Comparing posture induced intraocular pressure variations in normal subjects and glaucoma patients
Onyekachi Jane Ireka, Chimdia E Ogbonnaya, Obinna C Arinze, Nneka Ogbu, Chimdi M Chuka-Okosa
1Department of Ophthalmology, Alex Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi State 48028, Nigeria
2Department of Ophthalmology, University of Nigeria Teaching Hospital, Ituku Ozalla, Enugu 01129, Nigeria
Abstract
INTRODUCTION
Primary open angle glaucoma (POAG) is the most predominant type of glaucoma worldwide and in Africans[1-4]. It is a progressive and chronic optic neuropathy which has characteristic optic disc and visual field changes resulting from death of retinal ganglion cells and their axons[1]. Among other risk factors for POAG, raised intraocular pressure (IOP) is the commonest and at present, the only risk factor that can be modified[5-7].
Glaucoma is the second most common cause of blindness behind cataract and the leading cause of irreversible loss of vision worldwide[8]. It is estimated that the number of people with glaucoma worldwide will rise from 64 million to 76 million in 2020 which will double in 2040, with Africa and Asia being more affected than the rest of the world[3]. A population based survey in Nigeria showed that glaucoma is the second most common cause of blindness and the leading cause of irreversible blindness accounting for 16.7% of causes blindness with a prevalence of 0.7% [95% confidence interval (CI) 0.55%-0.88%][9]. Igbo ethnic group was identified as one of the risk factors for POAG among Nigerian subjects[9].
The chronic elevation in IOP which occurs in POAG causes deformation of the lamina cribosa[10-11]. This causes compression of ganglion cell axon as well as affects their blood supply resulting in impaired axoplasmic flow and poor perfusion of the optic nerve head with consequent death of these axons seen as cupping in optic nerve head during fundus examination[10-11]. Studies had shown that IOP fluctuates with change in posture with glaucomatous eyes having greater IOP elevation than non-glaucomatous eyes during changes in such body positions (from sitting to a horizontal position)[12-14].
In a study to determine the relationship between the postural changes of the IOP and the visual field loss in patients with POAG, Hirrooka and Shiraga[15]reported that IOP was higher in treated and untreated POAG group compared to normal when subjects changed from a sitting to supine position. Similar findings were made by Buys et al[16]and Katsanos et al[17]who observed higher posture-induced changes in IOP among the glaucoma patients than non-glaucoma subjects.
On the other hand, some studies have described no difference in posture induced IOP variation between glaucomatous and non-glaucomatous eyes[18-19]. Sawada and Yamamoto[19]in Japan reported that posture induced IOP variations were similar among eyes with primary open-angle closure with and without glaucoma medications and control eyes.
The effect of posture changes on IOP between glaucoma and non-glaucoma subjects remains controversial. While some authors have observed differences in posture induced IOP variation between glaucomatous and non-glaucomatous eyes, others have not. Most of these studies were done in Caucasians with few in African population. Do the African population have greater fluctuations in posture induced IOP than the Caucasians? In Sub-Saharan Africa, there is paucity of published data documenting IOP variation associated with changes in posture. It is well documented that POAG in African population tends to be more aggressive and difficult to treat[2,20-22]. To the best of our knowledge this is going to be the first study in Nigeria to compare postureinduced IOP variation among glaucoma and non-glaucoma patients. Therefore, the purpose of this study is to compare the posture-induced variations in IOP between the POAG and non-glaucoma subjects.
SUBJECTS AND METHODS
Ethical ApprovalEthical approval was obtained from Research and Ethical committee of Alex Ekwueme Federal University Teaching Hospital, Abakalik in line with Declaration of Helsinki. All the participants included in the study were fully informed on the procedures for study evaluation. Details concerning the further assessment and measurements of IOP in different positions were further explained to them and a signed, written or thumb printed consent obtained before participation. Only those who gave voluntary consent were recruited.
Study DesignThis was a case control study among newly diagnosed patients with POAG and age-matched non- glaucomatous patients as controls.
Study PopulationParticipants for the study were drawn from patients attending Glaucoma clinic and general Ophthalmology clinic between July to September 2017 in the Department of Ophthalmology Federal Teaching Hospital, Abakaliki, Ebonyi State. The cohorts included newly diagnosed POAG patients aged ≥30y and age-matched nonglaucomatous participants (aged 30-70y) attending the same clinics.
