Predictive risk factors for recollapse of cemented vertebrae after percutaneous vertebroplasty: A meta-analysis
Yi-Hang Ma, Zhi-Sen Tian, Hao-Chuan Liu, Bo-Yin Zhang, Yu-Hang Zhu, Chun-Yang Meng, Xiang-Ji Liu,Qing-San Zhu
Yi-Hang Ma, Zhi-Sen Tian, Hao-Chuan Liu, Bo-Yin Zhang, Yu-Hang Zhu, Chun-Yang Meng, Xiang-Ji Liu, Qing-San Zhu, Department of Spine Surgery, China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China
Abstract BACKGROUND As one of the most common complications of osteoporosis, osteoporotic vertebral compression fracture (OVCF) increases the risk of disability and mortality in elderly patients. Percutaneous vertebroplasty (PVP) is considered to be an effective, safe, and minimally invasive treatment for OVCFs. The recollapse of cemented vertebrae is one of the serious complications of PVP. However, the risk factors associated with recollapse after PVP remain controversial.AIM To identify risk factors for the recollapse of cemented vertebrae after PVP in patients with OVCFs.METHODS A systematic search in EMBASE, MEDLINE, the Cochrane Library, and PubMed was conducted for relevant studies from inception until March 2020. Studies investigating risk factors for the recollapse of cemented vertebrae after PVP without additional trauma were selected for analysis. Odds ratios (ORs) or standardized mean differences with 95% confidence interval (CI) were calculated and heterogeneity was assessed by both the chi-squared test and the I-squared test. The methodological quality of the included studies was assessed according to the Newcastle-Ottawa Scale.RESULTS A total of nine case-control studies were included in our meta-analysis comprising 300 cases and 2674 controls. The significant risk factors for the recollapse of cemented vertebrae after PVP in OVCF patients were fractures located at the thoracolumbar junction (OR = 2.09; 95%CI: 1.30 to 3.38; P = 0.002), preoperative intravertebral cleft (OR = 2.97; 95%CI: 1.93 to 4.57; P < 0.00001), and solid lump distribution pattern of the cement (OR = 3.11; 95%CI: 1.91 to 5.07; P < 0.00001).The analysis did not support that age, gender, lumbar bone mineral density,preoperative visual analogue scale score, injected cement volume, intradiscal cement leakage, or vertebral height restoration could increase the risk for cemented vertebra recollapse after PVP in OVCFs.CONCLUSION This meta-analysis suggests that thoracolumbar junction fractures, preoperative intravertebral cleft, and solid lump cement distribution pattern are associated with the recollapse of cemented vertebrae after PVP in OVCF patients.
Key Words: Vertebroplasty; Osteoporotic vertebral compression fracture; Risk factors;Recollapse; Cemented vertebrae; Meta-analysis
INTRODUCTION
Osteoporosis is characterized by reduced bone mass and bone microstructure degeneration. The immediate consequence of osteoporosis is the occurrence of osteoporotic fractures, especially in areas where cancellous bone is abundant such as the vertebra and hip[1]. An osteoporotic vertebral compression fracture (OVCF) is one of the most common complications of osteoporosis. As the global population ages, the absolute number of elderly patients and the incidence of OVCF are increasing[2].OVCFs can not only cause pain and kyphosis, compromising the quality of life, but also increase the risk of disability and mortality to some extent[3]. As a minimally invasive technique for treating OVCFs, percutaneous vertebroplasty (PVP) involves inserting a needle under radiation control and injecting bone cement into the fractured vertebra, and this procedure has been widely used due to its good therapeutic efficacy[4]. Even so, several studies[5-7]have reported the recollapse of cemented vertebrae during follow-up with no additional trauma, leading to a decrease in vertebral height and aggravation of kyphosis. Recollapse is regarded as an insufficiency fracture of the treated vertebra, which can be assessed through medical history, clinical symptoms, and imaging findings. When the treated patient reappears with intractable back pain or neurological symptoms, combined with severe kyphosis in imaging finding, it should be required further treatments after excluding new injuries. Hence, we need to determine the predictive risk factors for the recollapse of cemented vertebrae after PVP in OVCFs.
In recent decades, many risk factors for the recollapse of cemented vertebrae have been reported in previous studies, and they can be summarized in three categories.The first is the physical condition of patients, which includes risk factors such as lumbar bone mineral density (BMD), body mass index (BMI), gender, and old age. The second is the classification of differences in the effects of trauma on individuals, which includes the local kyphotic angle, location of the fractured vertebra, occurrence of an intravertebral cleft (IVC), and fracture type. The third category represents risk factors related to the PVP procedure, such as the injected cement volume, the cement distribution pattern, intradiscal cement leakage, and vertebral height restoration(VHR). However, high-quality and large-scale studies concerning these risk factors are scarce. Most studies lacked sufficient sample sizes and did not evaluate each potential risk factor systematically.
