Clinical observations of acute onset of myopic optic neuropathy in a real-world setting
Li Liao, Rui Fang, Fang Fang, Xiao-Hua Zhu
1Department of Ophthalmology, the Second Xiangya Hospital, Central South University, Changsha 410011, Hunan Province, China
2Changsha Aier Eye Hospital, Changsha 410015, Hunan Province, China
3Department of Orthopedics, the Second Xiangya Hospital, Central South University, Changsha 410011, Hunan Province, China
Abstract
INTRODUCTION
High myopia is very common and is one of the major causes of blindness, especially in East Asian countries[1]. Previous studies have shown that the number of myopia has increased year by year in parts of East and Southeast Asia, and by 2050, half of the world’s population will be affected[2].
However, no effective intervention is available to prevent the development of myopia[3]. It is clear that myopia may also cause progressive abnormalities in retinal nerve fibres. Ohno-Matsui[4]proposed that this myopic optic neuropathy is not found in emmetropic eyes. We found that retrobulbar glucocorticoid therapy effectively improved best corrected visual acuity (BCVA) in high myopia after cataract surgery. Therefore, we conducted a real-world study to observe the treatment effects of retrobulbar glucocorticoid therapy in myopia optic neuropathy patients. Real-world research is based on the actual conditions of patients who are not randomly chosen for treatment measures but are instead evaluated for a long time, during which attention is paid to treatment outcomes[5-9].
This original article aims to describe the clinical features of acute onset of myopic optic neuropathy and observe the effects of retrobulbar and systemic glucocorticoid therapy in a realworld research setting. These data are meaningful for further evaluating the external validity authenticity and security of treatments.
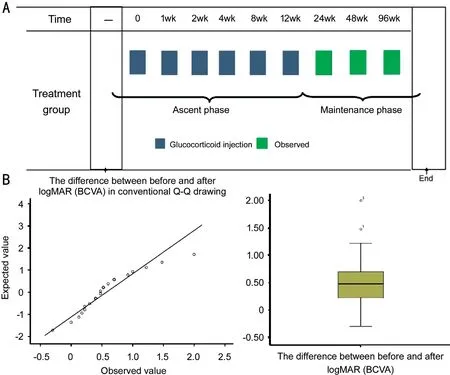
Figure 1 The treatment procedures of patients (A) and average BCVA change is 0.57 (95%CI 0.34-0.79) logMAR (B).
SUBJECTS AND METHODS
Ethic ApprovalThis article followed ethical guidelines that was approved by Ethics Committee of the Second Hospital of Central South University and the principles outlined in the Declaration of Helsinki (2008). We also have informed consent which was obtained from the subjects.
Patient InformationA total of 18 cases (22 eyes) of myopic optic neuropathy, including 11 females and 7 males, who were admitted to the Second Xiangya Hospital of Central South University between January 2000 and December 2017 were recruited. All eyes underwent a basic inspection, such as uncorrected visual acuity, optometry, or slit lamp and fundus examinations. Twelve eyes underwent a visual field (VF) examination, 11 underwent optical coherence tomography (OCT) examination, 10 underwent visual evoked potential (VEP) examination, 9 cases underwent a pupillary light reflex examination, and 9 cases underwent a fundus fluorescein angiography (FFA) examination; additionally, 3 cases underwent magnetic resonance imaging (MRI) examination, and 4 cases had AQP4 antibody detection[10]. Factually, we excluded any previous neurological episodes and any macular or retinal pathology in all eyes.
ImagingThe fundus color photography was performed using a TOPCON TRC-NW300, VF examinations were performed using a Humphrey Field Analyzer 860 perimeter, electrophysiological examinations were performed using a METROVISION MonpackONE, FFA was performed using Heidelberg fundus angiography system (HRA and HRAII; Germany), and OCT was performed using Heidelberg Spectralis-OCT (Germany).
