An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
Faried Wagdy, Tharwat H. Mokbel, Hisham Elsorogy, Ahmed Alnagdy, Dina Abd Elfattah, Abd-Elmonem A. Elhesy
1Menofia University Hospital, Menofia University, Menofia 32511, Egypt
2Mansoura Ophthalmic Center, Faculty of Medicine, Mansoura University, Mansoura 35516, Egypt
Abstract
INTRODUCTION
Trabeculectomy is the main surgery that used for glaucoma. Despite the good decline in intraocular pressure (IOP) that occurs rapidly after the procedure, a failure might occur due to progressive subconjunctival fibrosis associated with an increased IOP[1-3]. If the bleb is revived by needling with use of antimetabolites as mitomycin C (MMC) that is usually used during the operation, the associated increase in IOP will be controlled if the revision occurred early within the first three months after surgery[4]. However, likelihood of success is less if the bleb revision is delayed[5-6].
If the bleb revision fails, alternative surgeries include a second trabeculectomy or an aqueous implant surgery[7-8].
The Ex-Press shunt permits the flow of the aqueous humour from the anterior chamber of the eye like a trabeculectomy. It is a non-valved shunt. This procedure is less traumatic and invasive than a subscleral trabeculectomy (SST) with regards to non-removal of the trabecular tissue or the peripheral iris. Few complications, low diffuse bleb, and low incidence of bleb-related complications such as subconjunctival fibrosis and a high success rate are also observed[9-15].
The present study aimed to compare the outcome of the surgery and complications related to the bleb between Ex-Press implant and SST in the management of glaucoma after previous trabeculectomy with a fibrotic bleb, while other studies focused on comparing both techniques only for the management of glaucoma as primary techniques not after bleb failure of a previous trabeculectomy.
SUBJECTS AND METHODS
Ethical ApprovalEthics Committee approval was obtained (Institutional Review Board, IRB), Faculty of Medicine, Menofia University in acceptance with Declaration of Helsinki principles on number 3/2017 OPHT3. Written informed consent was taken from all patients before any study procedures. This trial was registered with ClinicalTrial.gov (NCT04417920).
Overall, 28 eyes of 28 patients with open angle glaucoma, despite maximally tolerated medication and previous SST with a fibrotic bleb for more than 4mo, were enrolled in this prospective randomized controlled clinical study in which the randomization was applied by a random number table (computer-generated). Other types of glaucoma, patients who complained of any diseases that interfered with wound healing such as diabetes and other vascular or auto-immune disorders, SST failure other than fibrotic bleb, patients who followed less than 4mo after the first surgery, and those less than 12mo after the second surgery were not included the present study.
This prospective study included those patients who diagnosed with increased IOP with fibrotic bleb however previous SST. The present study was done in Menofia University Hospital between July 2017 and May 2019, where the eyes conducted in the study were classified into two groups. Group I included 14 eyes that were subjected to Ex-Press implant surgery, and group II included 14 eyes that were subjected to SST with MMC. Follow-up continued until one year after surgery was performed.
Preoperative examination for all patients (42 to 55 years old) was performed including IOP using a Goldmann applanation tonometer, visual acuity (VA) using Snellen chart, visual field (VF) by Humphrey perimeter, angle examination by Goniolens, optic disc examination by Volk+90 lens, examination for the previous bleb, upper bulbar conjunctiva, and anterior chamber depth using slit lamp. Peri-bulbar anaesthesia was used for all patients.
The operative technique in group I (Ex-Press implant) was similar to that of group II (trabeculectomy) except with no sclerectomy or peripheral iridectomy. The steps included conjunctival peritomy superior-temporal away from the site of the fibrotic bleb at 12 o’clock, light cauterisation, and administration of MMC with 0.2 mg/mL concentration. MMC were placed over the sclera using three sponges for 2min, followed by copious irrigation with balanced salt solution, triangular scleral flap, and scleral dissection forward to the clear cornea to allow scleral spur to be exposed. Thereafter, a hole was fashioned using a sapphire blade (Alcon laboratories, USA). An Ex-Press implant 3 mm long with an external diameter of 400 μm was implanted, followed by the closure of scleral flap and conjunctiva (Figures 1 and 2).
In group II, trabeculectomy with MMC was performed in the superior-temporally region away from the fibrotic bleb at 12 o’clock. MMC of the same concentration as in the Ex-Press technique was administered, followed by sclerectomy and a peripheral iridectomy.
