Standardization of critical care management of non-critically ill patients with COVID-19
Chang-Song Wang, Yang Gao, Kai Kang, Dong-Sheng Fei, Xiang-Lin Meng, Hai-Tao Liu, Yun-Peng Luo, Wei Yang, Qing-Qing Dai, Yan Gao, Ming-Yan Zhao, Kai-Jiang Yu
Chang-Song Wang, Hai-Tao Liu, Department of Critical Care Medicine, Harbin Medical University Cancer Hospital, Harbin 150081, Heilongjiang Province, China
Yang Gao, Kai Kang, Dong-Sheng Fei, Xiang-Lin Meng, Yun-Peng Luo, Wei Yang, Ming-Yan Zhao,Kai-Jiang Yu, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China
Qing-Qing Dai, Department of Critical Care Medicine, The Second Affiliated Hospital of Harbin Medical University, Harbin 150086, Heilongjiang Province, China
Yan Gao, Department of Critical Care Medicine, The Fourth Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China
Kai-Jiang Yu, Institute of Critical Care Medicine, The Sino Russian Medical Research Center of Harbin Medical University, Harbin 150081, Heilongjiang Province, China
Abstract The large global outbreak of coronavirus disease 2019 (COVID-19) has seriously endangered the health care system in China and globally. The sudden surge of patients with severe acute respiratory syndrome coronavirus 2 infection has revealed the shortage of critical care medicine resources and intensivists.Currently, the management of non-critically ill patients with COVID-19 is performed mostly by non-intensive care unit (ICU) physicians, who lack the required professional knowledge, training, and practice in critical care medicine,especially in terms of continuous monitoring of the respiratory function,intervention, and feedback on treatment effects. This clinical problem needs an urgent solution. Therefore, here, we propose a series of clinical strategies for non-ICU physicians aimed at the standardization of the management of non-critically ill patients with COVID-19 from the perspective of critical care medicine. Isolation management is performed to facilitate the implementation of hierarchical monitoring and intervention to ensure the reasonable distribution of scarce critical care medical resources and intensivists, highlight the key patients, timely detection of disease progression, and early and appropriate intervention and organ function support, and thus improve the prognosis. Different management objectives are also set based on the high-risk factors and the severity of patients with COVID-19. The approaches suggested herein will facilitate the timely detection of disease progression, and thus ensure the provision of early and appropriate intervention and organ function support, which will eventually improve the prognosis.
Key Words: Non-critically ill patients; COVID-19; SARS-CoV-2 infection; Standardized management; Isolation management; Hierarchical monitoring and intervention; Different management objectives
INTRODUCTION
The infection caused by a novel coronavirus, which has rapidly spread in China and all over the world, was officially named coronavirus disease 2019 (COVID-19) by the World Health Organization on February 12, 2020[1]. The causative infectious agent of COVID-19 is the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).However, its pathogenesis remains unclear. The existing knowledge is limited to the findings that bats are the original natural hosts and the most probable source of infection, and that angiotensin-converting enzyme 2 is used as a receptor for crossspecies spread[2-5]. The massive epidemic outbreak has posed a major threat to global public health systems. Up to now, this highly pathogenic and transmissible disease still has not shown any signs of abating. The proportion of severe and critically ill patients among SARS-CoV-2-infected patients was close to 20%, with an undoubtedly considerable fatality rate[6-8]. A significant increase has also been observed in the clinical fatality rate among older patients or those with comorbidities and acute respiratory distress syndrome (ARDS)[8-11]. In the absence of effective targeted intervention for SARS-CoV-2 infection[9,12,13], the prevention and timely detection of disease progression and intervention are essential. Therefore, improvements in the standardized management of non-critically ill patients with COVID-19 are crucially important and urgently needed for the timely detection of disease progression and the subsequent provision of early and appropriate intervention and organ function support, which thus improves the prognosis.