MethodsAs mentioned, we selected retrobulbar and systemic glucocorticoid therapy. The former was the main treatment because it is widely prescribed for patients with cataracts or vitrectomy during the perioperative time[11]. In the real word, patients received a retrobulbar injection of dexamethasone (5 mg) once a week for 2 to 3wk and were then changed to triamcinolone acetonide (5 mg) once a month for 2 to 3mo. If someone who was in the early stages of disease development received systemic glucocorticoid treatment with methylprednisolone (500 mg), shock treatment was administered for 3d. The treatment procedures of patients are shown in Figure 1A.
Follow-upThe timepoints at which vision were evaluated at 1, 2wk, 1, 2, 3, 6mo, 1 and 2y. In some cases, regular checks (i.e., BCVA, VF, VEP and other examinations) needed to be performed. Findings were generally stable after 6mo of treatment, and the follow-up observation period was from 6mo to 2y. The time of each visit was determined by communication between the patient and the doctor.
Statistical AnalysisAll data analyses were performed using SPSS 22.0. Paired t-test was used for statistical difference analysis in our study. P<0.05 was considered statistical significance.
RESULTS
The age ranged from 14 to 72 years old (average, 44.09±3.86 years old). The duration of the disease was 2 to 21d (average, 10±2.1d). The range of spherical equivalent was -3 to -21 D(average, -8.46±1.30 D). There were 4 cases whose subjective visual acuity decreased in both eyes, and 14 cases in which it decreased in one eye (Table 1).

Table 1 Data from 22 eyes
The BCVA before treatment ranged from 2 (logMAR) in both eyes to 0 (logMAR). The average BVCA before treatment was 1.04±0.63, while BVCA after treatment was 0.47±0.57 (P<0.05; Figure 1B). In patients with a short course (within 1wk), recovery was fast and achieved the same BCVA as recorded before the onset within 6d. However, in patients with the long course (1 to 2wk), recovery was slow and did not achieve the BCVA recorded before the onset within 10d. These differences were statistically significant (P<0.01).
The average intraocular pressure (IOP) before and after treatment was 18.68±5.30 and 19.55±5.34 mm Hg (P>0.05). Patients with normal IOP less than 21 mm Hg accounted for 78%, and patients with IOP greater than 21 mm Hg accounted for 22%. For patients with IOP less than 20 mm Hg, the IOP fluctuates within 5 mm Hg and the maximum IOP does not exceed 25 mm Hg during local glucocorticoid therapy. The increase of IOP ranged from 5 to 16 mm Hg, with an average of 8.6 mm Hg, which was controllable to normal after local use of antiglaucoma drugs.
Twelve cases underwent VF examination before treatment. The VF showed abnormalities in bilateral eyes, including the spread of physiological blind spots, central and paracentral dark spots, and centripetal peripheral VF reduction; but central vision with no subjective changes. The average mean deviation (MD) before and after treatment was -11.46±7.05 and -8.05±5.44 dB (P<0.001). The average PSD before treatment was -6.19±3.64 dB, and after treatment was -5.28±3.09 dB (P>0.05).
There were 10 cases underwent VEP examination before treatment. The VEP was abnormal in all eyes with vision loss, and only one eye showed central vision without subjective changes before treatment. After treatment, BCVA was restored, and VEP was significantly improved.
There were 9 cases that underwent FFA examination before treatment. In addition to myopic retinal choroidal lesions, mild leakage was also observed in the optic disc in 3 eyes on FFA. On OCT or OCT angiography (OCTA), no neuropathy and no obvious abnormalities were found in the fundus macula. Pupillary reflex metrics were sensitive in most affected individuals. There were 9 cases of pupillary light reflex examination, and there were 2 pupils with poor light reflection. In the 3 evaluated cases, MRI examination results showed no obvious abnormalities. In 4 cases, serum AQP4 antibody detection was performed and showed no obvious abnormalities. Long-term follow-up observation showed no recurrence or serious complications.

Figure 2 Case 5 A: No obvious abnormalities observed on MRI; B: No obvious exudation was observed on OCT; C, D: Leakage at the temporal of optic disc was found on fluorescence fundus angiography; E: Fundus photos showed temporal optic disc was pallor.