As far as we could see from the literature, the predictive risk factors vary across studies, and no consensus on this problem has been reached. Based on this, a metaanalysis was conducted to pool all relevant published data for the first time to identify risk factors that might lead to the recollapse of cemented vertebrae after PVP.
MATERIALS AND METHODS
Search strategy
We searched electronic databases including the CENTRAL (Cochrane Central Register of Controlled Trials), MEDLINE, Excerpta Medica (EMBASE), and National Library of Medicine (PubMed) for original articles published up to March 2020. Medical subject heading terms [“vertebroplasty” (MeSH)] combined with the following free words were selected to perform searches using Boolean operators: “Percutaneous vertebroplasty”, “PVP”, “recollapse”, “recompression”, “refracture”, “recurrent fracture”, “subsequent fracture”, “height loss”, “height decrease”, “cemented vertebrae”, “augmented vertebrae”, “treated vertebrae”, and “same vertebrae”.Additionally, the citation lists of the retrieved articles and recent reviews were scanned to identify additional relevant studies. There were no limitations imposed regarding the language of the included articles.
Eligibility criteria
Studies were considered eligible for this meta-analysis if they met the following criteria: (1) Randomized controlled trials (RCTs) or cohort, cross-sectional, and casecontrol studies; (2) adult patients with a diagnosis of OVCF; (3) studies that must investigate risk factors for the recollapse of cemented vertebrae after PVP without additional trauma; (4) completion of at least 12 mo of follow-up; and (5) sufficient published data to estimate a standardized mean difference (SMD) or odds ratio (OR)with a 95% confidence interval (CI).
The exclusion criteria were as follows: (1) Case reports, letters, reviews, editorials,abstracts, or meeting proceedings; (2) studies without a clear description of the design;(3) studies lacking comparable results; and (4) repeated reports of previous studies.
Study selection and data extraction
The titles and abstracts of studies that were initially screened out were evaluated by two independent investigators (Ma YH and Zhu YH). After omitting the obviously unrelated studies, the full-texts of the potentially eligible studies were searched for final inclusion. Then, two investigators (Ma YH and Zhu YH) independently read the full-texts and extracted the available data from each study for analysis. The extracted data from all eligible studies included characteristics of the study (author, study design, year of publication, country of origin, study period, and all included variables)and demographics of the patients (sample size, mean age, gender ratio, incidence of recollapse, and follow-up duration). Data that could not be acquired directly from the texts were recalculated. Any disagreement was solved through discussion between two investigators (Ma YH and Zhu YH). If no consensus was reached, a senior author(Zhu QS) was consulted for a final decision.
Assessment of methodological quality
The methodological quality of the included studies was independently assessed by two investigators (Ma YH and Zhu YH) according to the Newcastle-Ottawa Scale(NOS)[8]. This scale concerning object selection, comparability, and exposure objectively evaluates the risk of bias. The maximum score of the scale is 9, and studies with a score ≥ 7 were considered high quality. Disagreements were resolved through consultation and discussion with a senior author (Zhu QS).
Statistical analysis
The software Review Manager Version 5.3 (The Cochrane Collaboration, Oxford,United Kingdom) was used for all statistical analyses. Pooling of the data was only conducted when at least three studies reported on the outcome of interest. We calculated SMDs for continuous variables and ORs for dichotomous variables, both with a 95%CI. Heterogeneity across studies was evaluated by chi-squared tests andIsquared (I2) statistics. If thePvalue was < 0.1 and theI2value was > 50%, the heterogeneity among studies was considered significant. When heterogeneity obviously existed, a random-effect model was used to calculate pooled ORs or SMDs[9]; otherwise, a fixed-effect model was applied. All results are summarized graphically using a forest plot. Since the number of included studies was less than 10,publication bias was not analyzed in this meta-analysis[10].
The statistical methods of this study were reviewed by Kou CG from the Department of Health Statistics, School of Public Health, Jilin University.
RESULTS
Study selection process
As shown in Figure 1, the database search of CENTRAL, MEDLINE, EMBASE, and PubMed yielded 158 studies, and another five studies were identified from the reference lists of previous reviews. A total of 82 studies remained after eliminating duplicates. Of these, 30 were discarded during the title and abstract review. A total of 43 studies were abandoned after reviewing the full-texts for the following reasons: The treatment in 19 studies included both percutaneous kyphoplasty (PKP) and PVP; 21 studies provided no outcomes of interest; and three studies lacked sufficient data.Ultimately, a total of nine studies[11-19]were included in the final meta-analysis.
