Unilateral disc edema as the first presentation of chronic myeloid leukemia
Suzie Gasparian, Eman Hawy
Department of Ophthalmology, Loma Linda University, Loma Linda, CA 92354, USA
Dear Editor,
We report the first case of unilateral optic disc edema as the first presentation of chronic myeloid leukemia (CML) approximately one year prior to substantial elevation in white blood cell (WBC) count and subsequent diagnosis of CML. Ocular manifestations of leukemia are well recognized, and occasionally serve as the foundation for the leukemic diagnosis[1]. These findings can be secondary to direct infiltration by leukemic cells in the anterior and/or posterior segment of the eye, or by vascular/hematologic pathologies causing changes such as retinal hemorrhages and cottonwool spots[2-3]. Bilateral optic nerve edema has previously been reported as the initial presentation of CML[4-6]. Reported cases of CML have demonstrated bilateral, symmetrically edematous nerves attributed to elevation in intracranial pressure (ICP) in the setting of hyperviscosity, and rarely, isolated optic nerve involvement[1,4-7]. In particular, unilateral optic nerve involvement is more commonly seen in acute forms of leukemia[8], although unilateral involvement in CML has been rarely reported; however, unlike the case in our patient, complete blood count (CBC) demonstrated significant elevation of WBC count upon initial presentation and diagnosis of unilateral optic disc edema[1].
An 18-year-old woman presented with headaches associated with right eye pain (without changes in vision), nausea, and vomiting. Examination revealed visual acuity of 20/20 in each eye. Slit-lamp examination demonstrated a normal anterior segment exam with funduscopic exam demonstrating right optic disc edema and a normal-appearing left optic nerve. Cirrus OCT (Carl Zeiss Meditec, Inc, Dublin, CA, USA) average retinal nerve fiber layer (RNFL) thickness was 268 μm in the right eye and 109 μm in the left eye (Figure 1A). Blood work evaluation showed WBC count of 12.9×109/L and normal red blood cell and platelet count along with biochemistry tests. MRI of the brain and orbits demonstrated flattening of the posterior aspect of the ocular globes without evidence of optic nerve enhancement or structural abnormalities; MRV of the brain demonstrated bilateral narrowing of the transversesigmoid junction without evidence of thrombosis, consistent with imaging findings associated with elevated intracranial pressure ICP. Further workup included a lumbar puncture (LP) with cerebrospinal fluid (CSF) opening pressure of 21 cm water with normal CSF content. With close ophthalmology follow-up, over the course of a few months, unilateral optic disc edema progressed into eventual bilateral optic disc edema with worsening edema and transient episodes of vision loss resistant to maximally tolerated acetazolamide therapy. Repeat fundus exam demonstrated worsening optic disc edema with peripapillary hemorrhages, scattered retinal hemorrhages, cotton-wool spots, Roth spots, and dilated, tortuous vessels in both eyes (Figure 2). OCT average RNFL thickness was 151 μm in the right eye and 178 μm in the left eye (Figure 1B). Repeat imaging revealed worsening signs associated with elevated ICP (Figure 3), with repeat LP opening pressure 35 cm water and otherwise normal CSF composition. Blood work revealed WBC count of 141.9×109/L with rare blasts, and a normal red blood cell and platelet count. Bone marrow biopsy confirmed CML, BCR-ABL1+, chronic phase, and the patient was started on hydroxyurea and allopurinol with eventual transition to bosutinib. Acetazolamide was gradually tapered with resolution of optic disc edema and symptoms, along with normalization of WBC count.
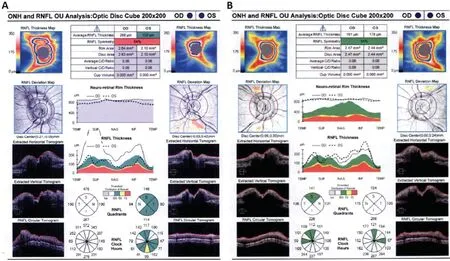
Figure 1 OCT RNFL findings Cirrus OCT RNFL thickness before (A) and after (B) substantial elevation in WBC count with initial treatment including acetazolamide therapy followed by CML treatment.

Figure 2 Fundus photographs Optos California (Marlborough, MA) fundus photos of the right eye (A) and left eye (B) demonstrating bilateral optic nerve edema at the time of diagnosis of CML.

Figure 3 MRI findings demonstrative of characteristic features of elevated intracranial pressure MRI of the brain (A) and orbits (B) and magnetic resonance phlebography of the brain (C) demonstrating flattening of posterior globes (A), intraocular protrusion of optic nerve head (B), and transverse sinus stenosis (C).
CML is a myeloproliferative disorder arising from uncontrolled proliferation of myeloid cells, characterized by a reciprocal t(9;22) chromosomal translocation, which results in the Philadelphia chromosome containing the BCR-ABL1 gene; the median age at presentation is 50 years of age[9]. Though the mechanism underlying leukemia-induced ocular manifestations is not well understood, our case elucidates that optic nerve involvement in leukemias may be more pronounced and may present earlier than other manifestations in the eye. Our patient initially presented with unilateral optic disc edema without changes in her vision and interestingly, without a considerable elevation in her WBC count. Optic disc edema in the setting of leukemia has been attributed to either direct optic nerve infiltration or papilledema secondary to elevated ICP. However, direct leukemic infiltration is more so associated with acute leukemias, which tend to have a unilateral or asymmetric presentation[1,5,8]. Although leukemic cells in the CSF fluid may be undetected, it is unlikely that our patient’s presentation was a result of that. In the setting of chronic leukemias, optic nerve swelling is postulated to be secondary to obstruction of CSF outflow through the arachnoid granulations due to hyperviscosity of the blood in the setting of elevated white blood cells[1,4,7,10]. The mechanism in accordance with the initial ophthalmological picture in our patient is controversial. Our patient had characteristic features of elevated ICP on initial imaging studies[11], and elevated ICP may have simply presented as unilateral disc edema, which has been reported in patients with idiopathic intracranial hypertension (IIH). Previous studies have demonstrated a linear relationship between resistance to CSF outflow and ICP[6]. A substantial elevation in her WBC count could have simply not yet manifested. During subsequent visits, evidence of bilateral optic disc edema associated with retinal hemorrhages and tortuous vessels in the setting of leukocytosis further supports the hypothesis of a diminished blood flow rate due to hyperviscosity resulting in obstruction of proper CSF outflow rather than hematologic abnormalities given her normal red blood cell and platelet count[1,4,7]. Over all, primary and secondary elevations in ICP may even co-exist. Our patient significantly improved following CML treatment and tapering of acetazolamide with normalization in WBC count and preservation of her vision suggesting that optic nerve edema was due to elevated ICP rather than nerve infiltration.
CBC is an important diagnostic consideration in patients who present with optic disc edema, but may not always initially confirm the diagnosis. Patients with CML may thus have atypical presentations at a young age with exam findings such as unilateral disc edema and symptoms mimicking IIH long before leukocytosis is seen. This case highlights the importance of maintaining a high clinical suspicion for secondary causes of optic disc edema and the early diagnosis of leukemia in patients suspected to have IIH.
ACKNOWLEDGEMENTS
Conflicts of Interest: Gasparian S,None;Hawy E,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
