgical robot in liver surgery. Robotic liver resection (RLR) has the advantage of more technically precise surgery because of its more flexible instrumentation and the 3D visualization of the operative field[21-23].
Short-term outcomes
The international consensus statement conclusions have been further validated by several systematic reviews and meta-analyses comparing LLR with open liver resection for patients with HCC. According to a recent one by Wanget al.[24], major LLR has the benefits of fewer postoperative complications, less blood loss, and shorter hospital length of stay with the potential drawback of longer operative time[24]. Long-term outcomes were comparable[24]. Another meta-analysis showed that LLR can lead to decreased intraoperative blood loss, need for transfusion, 30-day complication and mortality rate, and length of hospital stay[25].
According to the authors, LLR is a logical option even for recurrent HCC, with better short-term postoperative outcomes than the open approach[26]. Hybrid hepatectomy for HCC has also been associated with shorter length of hospital stay, same survival rates, and longer operation time when compared with open hepatectomy[27].
A study by Chenet al.[28]showed that RLR for HCC is a feasible option for challenging major hepatectomies in cirrhotic patients. When compared to the open procedure, it resulted in shorter hospital stay, less postoperative pain, and similar survival outcomes, but longer operation time[28]. When compared with the open or the laparoscopic approach, it was found to be comparable in terms of margin-free resection rates[29]. Overall, LLR and RLR are considered to be equivalent in terms of safety and effectiveness for the management of liver neoplasms[30].
ROLE OF MINIMALLY INVASIVE LIVING DONOR HEPATECTOMY FOR LIVER TRANSPLANTATION
Technical details and learning curve of laparoscopic living donor hepatectomy
Living donor LT was first reported in 1990[31,32]. The first laparoscopic donor hepatectomy in 2002 was a left lateral donor segmentectomy (LLDS) for a pediatric recipient[33]. Further minimal invasive surgical approaches have since been described[34].
During laparoscopic donor hepatectomy, the Pringle maneuver is typically utilized to allow less blood loss in donors without affecting liver function[35]. For parenchymal transection, the high-pressure waterjet system or the ultrasonic surgical aspirator are used[36]. For hepatic and portal vein occlusion and division,surgical staplers are used. For the hepatic artery and the bile duct, Hem-o-lok clips are used to avoid shortening of vessel length[37]. Because precise bile duct transection is important, intraoperative cholangiography or indocyanine-green fluorescence cholangiography is often used[38]. After resection, the graft is retrieved through a Pfannenstiel incision in an endo-bag. The retrieval should be careful to avoid graft injury[39]. Furthermore, several innovations have been implemented for minimally invasive donor hepatectomy, either preoperatively (i.e., 3D imaging[40]and 3D printing[41]) or intraoperatively (i.e., surgical robot[42]).
Donor hepatectomy is technically demanding. In particular, the learning curve for pure laparoscopic LLDS is 25 cases[43], while the more difficult right donor hepatectomy requires approximately 60 cases[44,45].However, these numbers depend on other factors, such as prior experience on both open donor hepatectomy and minimally invasive surgery in general.
Types and benefits of minimally invasive living donor hepatectomy
According to a recent systematic review, open donor hepatectomy is superior to the laparoscopic approach in terms of hilar and parenchymal dissection and ischemic time. However, the laparoscopic approach has a superior cosmetic effect[39].
Pure laparoscopic left and right hepatectomy for adult recipients
To choose between left or right donor hepatectomy, the surgeon has to consider the size of the recipient to avoid small-for-size syndrome[46]. Pure laparoscopic donor left and right hepatectomies for adult recipients were first reported in 2013[47-50]. These procedures are complex and require a high level of surgical expertise.Despite this, some experienced teams have published successful reports with laparoscopic living donor hepatectomy[51-55]. Some experts support the use of right donor hepatectomy without specific selection criteria[38], while others have developed such criteria incorporating vascular anatomy and graft weight[56,57].
Several studies have described successful pure laparoscopic right hepatectomy for donors with variations in bile ducts[53,58,59], while anatomical reasons have been associated with high complication rates[45,60].Laparoscopic right donor hepatectomy has been associated with a similar complication rate and shorter length of hospital stay compared to the open approach[45,60]. Suhet al.[38]showed that complication rates,hospital stay, and re-hospitalization were similar between donors undergoing either pure laparoscopic or open right donor hepatectomy.
