Severe Cytomegalovirus anterior uveitis and corneal endotheliitis after use of topical tacrolimus
Yukiko Tsubota, Yujiro Fujino, Kazuyoshi Ohtomo, Koji Ueda, Junko Yoshida,3, Takashi Miyai, Toshikatsu Kaburaki,4, Chihiro Mayama
1Japan Community Healthcare Organization Tokyo Shinjuku Medical Center, Tokyo 1628543, Japan
2The University of Tokyo Graduate School of Medicine, Tokyo 1130033, Japan
3International University of Health and Welfare Mita Hospital, Tokyo 1088329, Japan
4Jichi Medical University Saitama Medical Center, Saitama 3308503, Japan
Dear Editor,
Cytomegalovirus (CMV) uveitis is typically characterized by anterior segment inflammation with coin-shaped or linear keratic precipitates (KPs), mild cells and aqueous flare in the aqueous humor, corneal endothelial cell loss, and elevated intraocular pressure (IOP)[1-2]. Anti-CMV drugs are essentially effective in treatment of the disease[2], and concomitant topical steroids and/or more potent immunosuppressive medications are required to control inflammation in the most of the cases. However, excessive immunosuppressive treatment involves a risk of re-activation of the viral infection[3]. We experienced two cases of CMV anterior uveitis and corneal endotheliitis who presented with severe inflammation in the anterior chamber with massive broad pigmented KPs after the treatment using topical tacrolimus.
CASE 1
A 59-year-old Japanese man was referred to our clinic in 2018 with blurred vision and secondary glaucoma caused by anterior uveitis in the left eye. He had been diagnosed with scleritis in both eyes and rheumatism at another eye clinic, and treated with bilateral topical 0.1% betamethasone eye drops 4 times a IOP was 11 mm Hg in the right eye and 21 mm Hg in the left eye under topical anti-glaucoma medications. Open angle with no peripheral synechia in both eyes and increased pigment in the inferior angle of the left eye were found by gonioscopy, and iris atrophy or other pathological findings were absent in both eyes.
Systemic investigations including examination were performed. Serology for human immunodeficiency virus (HIV) infection were negative. Serum IgG antibodies, but not IgM antibodies, against herpes simplex virus (HSV), varicella zoster virus (VZV), and CMV were positive. At this time, under suspicion of HSV infection, systemic acyclovir (3000 mg/d) and topical acyclovir ointment 5 times a day were initially prescribed, and topical tacrolimus was discontinued and the aqueous humor from the left eye was collected.
One week later, the VA was decreased to 20/63 in the left eye and the results of the polymerase chain reaction (PCR) assay in the aqueous humor revealed CMV DNA but not HSV or VZV DNA in the affected eye. According to the clinical course and the PCR results, the case was diagnosed as CMV anterior uveitis and corneal endotheliitis and treated with oral valganciclovir (1800 mg/d) for a week and twice intravitreal injection of ganciclovir (1 mg). Topical instillation of twice daily 1% ganciclovir eye drops in addition to steroid and antiglaucoma drugs was continued.
The inflammation was gradually controlled by the treatment, and IOP was returned to the normal level in 2wk and the massive broad pigmented KPs disappeared in 3mo after that (Figure 2). However, the corneal endothelial cell density in the left eyes was decreased to 538 cells/mm2compared with that in the right eye, 2478 cells/mm2.