Figure 3 Case 20 A: The reflex amplitude was similar in both eyes, although the right eye pupil light reflex was delayed and showed a weak systole ability. VEP showed the peak was delayed and the latency was slightly longer. B: The physiological blind spot expanded, and the centripetal vision narrowed in the VF of the right eye.
Typical Case Report
Case 5The visual acuity of the right eye was decreased for 8d in a 28-year-old woman with BCVA of 0.52 (logMAR) (Table 1, Figure 2). The VF measured 1y after retrobulbar glucocorticoid therapy showed a slight improvement. BCVA improved to 0 (logMAR). in the right eye at 12mo.
Case 20The visual acuity of the right eye was decreased for 2d in a 35-year-old woman with BCVA of 1.22 (logMAR). No obvious exudation or abnormal neovascularization was observed on OCT or OCTA. The BCVA improved to 0 (logMAR) in the right eye at 34d (Table 1, Figure 3).
DISCUSSION
As previously noted, the aetiology of myopic optic neuropathy has remained unclear. This group of patients had no obvious cause of acute onset, such as general inflammation and immune lesions[12]. Glucocorticoid therapy was effective, indicating that the symptoms cannot be explained from the perspective of degeneration. If it was inflammatory change, the patients would have presented clinical signs and symptoms such as retrobulbar pain. Freund et al[13]reported observing intrachoroidal cavitation (ICC), which appeared as a yellowish orange lesion around the myopic conus and was located within the choroid, and suggested it might also be related to glaucomatous VF defects in non-myopic eyes. According to this study, the development of ICC and subsequent defects of inner retina are considered an important cause of VF defects in eyes with pathologic myopia. Park et al[14]prompted us to consider that an enlarged globe with tight lid may cause the eyeball to become compressed, thus elevating episcleral venous pressure, and this may also explain the mechanism underlying optic nerve damage in some patients. As Jonas et al[15]reported, simple mechanical disruption of retinal nerve fibres and increased susceptibility to developing glaucoma share a complicated relationship with pathological myopia. According to Ohno-Matsui et al’s study[16], the VF defects observed in this condition are progressive, and multiple regression analyses showed that the presence of an abrupt change in scleral curvature was the only factor that was significantly associated with the progression of VF defects.
Nonetheless, we found that glucocorticoid therapy was effective in this eye disease, and by examining individuals in a real-world setting, we found that post-bulbar glucocorticoid therapy is effective for neuropathy which is similar to openangle glaucoma in the VF. We suspect an atypical inflammatory response, which is associated with immune factors but not glaucoma. Chen et al[17]proposed that glaucoma is a curable immune system disease and T cells are the cause of optic nerve degeneration in glaucoma. However, we hypothesize that myopic optic nerve disease is a type of immune system disease that is not very serious, and the specific mechanism underlying it is not clear. In summary, the pathogenesis of acute onset of myopic optic neuropathy remains unknown.
Our research demonstrates that acute onset of myopia optic neuropathy is a rare disease with acute visual impairment and latent visual dysfunction. The course of the disease is generally approximately 2wk, and visual function is seriously impaired during this period of time. Other characteristics of this disease include involvement of both eyes and an acute onset with rapid visual decline. Acute onset of myopic optic neuropathy patients is predominantly female, and onset generally occurs in the young and middle-aged individuals with moderate to high myopia. The condition is characterized by persistent lesions, a lack of self-healing and self-limitation of the disease, but it is reversible with proper treatment. Some patients had no subjective vision loss but instead endured only frequent paroxysmal amaurosis.
