lntracameral anti-VEGF injection for advanced neovascular glaucoma after vitrectomy with silicone oil tamponade
Ling Bai, Farheen Tariq, Yi-Dan He, Shu Zhang, Feng Wang
1Department of Ophthalmology, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710003, Shaanxi Province, China
2Experimental Teaching Center for Clinical Skills, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710003, Shaanxi Province, China
3Department of Geriatric Medicine, the Second Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710003, Shaanxi Province, China
Abstract
INTRODUCTION
Neovascular glaucoma (NVG) is a devastating type of secondary glaucoma. It is caused by the formation of abnormal new blood vessels, which impede normal drainage of aqueous from the anterior segment of the eye[1]. It can be associated with ischaemic retinopathies such as central retinal vein occlusion (CRVO) or proliferative diabetic retinopathy (PDR). Vascular endothelial growth factor (VEGF) is one of the most important proangiogenic factors, its expression is enhanced by ischemic retina, and its level is significantly elevated in aqueous humor and vitreous of patients with NVG[2-3], so anti-VEGF agent intraocular injection is an option for the treatment for NVG[4-6].
Some patients with complex retinopathy have to undergo vitrectomy with silicone oil tamponade. In the presence of silicone oil, the delivery and concentration of drugs injected into the ocular become unpredictable. Previously few studies have used anti-VEGF agent through the intravitreal route in silicone oil tempande eyes for the treatment of NVG. None of these studies have data recorded for the advanced stage of NVG[7-8]. Conbercept is a new anti-VEGF agent; it has been proved to be the right candidate in the treatment of NVG in our previous study (unpublished data). This study aimed to evaluate the safety and efficacy of intracameral conbercept injection for the treatment of advanced NVG (stage III) after vitrectomy and silicone oil tamponade.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the medical ethics board of the Second Affiliated Hospital of Xi’an Jiaotong University and complied with the Declaration of Helsinki. Informed consent was signed by all patients prior tostudy enrollment. The study was registered at clinicaltrials.gov (NCT03154892).

Table 1 The patients’ information
PatientsFive patients (5 eyes) of NVG stage III were recruited in this study at the Department of Ophthalmology, the Second Affiliated Hospital of Xi’an Jiaotong University. All participants had undergone vitrectomy and silicone oil tamponade for the treatment of PDR or CRVO.
Intracameral Conbercept InjectionUnder topical anesthesia with 0.5%, proparacaine hydrochloride eye drops, the conbercept (Chengdu Kanghong Biotech Ltd, Sichuan, China) 0.5 mg/0.05 mL injection was performed through a 30-gauge needle at corneal limbus into the anterior chamber. This procedure was assisted by a surgical microscope and did not need extra anterior chamber paracentesis.
Pan-retinal PhotocoagulationPan-retinal photocoagulation (PRP) was performed under a slit lamp using a LIGHTMED 577 wavelength fundus laser machine. The spot size was 300 microns, level II to III reaction for retinal photocoagulation was appropriate. Usually, PRP was completed within one week. The setting for total photocoagulation was 1500-2000 spots. If the eye had got PRP before, extra-pan-retinal photocoagulation (E-PRP) of 2000-2500 spots, and especially approaching ora serrata, was completed.
Ophthalmic ExaminationsAt the initial time, patients underwent the following set of examinations: best-corrected visual acuity (BCVA) with Snellen chart, intraocular pressure (IOP) by Goldman applanation tonometer, slit lamp examination for the anterior segment, and neo-vessel at iris (NVI) grade, gonioscopy, and detailed fundus examination. The patients were observed on the first and the second day after conbercept injection. On the second day after injection, all patients underwent trabeculectomy with mitomycin C[9], then promptly completed PRP or E-PRP. Patients were followed up every month for at least 6mo (Figure 1).
RESULTS

Figure 1 The therapeutic regimen for advances NVG after vitrectomy with silicone oil tamponade.
The patients’ characteristics were shown in Table 1. The NVG developed 4-8mo after vitrectomy with silicone oil tamponade[10]. Within 2d after conbercept intracameral injection, we can achieve good IOP control and NVI regression. The mean IOP before injections was 50.4±6.39 mm Hg (range 42-58 mm Hg) despite maximum anti-glaucoma therapy. On the first day after conbercept injection, the IOP decrease to 21.6±2.3 mm Hg, and the NVI regressed obviously (from grade 4.60±0.55 to 0.80±0.45). On the second day, the IOP slightly increased to 26.0±2.65 mm Hg, the NVI in No.3 patient regressed completely, the other eyes were the same as the first day (grade: 0.60±0.55). Because the IOP had an increasing tendency, trabeculectomy with mitomycin C was conducted on this day, then PRP/E-PRP was completed promptly.