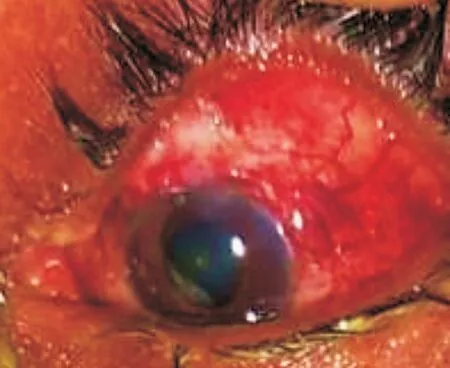
Figure 1 Female patient 46 years old (group II), 1wk after the surgery with old fibrotic bleb at 12 o’clock and a second trabeculectomy superotemporally.

Figure 2 Female patient 48 years old (group I), 4mo after the surgery with old fibrotic bleb at 12 o’clock and an Ex-Press implant superotemporally.
Prednisolone acetate 1% and moxifloxacin 0.5% eye drops every 2h were to be taken by the patients for at least 1mo after surgery, and then gradually withdrawn based on clinical improvement. All glaucoma medications were stopped in the postoperative period and were used only if needed. No specific drugs that modulated wound healing were administered to the patients.
The follow-up criteria of these patients included IOP, VA, VF, and optic disc examination by Volk+90 lens, Slit lamp examination for the recent bleb, upper bulbar conjunctiva, and anterior chamber depth.
Reduction of IOP throughout the follow-up period in one year was considered a primary surgical outcome. Complete success was defined as an IOP lower than 21 mm Hg without treatment; a qualified success was defined as an IOP lower than 21 mm Hg with medical treatment. The treatment was deemed to be a failure if the IOP was more than 21 mm Hg with medical treatment at any time during the follow-up period.
Secondary surgical outcomes were presented as postoperative changes in VA, VF, and bleb-related complications throughout the follow-up period of one year.
A statistical power analysis was performed after sample size estimation, based on data from the present study (n=28),distributed into 2 groups. The effect size for this study was 2.28, considered to be large using Cohen’s (1988) criteria, with an alpha=0.05 and sample size=28 distributed as 14 for group I and 14 for group II, a post-hoc power analysis was conducted with this effect size (G Power 3.1) and it is approximately (1-β)=0.83. Thus, the power analysis for the sample size is adequate for the main aim of this study.

Table 1 IOP of the studied groups mean±SD, median (IQR)
Statistical AnalysisAnalysis of the study was done by SPSS version 22 (SPSS Inc., Chicago, IL, USA). Mann-Whitney and Wilcoxon signed-rank tests were used for non-parametric data. Fisher’s exact test was used for qualitative variables. The P value was considered significant if P<0.05.
RESULTS
The patients aged between 42 and 55y (11 men and 17 women). Despite the maximally tolerated treatment after previous SST surgery with a fibrotic bleb, the patients were diagnosed with primary open angle glaucoma (POAG) and had a high IOP. The preoperative median IOP was 31.50 mm Hg with a range of 29-34 mm Hg in group I and range of 29.75-33.25 mm Hg in group II. IOP showed significant reduction in both groups throughout the follow up period after 1y. Median IOP in group I after 1y was 14.5 mm Hg with a range of 14-16.5 mm Hg (P=0.001) while in group II, the median IOP was 16.50 mm Hg with a range of 14.75-23.5 mm Hg (P=0.001; Table 1, Figure 3). No significant difference in IOP reduction was observed in either group. Postoperative elevation in IOP was reported. In group I, one patient showed an increase in IOP that occurred after one month; IOP was 27 mm Hg and decreased to 15 mm Hg with two topical drugs in the form of an alpha agonist and a betablocker. In group II, three cases showed a rise in IOP and were controlled as follows: one case was controlled by a single betablocker medication, the second case was controlled by two medications in the form of an alpha agonist and a betablocker. In the third case, the IOP was initially controlled by administration of an alpha agonist and a betablocker; however, the patient presented with subconjunctival fibrosis at the new bleb and consequently, prostaglandin drug was also prescribed to reduce IOP from 29 mm Hg to 15 mm Hg. Complete success occurred in 92.9% of patients in group I and 78.6% in group II. The qualified success rate was 7.1% in group I and 21.4 % in group II (Table 1).There was stability in VA and VF, with only one case in group II showing a decrease in one line in the Snellen chart, and this case also showed a more deterioration in the VF.Table 2 summarizes the postoperative complications in both groups. Slit-lamp examination clarified shallow anterior chamber that was clinically diagnosed and considered if iridocorneal touch occurred in the periphery. This was noted in two cases in group II that were presented with hypotony and improved 2d later with cycloplegic and steroid topical eye drops. Hypotony was seen in three cases in group II and in two cases in group I due to excess filtration and improved after 3d. Choroidal detachment was identified in one eye in group I (7.1%) and disappeared spontaneously within 2mo. There was one case of hyphaemia in group I (7.1%) and three cases in group II (21.4%). In addition, no cases in the group I showed any blockage of the implant with fibrin or blood.