Inclusion CriteriaPOAG was diagnosed[1,7,23-24]if the patient met the following criteria: 1) open anterior chamber angle (Shaffer’s grade 3 or 4 in all quadrants); 2) raised IOP (≥22 mm Hg), this is the true IOP after accounting for central corneal thickness (via pachymetry); 3) a vertical cupdisc ratio of ≥0.6 or asymmetry of disc cupping equal to or greater than 0.2 with or without the following disc changes: a rim notching or thinning of the rim, disc haemorrhage or violation of the ISNT (inferior, superior, nasal, temporal) rule, seen on dilated fundoscopy using +78 D in one or both eyes; 4) characteristic glaucomatous visual field defect (such as nasal step, paracentral scotoma, temporal wedge defect, seidel scotoma, arcuate scotoma, double arcuate scotoma using automated Perimetry using Optos Automated Perimeter Model AP 200) may or may not be present.
Non-glaucomatous patient was one who in each eye met the following criteria[25-26]: 1) vertical cup-disc ratio of <0.6, no disc asymmetry of >0.2, no rim notching or thinning of the rim, no disc haemorrhage or violation of the ISNT rule, and no disc pathology, with pink rim seen on dilated fundoscopy using +78 D; 2) true IOP of <22 mm Hg after pachymetry.
Exclusion CriteriaParticipants were <30y, did not give consent to participate in the study, diagnosed with POAG before this study, with other types of glaucoma, previous ocular surgeries or anterior segment pathologies such as acute or chronic uveitis, or any corneal abnormality that would prevent reliable IOP measurement such as corneal opacity, diabetic or hypertensive or blood pressure >130/80 mm Hg, subjects on medications known to influence IOP.
Clinical EvaluationThe bio data (age, sex, marital status etc.) of all new participants were collected. Biometric measurements were taken from each of them and recorded in the questionnaire. The body mass index was then calculated for each of them. Each of them had his/her unaided/aided distant visual acuity measured.
Detailed history and compressive systemic review and ocular examination were done. Pupillary reactions to light (direct, consensual, and swinging flashlight tests) were tested in a dimly lit room. Examination of the anterior segment was performed using the slit lamp bio microscope Keeler SL-16. Autorefraction and subjective refraction were done. The IOP was measured using Perkin’s handheld applanation tonometer and pachymetry was done to ascertain the central corneal thickness. The actual (true) IOP was recorded. Gonioscopy was performed using the Goldmann 2-mirror lens and the anterior chamber angles were graded using the Shaffer’s grading system.
Posterior segment examination with slit lamp and +78 D was done after dilating with topical tropicamide. Automated perimetry was performed using the Optos Automated Perimeter Model AP 200.
Measurement of IOP in Various Postures Measurements of IOP were taken in three positions namely sitting, supine flat and supine with pillow. The subjects were instructed to sit quietly near one end of an examination couch. A topical anaesthetic, 0.5% tetracaine hydrochloride, was instilled into the eyes. Then a fluorescein sodium strips 1 mg was applied into the inferior conjunctiva sac and removed immediately (and subsequently instilled a minute before measurements). The IOP of one eye (right before left), was measured after 15min while patient was in a sitting position. The subject then lay flat. This body position was maintained for 15min, and the IOP measured. Then a thick pillow was placed underneath the patient’s head (head elevation of 30°) and IOP was recorded after 15min of this posture. The same size of pillows (dimension: 65×45×23 cm3) was used for all patients. The dimensions of the used pillows were periodically checked. There were multiple spare pillows of the same dimension which was used to replace any pillow that did not meet the required dimension.
The same researcher measured IOP of all the participants and measurements were taken between 10:00 a.m. and 12:00 a.m. to minimize the effect of diurnal variations in IOP[12,27]. Excessive pressures on the globe as well as corneal abrasion resulting from rough handling of instruments were avoided during IOP measurement.