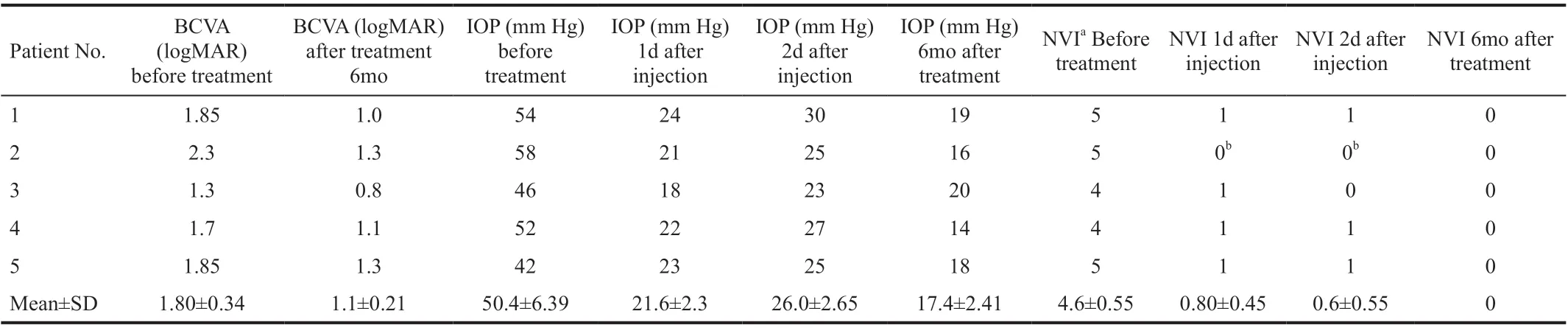
Table 2 BCVA, IOP, and NVI before and after treatment
At the end of follow up time (6mo after injection and surgery); BCVA (logMAR) improved in all eyes (1.80±0.34 vs 1.1±0.21), IOP decreased and returned to normal level (50.4±6.39 mm Hg vs 17.4±2.41 mm Hg), and the NVI completely disappeared (grade 4.6±0.55 vs 0; Table 2)[11].
Hyphema happened in No.2 patient during intracameral conbercept injection. We performed anterior chamber irrigation during trabeculectomy. Finally, the patient got improved visual acuity after treatment. None of the eyes happened hyphema during and after trabeculectomy. No NVI recurrence was observed during the followed-up period.
DISCUSSION
Our study indicated that intracameral injection of conbercept is safe and effective, and it may be the better option for patients with advanced NVG after vitrectomy with silicone oil tamponade. To reduce the risk of perioperative hyphema, we recommend to finish trabeculectomy within 2d after injection.The progression of NVG can be divided into three stages. At the advanced stage (stage III), contraction of the fibrovascular membrane produces peripheral anterior synechiae (PAS), the angle is closed. Patients suffered abrupt high IOP, severe pain, and eventually irreversible optic nerve damage and blindness. Because the angle of the anterior chamber cannot be opened again, usually anti-glaucoma surgery is necessary to control the IOP in this stage. Because of high IOP and massive NVI/(NVA), perioperative hyphema is a common complication and is associated with higher rates of surgery failure[12-13].
The implement of anti-VEGF agents in the treatment of NVG has been generally accepted[14]. Currently, available anti-VEGF agents are composed of monoclonal IgG antibodies (ranibizumab and bevacizumab) and recombinant fusion proteins (conbercept and aflibercept)[15]. The latter one can block not only all VEGF-A isoforms but also VEGF-B and placental growth factor (PGF), thus should have a much higher anti-VEGF effect than monoclonal IgG antibodies. Our previous study also showed a good effect of conbercept in the treatment of NVG (unpublished data). NVG in the vitrectomized eye with silicone oil tamponade is a rare condition; the advanced stage makes it much worse for the treatment.