Study characteristics and methodological quality
The basic characteristics of the nine studies[11-19]are presented in Table 1. All selected studies were case-control studies published between 2008 and 2018, and no RCTs were published on this subject. Of these studies, three were conducted in China[17-19], three in Taiwan[11,13,15], and three in Korea[12,14,16]. The sample sizes ranged from 44 to 1800, and together, the studies included a total of 2974 patients. Recollapse of cemented vertebrae after PVP occurred in 300 cases, and did not occur in 2674 cases. The recollapse rate in each study ranged from 0.6% to 63.3% and the pooled incidence was 10.1%. The mean follow-up duration for each study was no less than 12 mo.Additional details are shown in Table 1. Numerous potential risk factors were evaluated in the included studies; however, we only selected the risk factors reported in at least three studies. The potential risk factors for recollapse involved in all included studies are depicted in Table 2.
For the nine case-control studies, methodological quality was assessed in accordance with the NOS. Among them, one single study had a score of 9 points[13], six studies had a score of 8 points[11,12,15,17-19], and two studies had a score of 7 points[14,16].Therefore, all included studies could be regarded as relatively high quality, and the scoring results are listed in Table 1.
Risk factors involving the physical condition of patients
Three eligible factors concerning the physical condition of patients were selected for meta-analysis. Of these, age was evaluated as a predictive risk factor for the recollapse of cemented vertebrae after PVP in seven studies[11-14,17-19]containing 1130 patients. A fixed-effect model was used due to the heterogeneity test (χ2= 4.00;P= 0.68;I2= 0%).The results of age exhibited no significant differences between the recollapse group and the well-maintained group (SMD = 0.05; 95%CI: -0.10 to 0.20;P= 0.52) (Figure 2A).All the nine studies[11-19]assessed the potential effect of gender (female). Because of the low heterogeneity among the included studies, a fixed-effect model was utilized (χ2=8.28;P= 0.41;I2= 3%). The difference in gender did not reach statistical significance(OR = 0.88; 95%CI: 0.61 to 1.28;P= 0.51) (Figure 2B). A total of five studies[12,14,17-19]containing 951 patients recorded comparable results for lumbar BMD. The test for heterogeneity was significant (χ2= 8.02;P= 0.09;I2= 50%). Using a random-effect model, the aggregated results of the five studies showed that there were no significant differences between them (SMD = -0.23; 95%CI: -0.49 to 0.03;P= 0.09) (Figure 2C).
Risk factors involving differences in the effects of trauma on individuals
Three eligible factors concerning this aspect were selected for meta-analysis. With respect to the location of the fractured vertebra, five studies[11,13-15,19]consisting of 2191patients were pooled for this outcome by a fixed-effect model due to low heterogeneity(χ2= 3.56;P= 0.47;I2= 0%). The pooled results suggested that OVCFs located at the thoracolumbar junction (T10-L2) were associated with a significant increase in the incidence of the recollapse of cemented vertebrae after PVP (OR = 2.09; 95%CI: 1.30 to 3.38;P= 0.002) (Figure 2D). Five studies[11,13,14,16,19]consisting of 435 patients investigated the association between preoperative IVC and the risk of recollapse after PVP. A fixedeffect model was adopted as the studies had low heterogeneity (χ2= 2.41;P= 0.66;I2=0%). The aggregated results demonstrated a statistically significant difference between the two groups (OR = 2.97; 95%CI: 1.93 to 4.57;P< 0.00001) (Figure 2E). Data on preoperative visual analogue scale scores were available for analysis from three studies containing 436 patients[14,18,19], and the studies were considered heterogeneous (χ2= 6.21;P= 0.04;I2= 68%). Therefore, a random-effect model was applied to evaluate the effect. However, the results showed no significant differences between the recollapse group and the well-maintained group (SMD = 0.14; 95%CI: -0.27 to 0.56;P=0.50) (Figure 2F).