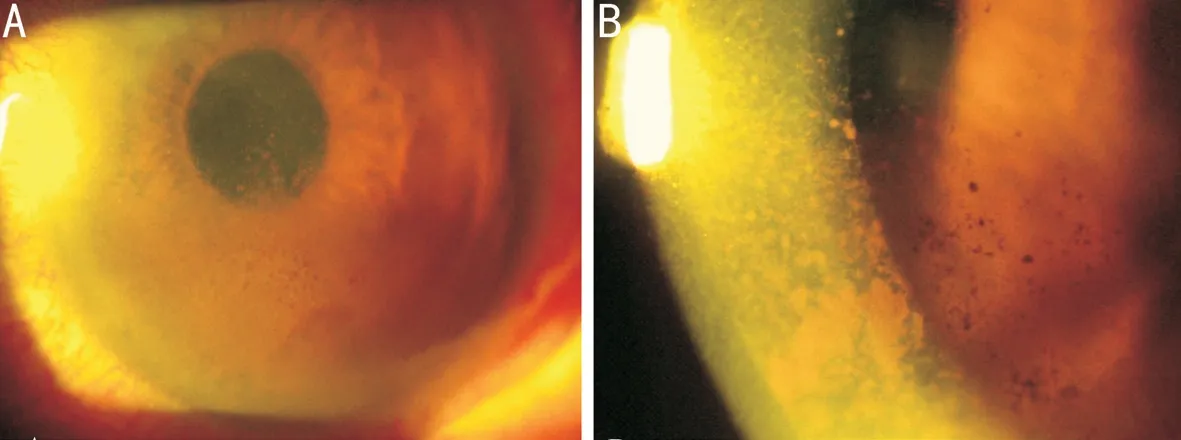
Figure 1 Slit-lamp photographs of the anterior segment of the left eye in Case 1 before administration of ganciclovir and valganciclovir showed the presence of moderate hyperemia of the conjunctiva, corneal epithelial edema, and highly pigmented keratic precipitates (KPs; A), and massive broad pigmented KPs in the inferior part of the cornea at higher magnification (B).

Figure 2 Slit-lamp photographs of the anterior segment of the left eye in Case 1 after 3mo’ treatment of ganciclovir and valganciclovir showed the absence of pigmented KPs.
CASE 2
The patient was a 64-year-old Japanese man with bilateral primary open angle glaucoma treated with topical medications since 1999 and he underwent trabeculectomy in the left eye in 2011. Mooren’s ulcer developed in the left eye in 2016, which was treated with topical 0.1% betamethasone eye drops 8 times a day, 0.1% tacrolimus eye drops 4 times a day, and systemic cyclosporine (400 mg/d). Five months later, he visited our clinic with a symptom of reduced VA in the left eye.
Slit-lamp examination revealed the peripheral corneal ulcer and massive broad pigmented KPs on the inferior half of the corneal endothelium similar to that of Case 1 and cell infiltration in the anterior chamber in the left eye (Figure 3A, 3B). Besides, moderate cataract and a thin, non-vascular, and pigmented filtration bleb at 11 o’clock of the limbus were observed (Figure 3C). The VA decreased from 20/63 to 20/100 in the left eye and IOP was 12 mm Hg without iris atrophy in both eyes, and corneal endothelial cell density was 1845 cells/mm2in the left eye. Blood examination and PCR test in the aqueous humor from the left eye were performed at this time. Serology for HIV infection were negative, and serum IgG antibodies, but not IgM antibodies, against HSV, VZV, and CMV were positive. According to the results of real-time PCR, 1.5×107copies/mL of CMV DNA were detected in the aqueous humor in the affected eye suggesting diagnosis of CMV uveitis. Topical tacrolimus and systemic cyclosporine were discontinued, and oral valganciclovir (900 mg/d for 3wk and 450 mg/d for another 3wk) was administered. Three months later, the real-time PCR test in the aqueous humor from the left eye was repeated and 1×104copies/mL of CMV DNA was detected. Oral administration of valganciclovir for 6wk was repeated and topical betamethasone was gradually reduced. Then inflammation in the anterior chamber was well controlled and CMV DNA was not found in the aqueous humor by the following real-time PCR test performed three months after that. However, the corneal endothelium was continuously decreased, and cataract surgery and corneal transplantation for bullous keratopathy were performed in the affected eye 6mo later.

Figure 3 Slit-lamp photographs of the anterior segment of the left eye in Case 2 before administration of valganciclovir showed the presence of intensive hyperemia of the conjunctiva, pigmented KPs, and Mooren’s ulcer (A), the massive broad pigmented KPs in the inferior part of the cornea (B), and a thin, non-vascular, and pigmented filtering bleb at the superior limbus (C).
DISCUSSION
CMV anterior uveitis and corneal endotheliitis in immunocompetent patients have typical clinical manifestations including slight conjunctival injection, mild anterior chamber inflammation, coin-shaped or linear KPs, absence of pupillary synechia, iris atrophy, increased IOP, and corneal endothelial cell loss[1-2], and they are prone to recurrence[4]. In addition to those findings, the results of PCR targeting CMV-DNA in the aqueous humor and effectiveness of antiviral drugs support the diagnosis of the disease[2].