VEGF inhibitors were usually injected through intravitreal routes[16-17]. Just until now, only two papers about its use in silicone oil tamponade eyes could be searched from PubMed. Salman[7]reported intra-silicone injection of 1.25 mg/0.05 mL bevacizumab (conventional dose of intraocular injection) was safe and effective in the treatment of NVG stage I, but no advanced stage was recorded. Falavarjani et al[8]reported intrasilicone injection of double dose bevacizumab (2.5 mg/0.1 mL)was effective in the treatment of NVG after vitrectomy in 5 eyes, and recurrence occurred in one eye at ten weeks after injection. But as for the cardiovascular events and bleeding risk with bevacizumab intraocular use[18], we still think the double dose injection of bevacizumab into the eyes is dangerous. We once tried intra-silicone injection of 1.25 mg/0.05 mL bevacizumab for 2 stage III NVG patients with silicone oil tamponade; after seven days of observation, there was no obvious regression of NVI, and the IOP was still in a high level (data not shown in this paper). Thus, we prefer to find a better way to treat stage III patients with silicone oil tamponade.
For the patients in NVG stage III, the first task was to decrease IOP to prevent irreversible optic nerve damage. Bhagat et al[19]reported intracameral route was more effective in terms of control IOP than the intravitreal route for NVG, but in the presence of silicone oil tamponade, there was no report about intracameral injection yet. In this study, we tried to inject the recommended dose of conbercept through the intracameral route; the results were exciting. NVI regressed obviously, and the IOP decreased markedly on the first day after injection, and the IOP tended to increase on the second day. We performed trabeculectomy with mitomycin C on the 2nd day after injection, and there was no intra-operation or post-operation hyphema. We chose trabeculectomy just because it had been verified to have a similar success rate when compared to the Ahmed glaucoma valve in NVG[20]and was quite a costeffective option. All patients completed PRP within one week after surgery. For 2 patients with PRP history, we did additional E-PRP to minimize retinal oxygen consumption. The BCVA was improved, the IOP was all in the normal range, and the NVI was completely disappeared at the end of follow-up time.As we observed before, hyphema could not be avoided for the intravitreal injection route in NVG stage III because anterior chamber paracentesis was necessary at the end of intravitreal injection to decrease IOP[1,14]. Hyphema occurred only in one patient in the process of intracameral injection due to the sudden decrease of IOP. We performed anterior chamber irrigation during trabeculectomy; no more hyphema happened during and after surgery. The patient finally got improved visual acuity (typical case).
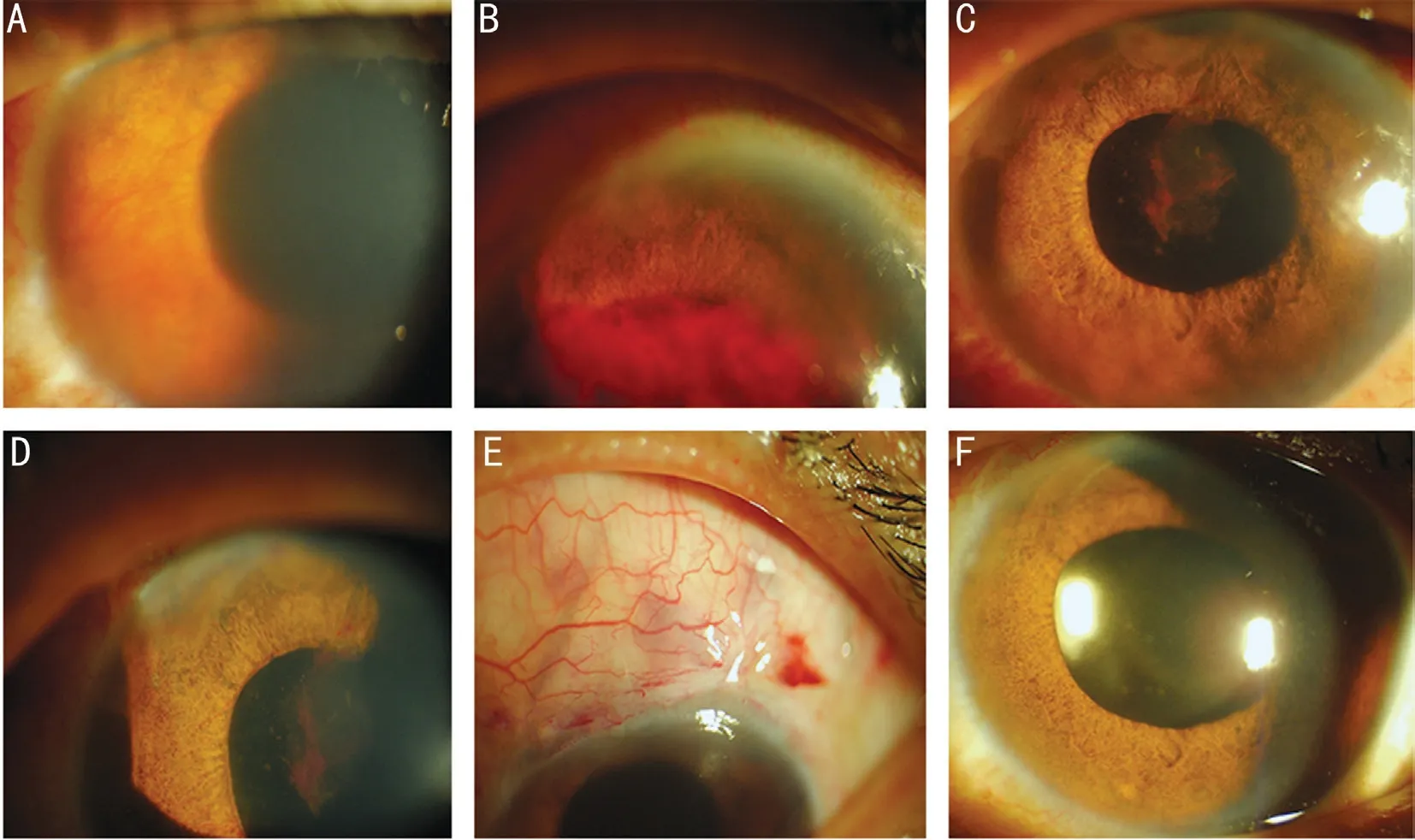