Right donor hepatectomy may be preferred for yielding a larger graft, yet studies have shown that laparoscopic left donor hepatectomy is also feasible[49]. Samsteinet al.[61]compared laparoscopic to open or hybrid left donor hepatectomy. While the laparoscopic group required a longer time for graft procurement,it was associated with decreased blood loss, shorter hospital stay, and fewer days away from work. The oneyear survival rates were similar between the two groups[61].
Pure laparoscopic left lateral donor sectionectomy for pediatric recipients
Laparoscopic LLDS is considered to be a safe alternative to the open approach. This method has been advocated to become the new standard of care for LLDS for pediatric recipients[57]. It has the benefit of acceptable recipient outcomes, less intraoperative bleeding, a shorter length of hospital stay, no wound complications, and similar biliary and vascular complications with the open approach, again with the potential drawback of long operative time[61-66]. Soubraneet al.[67]compared laparoscopic liver with kidney donors and found that, while liver donors had longer hospital stay and operation times, LLDS resulted in fewer minor complications[67].
Hand-assisted and hybrid donor hepatectomy
Hand-assisted or hybrid donor hepatectomy has the same principles as pure laparoscopic donor hepatectomy, but the hepatic hilum is dissected and the liver is transected through a small open upper midline or transverse incision[34,68]. Similarly, the muscle layer is not interrupted, and, as a result, patients feel less abdominal wall pain than with the open hepatectomy[69]. However, the small incision of these techniques has drawbacks for obese patients with deep body cavities, such as longer operative duration,postoperative complications, and longer hospital stay, as it is difficult for surgeons to manage vascular injuries in these deeper areas[68,70,71]. Recent meta-analyses associated laparoscopic-assisted hepatectomy with fewer complications, less blood loss and pain, no mortality, faster recovery, better cosmetic result, and longer operation time[70,72]. In other words, laparoscopic-assisted hepatectomy is a safe and feasible alternative to open hepatectomy for well-selected donors when performed by experienced teams[73]and can be gradually adopted by less-experienced groups[74,75]. In fact, hand-assisted or hybrid donor hepatectomy can be used by surgeons when transitioning from open to pure laparoscopic donor hepatectomy, because of the steep learning curve of the latter[76].
Robotic donor hepatectomy
The first robotic donor hepatectomy was a right hepatectomy reported by Giulianottiet al.[40]in 2012, and since then it has been implemented by several centers[40,77-79]. This technique offers the benefits of 3D vision,a stable and magnified field, and improved instrument precision compared to the laparoscopic technique.This helps the biliary and vascular dissection, and the decision of the point of transection, while the improved ability for suture ligation of venous bleeders can be helpful in minimizing blood loss[40]. The first series of 13 robotic right donor hepatectomies was published by Chenet al.[77]in 2016. The robotic group required no open conversion, the postoperative recovery was quicker, and the need for analgesics was decreased. Compared to the open group, the robotic one showed comparable results for complication rates,blood loss, and recovery of donor liver function. However, the robotic group had longer operation time, and one donor had bile leakage after discharge[77]. While some studies have shown the safety of robotic donor hepatectomy, they have not yet reported superiority in efficacy when compared to open and laparoscopic approaches[80,81]. A recent systematic review supports that the robotic approach is more beneficial regarding hilar dissection, while the laparoscopic is more beneficial for parenchymal dissection with no major difference in terms of ischemic time or cosmesis[39]. In 2018, the international consensus statement on RLR recommended that robotic donor hepatectomy can be an alternative option when performed by experienced surgeons[82].
Laparoscopic living donor hepatectomy for recipients with hepatocellular carcinoma
Leeet al.[45]compared pure laparoscopicvs. open donor right hepatectomy for living donor LT. The authors reported data from 115 donors and recipients, with HCC being the indication for LT in 67.8% of the patients. The study concluded that pure laparoscopic donor right hepatectomy is safe when performed by an experienced team[45]. A year later, Leeet al.[83]conducted a similar study of 33 donors and recipients, with HCC being the indication for LT in 21.2% of the patients. The incidence of postoperative complications among donors was similar between the open and laparoscopic groups, while the two approaches yielded similar results for most perioperative outcomes[83]. Further details about these two studies are shown in Table 1[45,83].