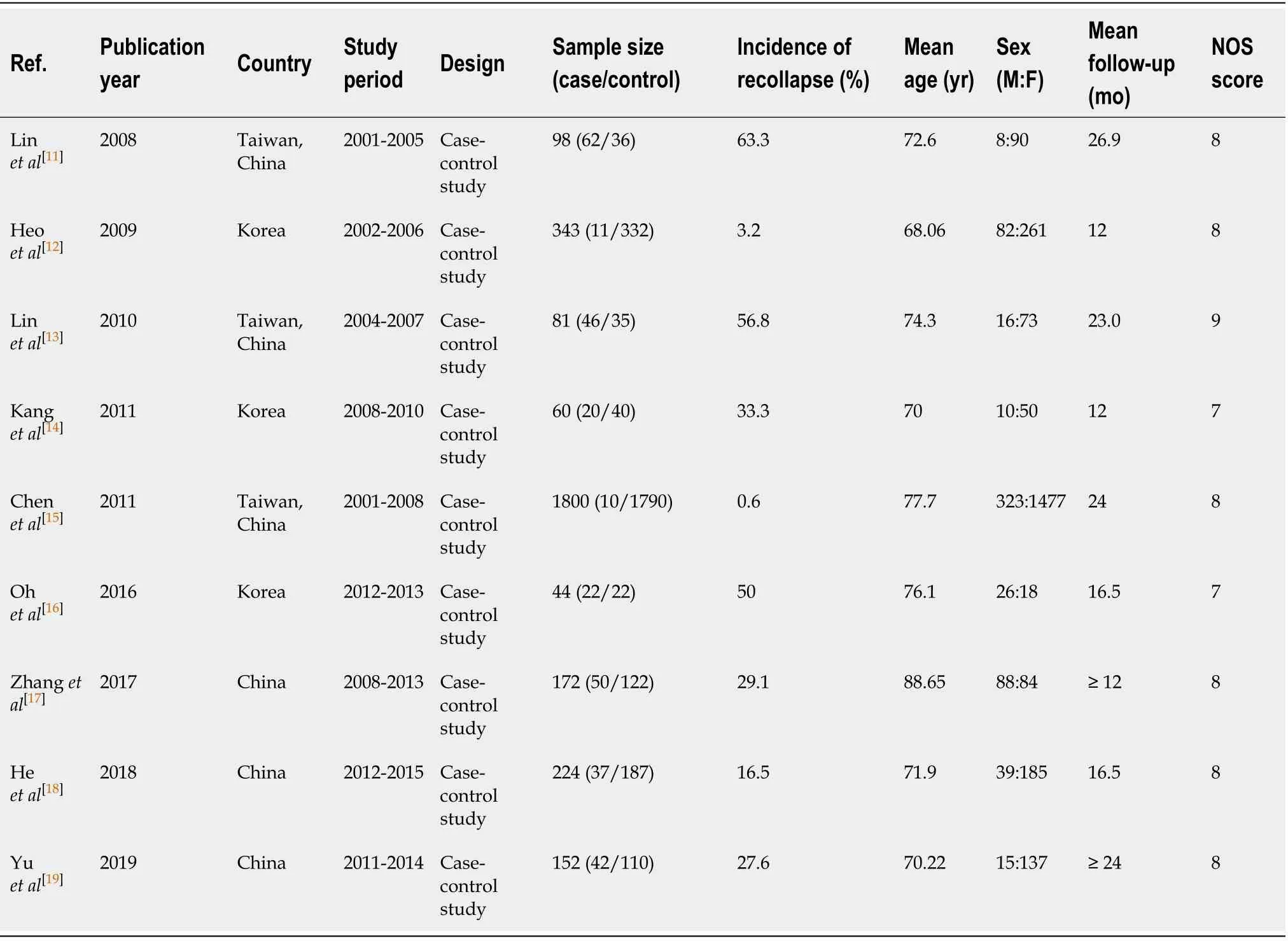
Table 1 Basic characteristics of the included studies
Risk factors involving the PVP procedure
Four eligible factors related to the PVP procedure were selected for meta-analysis. A total of seven[11-14,17-19]out of nine studies containing 1130 patients were pooled to analyze the effect of injected cement volume. The heterogeneity among the studies was high, so a random-effect model was used (χ2= 19.01;P= 0.004;I2= 68%). The results demonstrated that the injected cement volume was not associated with the recollapse of cemented vertebrae (SMD = 0.11; 95%CI: -0.18 to 0.39;P= 0.46) (Figure 2G). In a total of six studies[13-17,19]containing 2309 patients, the data of intradiscal cement leakage were evaluated. A fixed-effect model was employed because of the low heterogeneity (χ2= 3.65;P= 0.60;I2= 0%). Consequently, intradiscal cement leakage was not significantly different between the two groups (OR = 1.25; 95%CI: 0.76 to 2.05;P= 0.37) (Figure 2H). Regarding the cement distribution pattern, the data of 2236patients from four studies[14,15,18,19]were pooled in the analysis. A fixed-effect model was adopted as the heterogeneity among the included studies was relatively low (χ2= 3.52;P= 0.32;I2= 15%). The solid lump distribution pattern of the cement was associated with an increase in the risk of recollapse of cemented vertebrae (OR = 3.11; 95%CI: 1.91 to 5.07;P< 0.00001) (Figure 2I). Four studies[11,12,17,19]consisting of 765 patients estimated the risk factor of VHR. Pooling these studies using a random-effect model showed that no significant differences were found between the two groups (SMD =0.58; 95%CI: -0.21 to 1.37;P= 0.15), with high heterogeneity (χ2= 44.53;P< 0.00001;I2=93%) (Figure 2J).