According to the “Diagnosis and Treatment of New Coronavirus Pneumonia” (the seventh edition), COVID-19 patients can be classified into mild, moderate, severe, and critically ill cases depending on clinical symptoms and imaging findings. Patients with the below-mentioned high-risk factors are prone to disease progression into severe and critically ill status, and thus need to be closely monitored. The following has been recognized as high-risk factors that are closely related to disease progression and increased fatality rate in patients with COVID-19: Advanced age; comorbidities (such as diabetes, hypertension, and coronary heart disease); persistent high fever; altered state of consciousness; persistent lactic acid > 2.0 mmol/L; progressive increase of white blood cell count, neutrophil count, some inflammatory indicators, D-dimer, liver enzymes, lactate dehydrogenase, myoglobin, myocardial enzymes, ferritin, and troponin; progressive decrease of lymphocyte count and CD4+ and CD8+ T cells[14-18];and increased extent and density of diffuse exudation or consolidation in computed tomography (CT) images[19,20]. Therefore, in our clinical practice, non-critically ill COVID-19 patients have been divided into mild and moderate cases, mild and moderate cases with high-risk factors, and severe cases.
The rapid epidemic outbreak and the surge of patients with COVID-19 in a short period as well as the shortage of intensivists and critical care medical resource have brought substantial difficulties to the standardized management of non-critically ill patients with COVID-19. Currently, the management of non-critically ill patients with COVID-19 is handled mostly by non-intensive care unit (ICU) physicians, such as physicians in the departments of respiratory medicine, infectious diseases, emergency medicine, and even other departments. These medical personnel lack professional critical care medicine knowledge, training, and practice, especially in terms of continuous monitoring of the respiratory function and intervention and feedback on treatment effects. This is especially true for nurses that care for patients with COVID-19[21]. Therefore, appropriate standardization of the management of non-critically ill patients with COVID-19 within limited critical care medical resource is a prominent practical issue.
Critical care medicine has always adhered to the notion of close monitoring.Furthermore, along with early and appropriate organ function support, it is especially important for early diagnosis and timely intervention in non-critically patients with COVID-19 as it can improve their prognosis. Therefore, here, we propose a range of feasible and easy to implement critical care medicine-based clinical strategies that would facilitate the standardization of the management of non-critically ill patients with COVID-19 for non-ICU physicians.
ISOLATION MANAGEMENT
Isolation management of non-critically ill patients with COVID-19 is imperative. Mild and moderate patients with COVID-19, mild and moderate COVID-19 patients with high-risk factors, and severe patients with COVID-19 should be placed in separate areas for different-level management. At this current stage in China, all patients who are diagnosed with COVID-19 need to be hospitalized, no matter whether they are mild, moderate, severe, or critically ill patients. Even asymptomatic patients also need to be quarantined and closely monitored for changes in their condition since asymptomatic and mild infection patients are very likely to transform into moderate,severe, or critically ill patients. However, no clear hierarchical management has been established in clinical practice for COVID-19 patients with high-risk factors and different disease severity. Moreover, challenges exist in the practical realization of that separation management based on the high-risk factors and severity of COVID-19 patients due to medical resource shortage or family outbreaks. In such cases, such a division could be implemented by fixing the room layout or accentuating bedside markers. For example, the first bed on the right side of the entrance to each room should be routinely placed with severe patients with COVID-19 or mild and moderate COVID-19 patients with high-risk factors, as illustrated in Figure 1. The severity of patients with COVID-19 could be represented by different colors, such as red, yellow,and green, representing severe patients with COVID-19, mild and moderate COVID-19 patients with high-risk factors, and mild and moderate patients with COVID-19,respectively, as illustrated in Figure 2.
HIERARCHICAL MONITORING AND INTERVENTION
The purpose of isolation management is to facilitate the implementation of hierarchical monitoring and intervention. In severe patients with COVID-19, at least one of the following criteria has been met: Respiratory distress, respiratory rate ≥ 30 beats/min;mean oxygen saturation ≤ 93% in a resting state; and arterial oxygen partial pressure(PaO2)/ oxygen concentration (FiO2) < 300 mmHg, according to the “Diagnosis and Treatment of New Coronavirus Pneumonia” (the seventh edition). Moreover, these cases could also be identified by pulmonary CT imaging, where significant progression (more than 50%) of the involved area is visible within 48 h. Hence, the aforementioned indicators and the ROX index (the ratio of SpO2/FiO2to the respiratory rate) should be closely monitored as parameters reflecting disease progression in patients with COVID-19.