The results obtained in fundus examinations of patients showed that the optic cup to disc ratio was relatively large. Furthermore, its colour was slightly lighter but not pale. In addition to myopic retinal choroidal lesions, mild leakage in the optic disc was also observed in 3 eyes on FFA. FFA demonstrated that progressive elongation of the globe was associated with posterior pole findings, including tilted disc, posterior staphyloma, geographic atrophy of the retinal pigment epithelium (RPE), Fuchs spots, attenuation of the RPE and choroid, mottling of the RPE, lacquer cracks, and peripapillary atrophy of the RPE and choroid in patients with high myopia[18-19]. In addition to the original myopia lesions, the other areas of the fundus showed no specific changes. VEP was abnormal in all eyes with vision loss and in only one eye with central vision loss and showed no subjective changes from results obtained before treatment. In most patients, the VEP showed that peaks were delayed and the latency was slightly longer. Briefly, a VF-related characteristic of myopic optic neuropathy was the spread of physiological blind spots in addition to non-specific changes, such as central and lateral central dark spots and centripetal peripheral VF reduction[20-21]with abnormal VF at the other eye without visual loss. Changes in VEP and VF were similar to those observed in idiopathic optic neuropathy and indeed showed no specificity. After treatment, VF significantly improved. We have found VF was abnormal in both eyes but VF was also improved at the other eye with local treatment at one eye. There was no conclusive evidence indicating that treatment exerted a benefit in terms of changes in optic nerve fibre thickness and blood flow values on OCT. MRI examination showed that mild changes occurred in 2 cases. There were 4 cases with serum AQP4 antibody detection, which showed no obvious abnormalities. There were no changes in inflammatory demyelinating and multiple sclerosis pathological by MRI, VEP, and NMO-IgG.
The effects of retrobulbar and systemic glucocorticoid therapy were extraordinary. The findings presented here regarding the effectiveness of glucocorticoid in treating acute onset of myopia optic neuropathy are based on real-word methods. When MD value is <-4 dB, intervention can rapidly improve abnormal VF. It is amazing that once retrobulbar glucocorticoid therapy was used, not only BCVA but also VF was clearly improved. Moreover, we noted that the speed of recovery was related to the course of the disease and show that this condition is different from ischaemic optic neuropathy[22]in that a shorter disease course was associated with a faster recovery. Subjective recovery of central vision in a disease with a longer course occurred slightly slower. When central vision was subjectively restored to its original state, the VF still showed a slight change with regard for the physiological blind spot. This type of optic nerve dysfunction does not often relapse. In summary, a conclusive treatment benefit was associated with retrobulbar and systemic glucocorticoid therapy in that the eyes returned to normal visual acuity in the VF based on the evaluations included in this study.
We have done our best to provide comprehensive results of eye and body examinations, but the observation time was too long, and some data were missing. Moreover, considering the degree of patient cooperation and economic conditions in the setting used in this study, not all patients had undergone all tests, such as MRI, FFA, VEP, pupillometry, anti-AQP4, autofluorescence, and OCTA. In fact, we performed all the examinations on only a few typical patients, and the results were negative. Unfortunately, we found no systematic evidence to describe colour vision, contrast sensitivity and relative afferent pupillary defect (RAPD), which are important tests for excluding glaucoma. No controlled trials have yet addressed the issue of what to do if BCVA fails to improve in affected patients. We are sorry we were not able to include a control group because there were so few patients even though we have been exploring this issue for more than a decade. It is a pity that part of the data was lost.
In conclusion, in a real-word setting, acute onset of myopic optic neuropathy is rare and occurs predominantly in females, young, and middle-aged adults with moderate to high myopia. Another characteristic of this disease is that binocular lesions may occur simultaneously or sequentially, and the acute onset of visual decline is rapid. Changes in VEP and VF are similar to those found in idiopathic optic neuropathy and indeed show no specificity. The subjective recovery of central vision is slightly slower when the disease runs a longer course. When central vision is subjectively restored to its original state, the VF still shows a slight change with regard for the physiological blind spot. If one eye is treated, the BCVA and VF of the other eye will also improve. Retrobulbar and systemic glucocorticoid therapy exerted a significant effect, and recovery after treatment was also fast after treatment in a real-world study. This type of optic nerve condition does not often relapse. The pathogenesis of acute optic neuropathy remains unclear, but it is likely to be related to immunity. We hope that more researchers will pay attention to this type of disease to improve our ability to prevent high myopia.
ACKNOWLEDGEMENTS
Conflicts of Interest: Liao L,None;Fang R,None;Fang F,None;Zhu XH,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