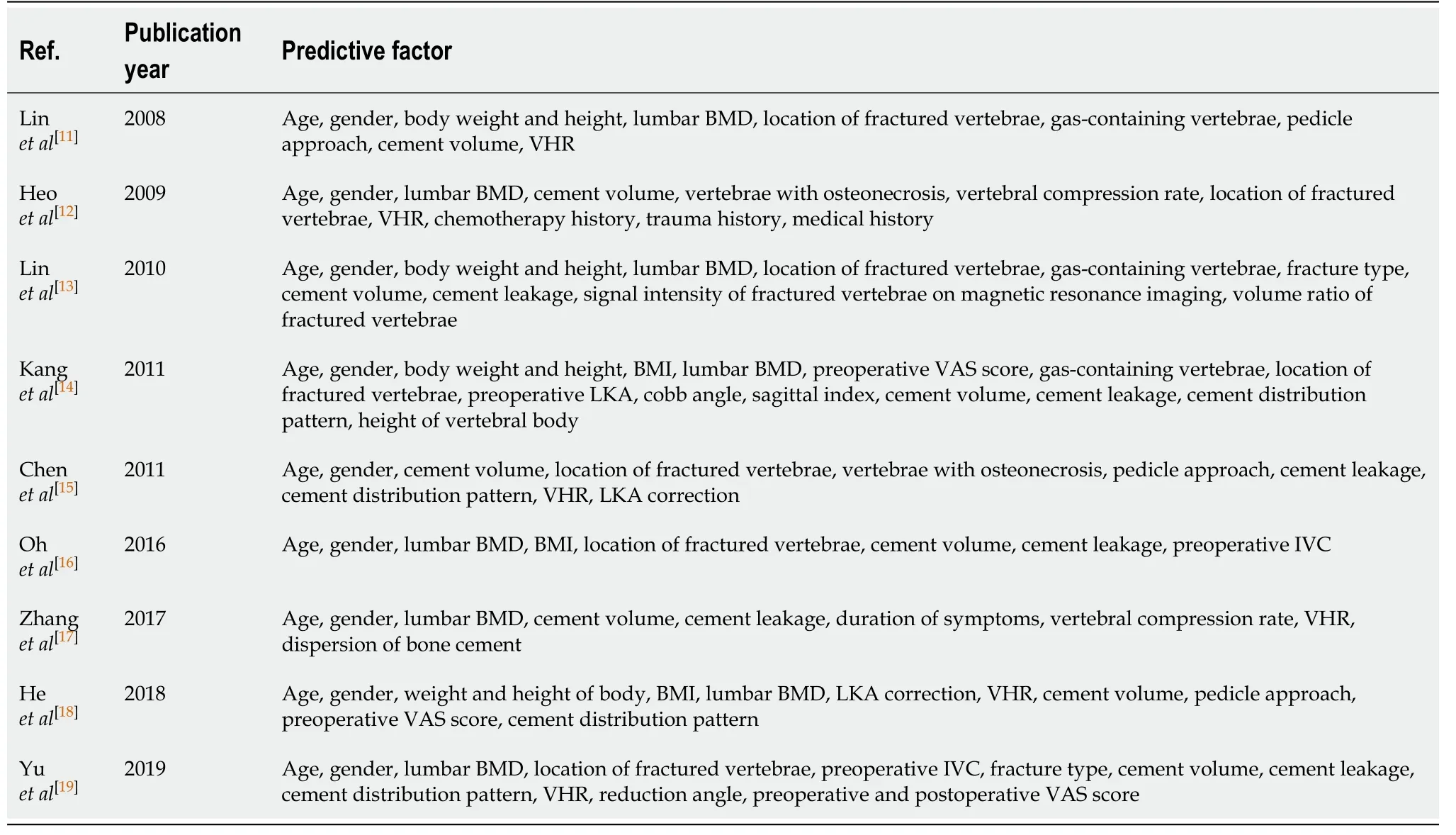
Table 2 Summary of potential risk factors for recollapse involved in all included studies
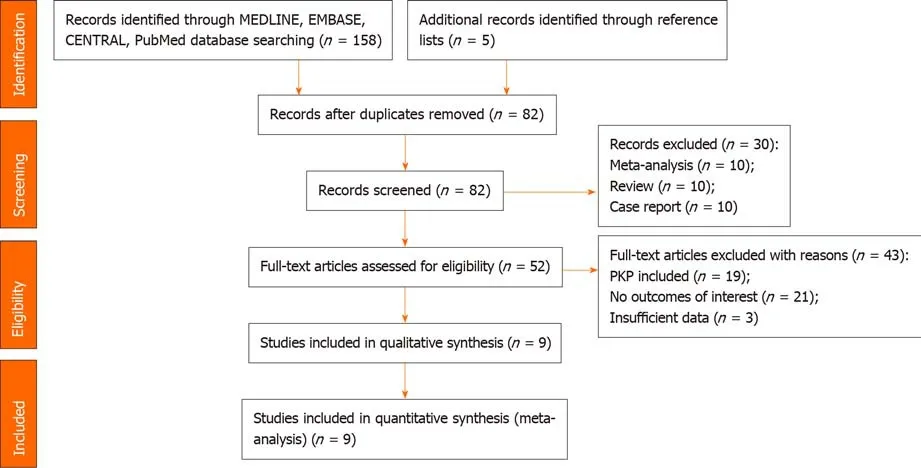
Figure 1 Flow diagram of literature search. PKP: Percutaneous kyphoplasty.