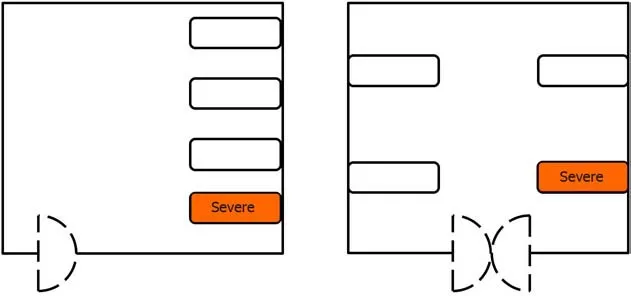
Figure 1 Routine bed layout for severe patients with coronavirus disease 2019 or mild and moderate coronavirus disease 2019 patients with high-risk factors.

Figure 2 Form to facilitate the understanding of the transformation of patient' condition. COVID-19: Coronavirus disease 2019.
Hierarchical monitoring and intervention can ensure the reasonable distribution of scarce critical care medical resources and intensivists, highlight the key patients,timely detection of disease progression, and early and appropriate intervention and organ function support, and thus improve the prognosis. Monitoring indicators generally include temperature, heart rate, respiratory rate, mean oxygen saturation,blood pressure, arterial blood gas analysis, laboratory tests, and imaging examinations. Pulmonary high-resolution CT is essential for early screening, diagnosis,evaluation of disease progression and treatment effect, and prediction of mortality in patients with COVID-19[22-25]. Bedside ultrasound has a broad application prospect in patients with COVID-19 and is especially prioritized for critically ill COVID-19 patients with hypoxemia and hemodynamic failure who are unable to tolerate transport[26]. Certainly, the more critical the condition is, the more comprehensive the content of hierarchical monitoring should be, in order to detect disease progression in time and provide relevant interventions and organ function support. The frequency of monitoring should also vary depending on the high-risk factors and severity of patients with COVID-19, as shown in Table 1.
To obtain earlier warning, the alarm range of the monitor should be set at a respiratory rate of 30 beats/min and mean oxygen saturation of 93%. If medical conditions allow, alarm signals could be real-time transmitted to the central monitoring system. If that is not possible, the alarm information of the monitor could be sent to a doctor or nurse with great speed. That can be performed by training noncritically ill patients with COVID-19, especially mild and moderate cases, and mild and moderate cases with high-risk factors. The easiest way to increase the knowledgeand awareness of non-critically ill patients with COVID-19 is to make and hand them a card with the normal values of common vital signs.
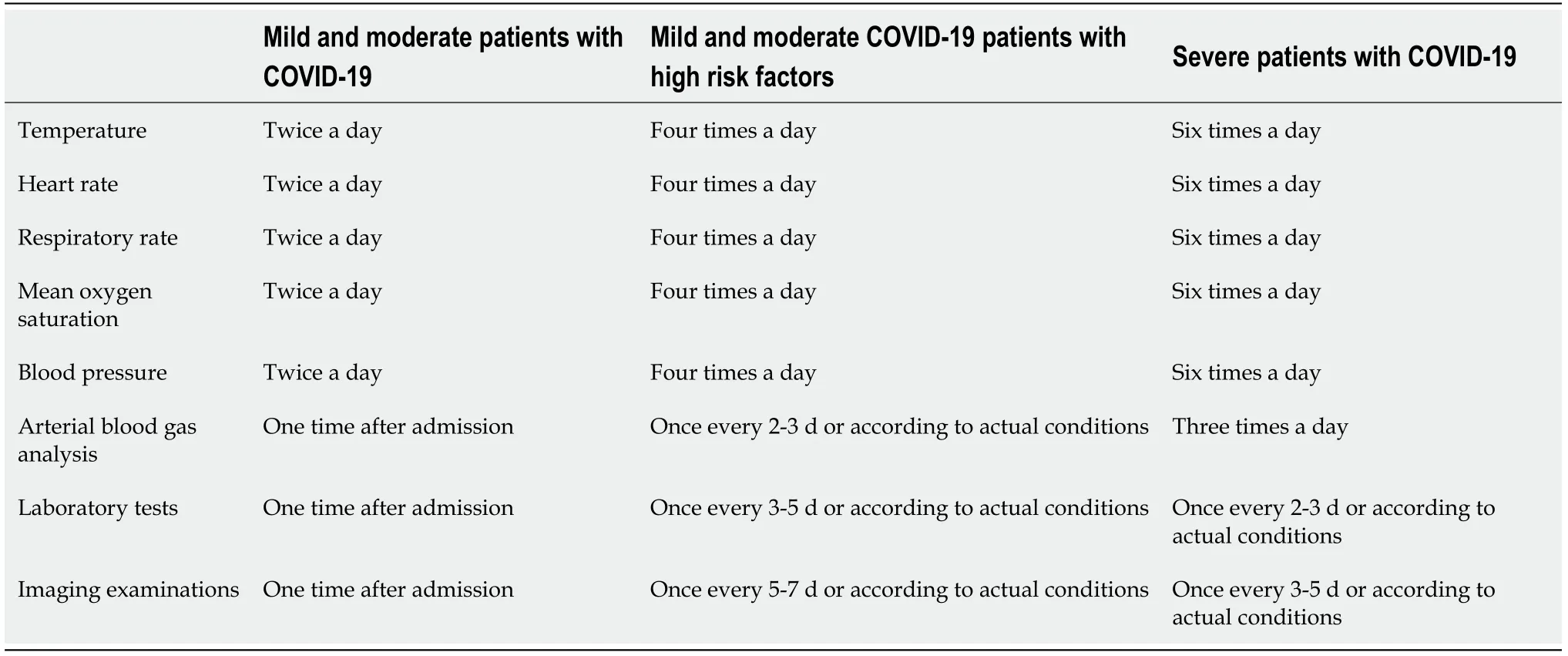
Table 1 Frequency of monitoring depending on the high-risk factors and severity of patients with coronavirus disease 2019
The purpose of hierarchical monitoring is to detect timely disease progression within limited critical care medical resources, providing early and appropriate intervention and organ function support. This approach prevents further deterioration of the condition, facilitate recovery, and improve the prognosis. It is worth noting that the clinical condition of patients with COVID-19 may deteriorate rapidly and progress into critically ill cases. A recent study showed that the 28-d fatality rate of critically ill patients with COVID-19 even exceeded 60%[8]. Undoubtedly, missing the best time window to intervene causes irreversible damage and even death.