In the present patients, both cases showed severe inflammation in the anterior segment with atypical massive broad pigmented KPs, and quantitative PCR performed in Case 2 revealed 1.5×107copies/mL CMV DNA in the aqueous humor, which is at the highest range of the PCR results reported in CMV anterior uveitis[5-8]. Higher copy numbers of CMV DNA are significantly associated with more severe IOP elevation and inflammation[5]. Chee et al[6]reported highly pigmented KPs in patients with corneal edema with high copy number of CMV DNA (1.1×104-2.3×107) after penetrating keratoplasty, which is consistent with the findings in Case 2.
Both patients in the current study had been previously treated with immunosuppressive drugs including topical steroid eye drops (4-8 times a day) and frequent tacrolimus eye drops (4-5 times a day for 4-6mo). Moreover, a thin peripheral cornea due to Mooren’s ulcer and a thin filtering bleb were present in Case 2, which increased the permeability of the topically administrated drugs into the anterior chamber.
Tacrolimus and cyclosporine are classified as calcineurin inhibitors, which suppress the immune cells’ activation by suppressing release of cytokines such as interleukin-2 by the T-lymphocytes. Tacrolimus is 10-100 times more potent in this effect than cyclosporine[9]and has lower corneal permeability[10], thus, topical tacrolimus is considered to be an effective and safer treatment option for extraocular or ocular surface inflammation. Twice daily instillation of 0.1% tacrolimus[11]or lower concentration of the drug[12]shows good treatment efficacy for allergic conjunctivitis. Additionally, topical tacrolimus is frequently prescribed for off-label use in intense treatment of patients with other extraocular inflammatory disorders such as scleritis or Mooren’s ulcer and to prevent graft rejection after corneal transplantation[13].
A previous study including 109 eyes of 106 patients with CMV endotheliitis reported that preceding topical steroid was used in 96.3% of the subjects at the time of diagnosis of CMV endotheliitis[2], and another case report described the development of CMV anterior uveitis after topical treatment with 0.05% cyclosporine A ophthalmic emulsion in patients with symptomatic dry eyes[3]. We observed the development of CMV anterior uveitis and endotheliitis after immunosuppressive treatment in both cases, and the severe inflammation was controlled by antiviral drugs and discontinuation of topical tacrolimus. In consideration of that CMV anterior uveitis developed hemilaterally in Case 1 though the amount of tacrolimus administration and other risk factors were equivalent in both eyes, and there was a five-month interval between the start of tacrolimus administration and development of CMV anterior uveitis in Case 2, the use of topical tacrolimus alone cannot account for the pathogenesis of CMV anterior uveitis. But we speculated that the immunosuppressive treatments including frequent and prolonged topical instillation of tacrolimus in both cases, accompanied with increased drug permeability in Case 2, may at least partly account for the development and severe presentation of CMV anterior uveitis with massive broad pigmented KPs.
Both patients of this study had been overdosed with topical 0.1% tacrolimus 4-5 times/day for 5-6mo. According to the previous report in the patients with ocular Behçet’s disease, the mean concentration of tacrolimus in the aqueous humor was 12.49 ng/mL after topical instillation of 0.3% tacrolimus 4 times/day for 3d, which is the sufficient therapeutic level for controlling ocular immune-mediated diseases[14]. Shoughy et al[15]recently reported the mean concentration of tacrolimus in the aqueous humor was 4.15 ng/mL after topical instillation of 0.05% tacrolimus every 1min for 5min in nonpathological eyes before cataract surgery. The results of these investigations suggest that frequently instilled 0.1% tacrolimus might be distributed in the aqueous humor at a pharmacological dose especially in the eyes with increased corneal permeability.
In conclusion, we experienced two cases of severe CMV anterior uveitis and endotheliitis with atypical massive broad pigmented KPs which may be correlated with preceding topical administration of tacrolimus. Discontinuation of tacrolimus and systemic and/or topical anti-CMV drugs were effective to control the inflammation even though the significant corneal endothelial cell loss progressed. Clinicians should be aware of the possibility of CMV anterior uveitis and endotheliitis in the eyes under immunosuppressive treatments including topical tacrolimus.
ACKNOWLEDGEMENTS
Conflicts of Interest:Tsubota Y,None;Fujino Y,None;Ohtomo K,None;Ueda K,None;Yoshida J,None;Miyai T,None;Kaburaki T,None;Mayama C,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