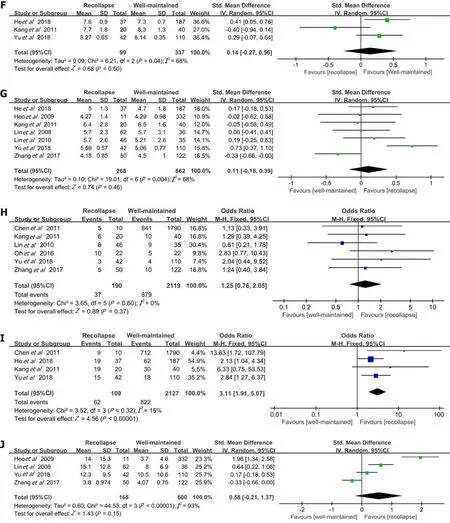
Figure 2 Forest plots of meta-analysis for age, gender (female), lumbar bone mineral density, fractures located at the thoracolumbar junction, preoperative intravertebral cleft, preoperative visual analogue scale scores, injected cement volume, intradiscal cement leakage, cement distribution pattern, and vertebral height restoration. A: Age; B: Gender (female); C: Lumbar bone mineral density; D: Fractures located at the thoracolumbar junction; E: Preoperative intravertebral cleft; F: Preoperative visual analogue scale scores; G: Injected cement volume; H: Intradiscal cement leakage; I: Cement distribution pattern; J: Vertebral height restoration. CI: Confidence interval; SD: Standard deviation.
DISCUSSION
In 1997, Jensenet al[20]first proposed that PVP was a valuable tool in the treatment of painful OVCFs, as it provided acute pain relief and early mobilization. As the safety and efficacy of PVP were gradually recognized by spine surgeons, this treatment was widely used in clinical practice. Recently, an increasing number of cases with the recollapse of cemented vertebrae after PVP without additional trauma have been reported[21,22]. This recollapse is considered a further insufficiency fracture that results in more severe symptoms, deserving our attention. According to our literature review,this is the first meta-analysis covering all relevant studies in a search of the risk factors for the recollapse of cemented vertebrae after PVP in the treatment of OVCFs. A previous meta-analysis[6]evaluated risk factors for the recollapse of augmented vertebrae after percutaneous vertebral augmentation including PVP and PKP. Besides the three risk factors identified through our analysis including fractures located at the thoracolumbar junction (T10-L2), preoperative IVC, and solid lump distribution pattern of the cement, higher VHR and preoperative severe kyphosis were also considered to associate with the cemented vertebra recollapse in the previous work.Reasons for the differences were due to the details of the two techniques. PKP with balloon may better restore the height of fractured vertebrae but at the cost of partially destroying cancellous bones. In PVP, the bone cement penetrates evenly throughout the remaining trabeculae, which makes the stress distribution of the cemented vertebrae more balanced. This interlocking between trabeculae and cement is effective in restoring vertebral stability, but not as significant for vertebral height as PKP. On the other hand, preoperative severe kyphosis is usually accompanied by significant height loss of vertebral body, however, this condition may not be a standard indication for PVP[23]. Therefore, it is more appropriate to explore the risk factors associated with PVP separately.