LAPAROSCOPIC-ASSISTED LIVER TRANSPLANTATION
Nine cases of living donor LT with hand-assisted laparoscopic surgery were first reported in 2011 by Eguchiet al.[84]. The hand-assisted laparoscopic total hepatectomy was performed with an upper midline incision. Explantation and liver graft implantation were performed with an open approach after extending the incision[84]. In 2015, 29 selected cases of hybrid procedure for living donor LT were reported[85]. Liver recipients treated with the hybrid approach had no significant differences in blood loss, duration of surgery,vascular anastomosis, and survival, compared to those treated with the conventional open procedure[85].Dokmaket al.[86]in 2020 published a hybrid LT case for neuroendocrine liver metastases with laparoscopic total hepatectomy and liver graft implantation through a preexisting incision. They showed that the laparoscopic approach for LT recipients may be safe and reasonable[86]. Details from these studies are summarized in Table 2[84-86]. That growing body of evidence, even in patients with cancer, suggests that the use of laparoscopy either for the donor or the recipient in LT for HCC will pave the way for further advancements in the field of minimally invasive surgery and its introduction in the field of LT.
CONCLUSION
The use of minimally invasive surgical approaches for LT appears to be feasible. Such approaches may be beneficial even for patients with recurrent HCC after resection requiring salvage LT. Regarding LLDS,laparoscopy is advocated to become the gold standard. Regarding living donor hepatectomy or LT itself,minimally invasive or hybrid laparoscopic approaches have been described. However, laparoscopic or even robotic donor hepatectomy is still rarely performed and only by experienced teams, and thus the need for an international registry or multicenter studies is apparent. In the future, the ongoing improvements in technology will probably further expand this rising surgical field.

Table 1. Studies about pure laparoscopic donor hepatectomy for recipients with hepatocellular carcinoma
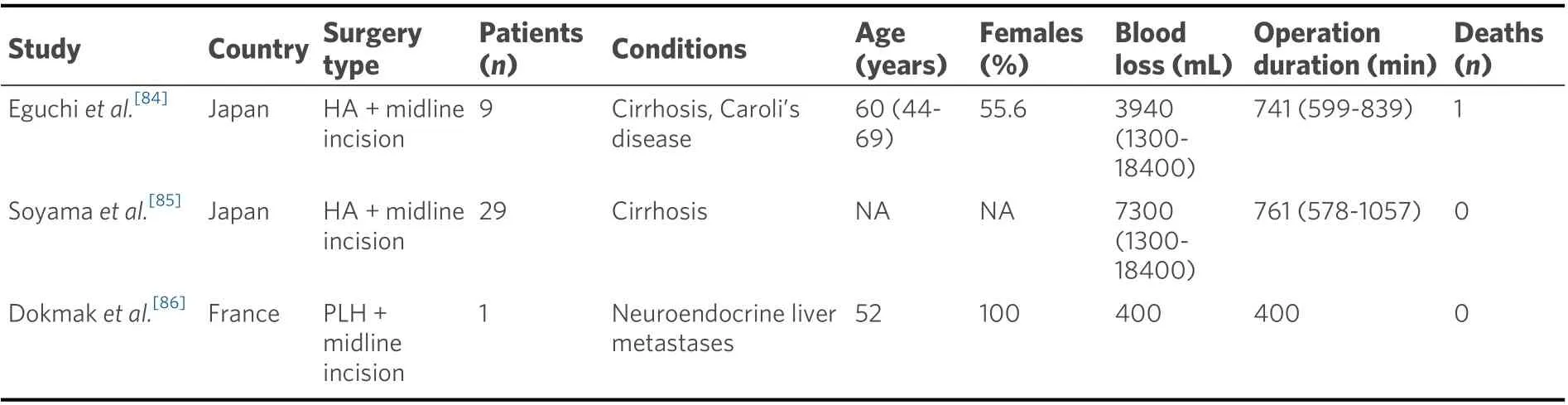
Table 2. Studies on laparoscopic-assisted liver transplantation
DECLARATIONS
Authors’ contributions
Study concept, data analysis and interpretation, critical revision of the manuscript, final approval of the manuscript: Sioutas GS, Tsoulfas G
Data acquisition, drafting of the manuscript: Sioutas GS
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
Both authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2021.
- Hepatoma Research的其它文章
- Laparoscopic isolated caudate lobectomy for HCC
- Coffee and hepatocellular carcinoma: epidemiologic evidence and biologic mechanisms
- Mechanisms of protective effects of astaxanthin in nonalcoholic fatty liver disease
- Prospects for a better diagnosis and prognosis of NAFLD: a pathoIogist's view
- Systematic review of existing guidelines for NAFLD assessment
- The narrow ridge from liver damage to hepatocarcinogenesis