Statistical Analysis Using previous published data, the anticipated mean change in IOP of 3.1 mm Hg in POAG[12,16]patients and 2.47 mm Hg in non-glaucoma subjects[28]; the sample size was calculated to be 55 for each group at a standard deviation (SD)[29-30]of 2.6 mm Hg and the power was set at 90%. All statistical analyses were performed using SPSS version 22.0 (SPSS, Inc). Data were expressed as means and frequency. Pearson's Chi-square test was performed for categorical variables. Student's t-test was performed to determine the mean change in IOP. Differences were based on a significance level of P<0.05.
RESULTS
A total of 111 patients (55 POAG patients and 56 nonglaucoma subjects) participated in the study. There were 30 males and 25 females in POAG group; and 26 males and 30 females in the non-glaucoma group with age range 30-70y. Majority of subjects (40.50%) were within 40-49y while the least (2.70%) were older than 70y. Their age distribution is shown in Figure 1.

Figure 1 Age distribution of POAG and non-glaucoma (N-G) subjects.

Table 1 Demographic characteristics of the POAG and the nonglaucomatous subjects mean±SD
The physical biometric characteristics of POAG and nonglaucoma subjects are shown in Table 1. Mean age, height and weight were not significantly different between the two groups. However, there was a statistically significant difference (t=-2.332, P=0.022) in the mean body mass index of 25.17±2.48 in POAG and 26.43±3.15 kg/m2in nonglaucoma group. There was no difference in the mean central corneal thickness between the right and the left eyes of both POAG and non-glaucomatous subjects. However, there was statistically significant difference (t=-3.358, P<0.001) in the mean central corneal thickness of patients with POAG and that of the controls.
In non-glaucomatous subjects, there was no significant difference of the mean IOP in the right and left eye during sitting, supine flat, and supine with pillow positions. The mean IOP in the sitting position was 12.28±1.83 mm Hg, which was lower than that measured in the supine with pillow (13.71±1.79 mm Hg, t=-15.344, P<0.001) and was much lower than in supine flat position (16.30±1.90 mm Hg, t= -31.078, P<0.001). In the supine with pillow, IOP was lower than supine flat position (t=29.30, P<0.001; Tables 2 and 3).In the POAG patients, the mean IOP upon sitting was 27.54±3.98 mm Hg, which was lower than that obtained in supine flat (35.22±4.61 mm Hg, t=-27.415, P<0.001), and supine with pillow (30.15±4.41 mm Hg, t=-13.016, P<0.001) positions respectively. Mean IOP was higher in the supineflat compared to supine with pillow positions (t=16.802, P<0.001; Tables 2 and 3).
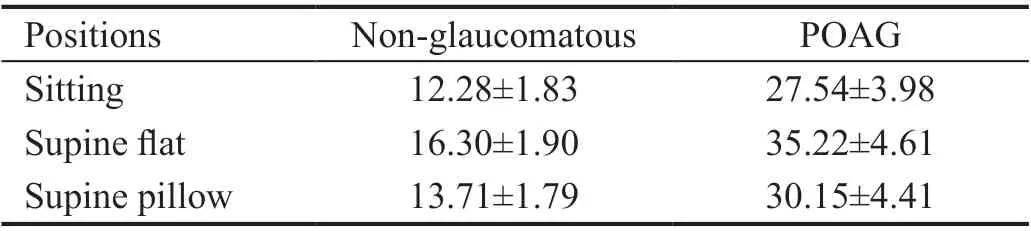
Table 2 Mean IOP of the various postures in the non-glaucomatous subjects and POAG patients mean±SD

Table 3 Mean IOP differences between the various postures among the POAG and non-glaucoma subjects mean±SD
Mean IOP variations with postural changes between the POAG and the non-glaucoma patients are illustrated in Table 3. The mean differences in IOP variation in the sitting compared to supine flat was 7.68±2.08 mm Hg in POAG and 4.03±0.13 mm Hg in non-glaucoma subjects respectively (t=13.106, P<0.001). In sitting compared to supine with pillow positions, the mean difference in IOP variations was 2.61±1.49 mm Hg in POAG and 1.44±0.70 mm Hg in nonglaucoma patients (t=5.310, P<0.001). Supine flat compared to supine with pillow in POAG was 5.07±2.24 mm Hg, where as it was 2.59±0.66 mm Hg in non-glaucoma subjects which was statistically significant (t=7.942, P<0.001)
DISCUSSION
This study observed that the mean differences in IOP change which occurred in non-glaucoma subjects as they change from a sitting to a supine flat position was 4.03±0.13 mm Hg (P<0.001). Upon elevating the head with a pillow from a supine flat position, the mean difference reduced to 2.59±0.66 mm Hg (P<0.001). It was lowest when subjects changed from a recumbent to a sitting position (P<0.001). These findings were similar to those from previous studies[25-26,30]that showed that IOP variation associated with posture in normal subjects was lower in the sitting compared to supine positions.