It is well known that flexion and extension of the spine are greatest at the thoracolumbar junction[24]. Relatively high mobility means a greater chance of injury.Moreover, early after PVP, higher mobility may lead to poor vertebral healing. An unhealed fracture appearing as an intravertebral cleft has been reported to occur frequently in thoracolumbar fractures[25,26]. Additionally, the thoracolumbar junction is a transition area where the spine changes from thoracic kyphotic curve to lumbar lordotic curve[27]. This region bears great load when it is subjected to external force from different directions. In addition, PVP can only fill the fractured vertebra with bone cement but has little expansion effect on the compressed vertebral body. This treatment is thought to preserve local deformity to some extent. Due to the special morphology of the thoracolumbar junction, the center of gravity passes only in front of the anterior half of the vertebral body. Thus, persistent uncompensated sagittal imbalance is deemed a true risk factor for progressive collapse after PVP[28]. A retrospective study[29]in 2014 demonstrated that the thoracolumbar junction was the most frequent region undergoing delayed vertebral collapse after PVP. All of these findings may explain the high incidence of recollapse at the thoracolumbar junction.
We also found that the recollapse of cemented vertebrae could be attributed to the presence of preoperative IVC, which was considered a sign of intravertebral instability[30]. The formation of IVC may be related to partial avascular necrosis in the vertebral body and is significantly associated with the anatomical characteristics of blood supply. In addition to the paired segmental arteries that correspond to a vertebra, the dorsum of the vertebral body can be supplied by collateral blood flow,while the ventral part could not[31]. However, the most frequently damaged portion in OVCFs is the ventral part of the vertebral body. When segmental arteries are impaired,a cleft presenting with a “vacuum” sign on plain radiography develops in the vertebral body due to ischemia. In particular, osteoporotic vertebrae accompanied by severe demineralization may be more susceptible to developing posttraumatic IVCs due to poor blood supply and pre-existing microfractures. These clefts are similar to pseudarthrosis and are connected by fibrocartilaginous tissue with significant motion[32], which indicates instability within the fracture. The dynamic mobility of vertebrae with IVC can be evaluated by flexion and extension radiographs or supine cross-lateral radiographs[33]. Even after PVP, persistent IVCs as weak regions of the vertebral body might further lead to the progressive collapse of cemented vertebrae.One study by Fanget al[34]reported that a high incidence of recollapse could be observed in treated vertebrae with IVC through at least 2 years of follow-up. Similarly,it was suggested that the presence of preoperative IVC, whether with PVP or PKP, was considered high risk for the recollapse of cemented vertebrae[6].
In addition, a solid lump distribution pattern of the cement was also shown to be a predictive risk factor for the recollapse of cemented vertebrae after PVP. It has been reported[18]that the distribution patterns of cement injected into fractured vertebrae are mainly divided into two types: Solid lump and trabecular. As bone cement is directly injected into the vertebral body, the optimum status is that cement interdigitates throughout the fractured vertebrae so that the loads are transferred through the cement column exactly between the vertebral endplates[35]. However, this condition may not be guaranteed for some objective and operational reasons. For example, when injecting bone cement into the osteonecrosis region in osteoporotic vertebrae, a lumpshaped distribution will result after cement solidification[15], where the stiffness of the cemented vertebrae is lower than that in a trabecular cement distribution pattern. The solid lump cement in vertebrae made surrounding non-cemented cancellous bones without load transfer, acting as a stress-shielding effect similar to PKP[36]. The trabecular structure of this stress-shielded area can be destroyed by a round mass congregation of bone cement in daily activities. Due to the osteoporotic nature of vertebrae, a vicious cycle forms to induce recollapse. Differently, the trabecular pattern allows the vertebral body to withstand external forces more evenly, avoiding the stress-shielding effect. Moreover, the interlocking between bone cement and cancellous bone is weakened in the solid lump distribution pattern[18], which leads to insufficient mechanical strength of the vertebral body. Consistent with our findings,Yanget al[37]concluded that lump-shaped cement distribution increased the incidence of recollapse of cemented vertebrae after PVP.
The recollapse of cemented vertebrae may lead to recurrent intractable back pain with no response to conservative treatment, which results from changes in loads over the facet joints along with progressive collapse. This situation seriously affects the quality of life of patients, resulting in certain psychological and physical burden. Not only that, the treatment of vertebral recollapse after PVP seems to be troublesome,which may require repeated PVP or revision surgery depending on the situation[29,38-40].Thus, if predictive risk factors for recollapse are identified preoperatively, surgical fixation and restoration can be used as the initial treatment option for patients whose physical conditions permit. Furthermore, if patients have undergone PVP with the presence of these conditions, surgeons should take the potential risk of recollapse seriously. Regardless of the surgical techniques, regular postoperative follow-up and systematic treatment of osteoporosis are necessary. Once diagnosed, further treatment should be provided by experienced surgeons timely to avoid more serious consequences.