Figure 3 Follow-up of the studied IOP among the studied groups over time.
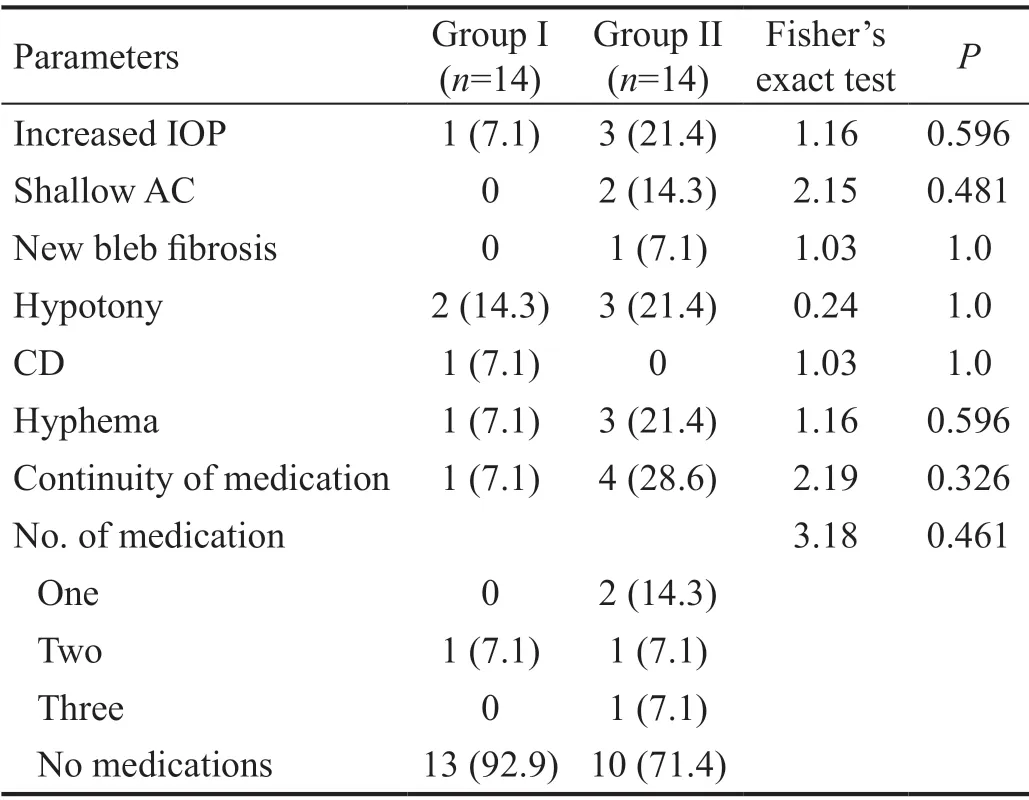
Table 2 Postoperative complications of the studied groups n (%)
DISCUSSION
Fibrotic blebs are a common cause of failure after glaucoma surgery. Bleb needling and revision usually give poor results if the subconjunctival fibrosis occurres late after 4mo of the primary trabeculectomy; therefore, additional surgeries may be needed for IOP control[7-8].
This study has shown that there was a significant reduction in IOP as a primary surgical outcome in both surgeries during the follow-up period, which reflected the effectiveness of both surgeries in IOP control up to one year after surgery. Secondary surgical outcomes were presented as a stability in postoperative VA, VF, and less incidence of bleb-related complications in the group I after 1y which might be related to the advantage of the Ex-Press implant as less invasive technique as compared to conventional trabeculectomy.
The novelty of the technique was clarified in the application of Ex-Press implants in cases with a fibrotic bleb in comparison with the conventional trabeculectomy, as both techniques may differ in primary surgical procedures based on previous studies. The results of the Ex-Press implant were clarified in different studies that were performed as a primary procedure, similar to a study that compared trabeculectomy and Ex-Press implants. In that study, the preoperative IOP was 24.5±9.2 mm Hg in group II and 22.3±9.3 mm Hg in the group I. In group II, complete success occurred in 62.3% of cases and qualified success occurred in 24.6% of cases. In the group I, complete success occurred in 66.6% of cases and qualified success occurred in 17.9% of cases[9].