Figure 2 Ophthalmic examination of the typical case A: At the initial stage, edema occurred in the cornea, there was obvious NVI in the iris, IOP was 58 mm Hg; B: Hyphema was presented on the 1st day after conbercept anterior chamber injection, but the cornea was clear, NVI disappeared at the visible superior iris, and IOP was 21 mm Hg; C-E: One day after trabeculectomy with mitomycin C plus anterior chamber irrigation, hyphema was almost disappeared, there was only slight residual NVI, and the filtering bleb was diffused; F: Six months later, the cornea was clear, and no neovessels could be found on the iris or in the angle.
Due to the advanced NVG after vitrectomy with silicone oil tamponade is a fairly rare condition, statistical analyses could not be conducted with small sample size and the absence of the control group. Larger studies with longer follow-up are required to further validate these findings.
Typical caseA 48-year-old man had vitrectomy with silicone oil tamponade in the left eye for 7mo and complained of pain for one month. Seven months before, he suffered a blurry vision in the left eye and got vitrectomy with silicone oil tamponade for the treatment of CRVO and vitreous hemorrhage at another hospital. One month ago, he felt pain in the left eye and got three topical hypotensive eye drops to control IOP. But he complained the severity of pain increased gradually, and finally came to our department. The physical examination showed that the visual acuity was hand movement, the cornea showed edema, the pupil was 5 mm with slow light reflex, and the iris had pronounced NVI. Under maximal medication, the IOP was still 58 mm Hg. Because of the corneal edema, the fundus was not clear. At the initial time, 0.5 mg conbercept was injected into the anterior chamber. When the needle pulled out, hyphema happened. One day later, the cornea was clear, IOP was 21 mm Hg, and NVI disappeared at the visible superior iris. On the second day, IOP increased to 25 mm Hg. Then we performed trabeculectomy with mitomycin C, combined with anterior chamber irrigation during surgery. No hyphema occurred again. One day later, the patient had diffused blebs, clear cornea, 12 mm Hg of IOP, and tiny residual NVI. Then PRP was completed promptly within one week. Six months later, visual acuity was 0.05, IOP was 16 mm Hg, the cornea was clear, and no neovessels could be found on the iris or in the angle (Figure 2).
ACKNOWLEDGEMENTS
Authors’ contributions: Zhang SandWang Fdesigned the study.Bai L,Tariq F, andHe YDcarried out the measurements.Bai LandTariq Fwrote the manuscript.Zhang SandWang F, together withBai L, were involved in the analysis of the results and further revision of the manuscript. All authors have read and approved the manuscript.
Foundation:Supported by the Natural Science Foundation of Shaanxi Province (No.2017JM8032).
Conflicts of Interest: Bai L,None;Tariq F,None;He YD,None;Zhang S,None;Wang F,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