Nevertheless, certain limitations cannot be ignored in this meta-analysis. First, the subjects in these nine studies were Asian, and we thus could not predict whether the results are applicable to patients from other regions. Second, the incidence of recollapse in the included studies might have been affected by the different follow-up periods, which were considered heterogeneous among the studies. Third, some other potential risk factors, such as BMI, steroid usage, vertebral compression rate, and pedicle approach (unilateral or bilateral), were not included in this meta-analysis because of insufficient published data. Finally, the formation of recollapse might result from the interaction of multiple factors; however, the results from the univariate analysis were not able to reveal the effect of an interaction.
CONCLUSION
This meta-analysis suggests that three risk factors, including fractures located at the thoracolumbar junction (T10-L2), preoperative IVC, and solid lump distribution pattern of the cement, are associated with the recollapse of cemented vertebrae after PVP. To the best of our knowledge, this is the first meta-analysis to explore the predictive risk factors for recollapse by synthesizing the available information, and the results will assist surgeons in identifying risk factors both preoperatively and intraoperatively. When treating patients with these conditions, a more comprehensive treatment plan should be developed; moreover, regular and detailed follow-up is necessary for surgeons to detect PVP failure in a timely manner. Prospective multicenter studies with large cohorts should be encouraged to evaluate these results further as well as to clarify the unexplored factors.
ARTICLE HIGHLIGHTS
Research background
Osteoporotic vertebral compression fracture (OVCF) is one of the most common complications of osteoporosis. As a minimally invasive technique for treating OVCFs,percutaneous vertebroplasty (PVP) has been widely used due to its good therapeutic efficacy and safety. However, there have been reports of the cemented vertebra recollapse after PVP, which deserves our attention.
Research motivation
To the best of our knowledge, studies with high-quality and large-scale exploring these risk factors are scarce. The predictive risk factors associated with the recollapse of cemented vertebrae after PVP in OVCFs remain controversial.
Research objectives
We performed this meta-analysis pooling all relevant published data to identify risk factors that might lead to the cemented vertebra recollapse after PVP in OVCFs.
Research methods
A systematic search in EMBASE, MEDLINE, the Cochrane Library, and PubMed was conducted for original articles published up to March 2020. Ten independent variables(age, gender, lumbar bone mineral density, location of the fractured vertebra,preoperative intravertebral cleft, preoperative visual analogue scale score, injected cement volume, intradiscal cement leakage, cement distribution pattern, and vertebral height restoration) were extracted for assessment from the included studies. Review Manager 5.3 was applied for calculating odds ratios (ORs) or standardized mean differences with 95% confidence interval (CI), as well as assessing the heterogeneity by both the chi-squared test and theI-squared test.
Research results
A total of nine case-control studies published between 2008 and 2018 were included in our meta-analysis comprising 300 cases and 2674 controls. The significant risk factors for the recollapse of cemented vertebrae after PVP in OVCFs were fractures located at the thoracolumbar junction (OR = 2.09; 95%CI: 1.30 to 3.38;P= 0.002), preoperative intravertebral cleft (OR = 2.97; 95%CI: 1.93 to 4.57;P< 0.00001), and solid lump distribution pattern of the cement (OR = 3.11; 95%CI: 1.91 to 5.07;P< 0.00001).Furthermore, there was no significant correlation between age, gender, lumbar bone mineral density, preoperative visual analogue scale score, injected cement volume,intradiscal cement leakage, or vertebral height restoration and the cemented vertebra recollapse.
Research conclusions
This meta-analysis supports that three risk factors, including fractures located at the thoracolumbar junction (T10-L2), preoperative IVC, and solid lump distribution pattern of the cement, are associated with the recollapse of cemented vertebrae after PVP in OVCFs.
Research perspectives
This is the first meta-analysis pooling all relevant published data to identify risk factors that may lead to the recollapse of cemented vertebrae after PVP in OVCFs.These findings through analysis can provide valuable information for current clinical work. Also, some other potential risk factors, such as body mass index, steroid usage,vertebral compression rate, and pedicle approach (unilateral or bilateral), need to be evaluated in the future.
ACKNOWLEDGEMENTS
The authors are grateful to Professor Kou CG from the Department of Health Statistics,School of Public Health, Jilin University for his kind help in reviewing the statistical methods and procedures in this meta-analysis.
 World Journal of Clinical Cases2021年12期
World Journal of Clinical Cases2021年12期
- World Journal of Clinical Cases的其它文章
- Standardization of critical care management of non-critically ill patients with COVID-19
- Mediastinal lymphadenopathy in COVID-19: A review of literature
- Polycystic ovary syndrome: Pathways and mechanisms for possible increased susceptibility to COVID-19
- Circulating tumor cells with epithelial-mesenchymal transition markers as potential biomarkers for the diagnosis of lung cancer
- Clinicopathological features of superficial CD34-positive fibroblastic tumor
- Application of a rapid exchange extension catheter technique in type B2/C nonocclusive coronary intervention via a transradial approach