DIFFERENT MANAGEMENT OBJECTIVES
Different management objectives should be set based on the aforementioned high-risk factors and the severity of patients with COVID-19. For example, for mild and moderate patients with COVID-19, the primary concern is associated with curative timing, the symptom-free term considered, which could be indicated by clinical signs such as three days without fever and improvement in clinical symptoms and pulmonary CT scan. The secondary focus in such patients is identification of disease progression. The primary and secondary concerns are exactly the opposite in mild and moderate COVID-19 patients with high-risk factors. Furthermore, severe patients with COVID-19 should always be alert for deterioration of their condition and progression to critically ill status. To facilitate the better understanding of the transitional changes in patients' condition, a form such as that depicted in Figure 2 can be designed and placed on the blackboard in the doctor' office as a reminder.
CONCLUSION
Currently, the epidemic is still spreading and raging around the world. The surge of patients with COVID-19 in a short period has made the shortage in critical care medicine resources and intensivists even more apparent. Timely detection of disease progression and subsequent early and appropriate intervention and organ function support could improve the prognosis in non-critically ill patients with COVID-19.Therefore, here, we have proposed a range of clinical strategies for non-ICU physicians aimed at achieving standardized critical care management of non-critically ill patients with COVID-19, including isolation management, hierarchical monitoring and intervention, and the fulfilment of different management objectives.
 World Journal of Clinical Cases2021年12期
World Journal of Clinical Cases2021年12期
- World Journal of Clinical Cases的其它文章
- Mediastinal lymphadenopathy in COVID-19: A review of literature
- Polycystic ovary syndrome: Pathways and mechanisms for possible increased susceptibility to COVID-19
- Circulating tumor cells with epithelial-mesenchymal transition markers as potential biomarkers for the diagnosis of lung cancer
- Clinicopathological features of superficial CD34-positive fibroblastic tumor
- Application of a rapid exchange extension catheter technique in type B2/C nonocclusive coronary intervention via a transradial approach
- Paradoxical relationship between proton pump inhibitors and COVID-19: A systematic review and meta-analysis