Another study also provided similar results: mean preoperative IOP lowered from 31.1±14.2 to 16.2±1.5 mm Hg in the trabeculectomy group, and from 28.1±9.0 to 15.7±1.8 mm Hg in the Ex-Press group at the last follow-up visit. The mean of antiglaucoma medications at the last follow-up decreased from 3.7 before the surgery to 0.9 after SST versus the 0.3 mean after Ex-Press surgery in both groups. Complete success was greater in group I than the trabeculectomy group. Postoperative complications were reported more frequently in SST (33%) than after Ex-Press surgery implant (20%)[10].
Similar results were observed after the Ex-Press implant was performed by Wagschal et al[11]. IOP was not significantly different between the groups. Complete success was 57% compared with 70% in the SST versus Ex-Press groups, respectively. No significant differences were reported regarding the time of surgery, number of antiglaucoma medications, VA, and postoperative complications between the group I and group II.
Other studies clarified a significant reduction in mean IOP compared with preoperative IOP in both groups. In one study, after 2y of follow-up, the mean IOP was 14.7±4.6 mm Hg and 14.6±7.1 mm Hg in the Ex-Press and trabeculectomy groups, and the success rates were 83% and 79% in the groups I and II. Complications that occurred postoperatively were more in the trabeculectomy group than in group I[12]. A retrospective study of patients who underwent trabeculectomy or Ex-Press shunt implantation showed no differences in the IOP-lowering effect or number of postoperative antiglaucoma medications between the two groups. Success rates were 86.9% for trabeculectomy and 84.6% for Ex-Press. Failure rate and hypotony were not different significantly between the two groups[13].
Moisseiev et al[16]clarified that IOP values declined significantly in the trabeculectomy group from 27.8±7.9 to 11.1±3.9 mm Hg and from 27.7±9.2 to 11.5±3.7 mm Hg in group I after 1y. The success rate was not significantly different between the groups was reported. Less choroidal detachment was reported in group I due to more reduction in postoperative IOP.
Eight controlled clinical trials were included in study that included 605 eyes from 559 patients with uncontrolled glaucoma who were medically treated. The mean difference in the IOP lowering percentage was 2.33 when comparing Ex-Press with SST. Ex-Press was associated with greater IOP reduction numerically, but with no significant difference with the SST group. Hypotony and hyphaemia were significantly lower in the Ex-Press group[17].
George et al[18]reported that Ex-Press implants have a high efficacy even in difficult types of glaucoma. In total, 45 patients and 49 glaucoma cases were included in the study. Significant IOP reduction was reported in different refractory glaucoma such as pseudophakia, aphakia, pigmentary, and neovascular glaucoma. The rate of Ex-Press mini shunt failure was 18.52%. Postoperative complications were observed in 20 (40.82%) cases[18].
Dewang et al[19], in another study, clarified the outcome of Ex-Press implant in advanced glaucoma. The diagnosis included primary angle closure glaucoma, POAG, juvenile open angle glaucoma, uveitic glaucoma, and neovascular glaucoma. The mean preoperative IOP was 29.58±7.13 mm Hg, which decreased to 17.40±0.89. Absolute success was seen in 66.7% of eyes and qualified success in 16.7% of eyes, at the 1-year follow-up[19].
Ex-Press implant was an effective procedure with lower complications when compared to SST in different studies as a primary procedure[20].
In conclusion, Ex-Press implant surgery and SST with MMC are effective for controlling IOP in late failure that occurs more than 4mo after previous SST with a fibrotic bleb, however Ex-Press shunt provided fewer complications as compared to conventional trabeculectomy.
The limitations of this study were the relatively small number of patients in addition to short-term follow-up. In the future, we intend to examine a larger study sample with a long-term follow-up to investigate the effectiveness and safety of this surgical technique and to evaluate the long-term postoperative changes. The strengths of the study were the effectiveness of the Ex-Press implant as a novel technique in patients who have had previous trabeculectomy with a fibrotic bleb with the advantage of eliminating peripheral iridectomy and the need for tissue removal, short time consumption , and less incidence of bleb-related complications.
ACKNOWLEDGEMENTS
All authors thanks Taha Baker for his help.
Conflicts of Interest: Wagdy F,None;Mokbel TH,None;Elsorogy H,None;Alnagdy A,None;Elfattah DA,None;Elhesy AEA,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Corneal stromal mesenchymal stem cells: reconstructing a bioactive cornea and repairing the corneal limbus and stromal microenvironment
- Real-world outcomes of two-year Conbercept therapy for diabetic macular edema
- Role of home monitoring with iCare ONE rebound tonometer in glaucoma patients management
- Comparing posture induced intraocular pressure variations in normal subjects and glaucoma patients
- High interpretable machine learning classifier for early glaucoma diagnosis
- Micropulse laser trabeculoplasty under maximal tolerable glaucoma eyedrops: treatment effectiveness and impact of surgical expertise