Our study showed a greater increase in the mean IOP variations of 4.03±0.13 mm Hg upon changing from a sitting to a supine position compared to lower values observed by Rajendra[25]and Jorge et al[28]which were (2.79±0.01 and 2.47±2.12 mm Hg in the same positions respectively. This greater increase in the mean difference of posture induced IOP variations observed in this study could be as a result of age differences of subjects studied.
The studies mentioned above employed younger subjects aged between 18 and 34y whose IOP changes with posture were expected to be more stable, while the subjects in this study were aged between 30 and 70y. Our study also, was on African population while theirs were on Caucasians. It is also possible that African subjects show greater degree of fluctuations in IOP and this may be one of the contributing factors to more the aggressive glaucoma which are more difficult to treat seen among this group.
The results of the present study corroborated with reports of Liu et al[31], which documented a mean IOP increase of 6 mm Hg from sitting to a supine position in normal subjects during a 24h monitoring of IOP. The increase in IOP which occurred on adopting a supine from a sitting position has been attributed to increase in episcleral venous pressure and increase in resistance to aqueous flow[25,32-33].
Yeon et al[26]reported mean IOP rise of 3.8±2.3 mm Hg in normal subjects after changing from sitting to a supine flat position which was similar to the result of this study. In contrast to their study which revealed that IOP increased in 6 out of 24 patients after changing from a supine flat to a supine with multiple pillows position, this study showed no such increase when subjects changed from supine flat to supine with pillow positions.
Some studies[2,12,15,34]had reported that the amount of increase in IOP associated with change in body positions varied significantly from 0.3 to 5.6 mm Hg or more in normal healthy subjects, normal tension glaucoma and POAG respectively. The present study showed mean IOP variation of 4.03±0.13 mm Hg in non-glaucoma and as much as 7.68±2.08 mm Hg in POAG group as subjects changed from sitting to supine (supine flat) position.
Greater increase in IOP was observed in our subjects, being more in POAG than in non-glaucoma compared to the studies mentioned above[12,15,34]. These studies differed in study populations. The subjects in Kiuchi et al’s[34]study were untreated normal tension glaucoma patients while subjects in this study were untreated POAG patients.
Hirooka and Shiraga[15]reported an average IOP increase of 4.0±0.2 mm Hg in POAG subjects and 3.1±0.4 mm Hg in normal subjects as they moved from sitting to supine position. The mean change in IOP was lower compared with the result of the present study. Their study and ours differed in sample size and study population. Their sample sizes were smaller and their glaucoma subjects were already on medications.
The limitations of the study were as follows: the IOP was measured at a specific period between 10:00 a.m. to 12:00 a.m. which may be affected by diurnal variation in IOP. POAG patients aged 30y and above who had a positive medical history of diabetics were excluded from the study. No test was done on those without a positive history to confirm that they were truly non-diabetic. Thus, it was possible that some diabetics had been included in the study.In conclusion, this study confirmed that posture induced IOP variation occurred in both glaucoma and non-glaucoma subjects. However, glaucoma subjects had greater increase in IOP variations associated with posture compared to nonglaucoma subjects. The degree of variation was observed to be lower in sitting compared with supine position. IOP upon adopting a supine position was observed to be lower when a thick pillow was used to elevate the head (supine with pillow) compared with supine flat position.
ACKNOWLEDGEMENTS
We wish to appreciate the entire staff of Ophthalmology Department of Alex Ekwueme University Teaching Hospital Abakaliki (AEFUTHA) for their immense support; the management of AEFUTHA where this study was conducted; Dr. Ginger-Ekeh, the Head of Ophthalmology Department; and all the consultants in the Department of Ophthalmology for their immeasurable support.
Conflicts of Interest: Ireka OJ,None;Ogbonnaya CE,None;Arinze OC,None;Ogbu N,None;Chuka-Okosa CM,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
