Auricular cartilage versus donor sclera as a wrapping of hydroxyapatite orbital implants
Ying-Jie Ma, Xiu-Ying Zhu, Ben Chen, Yan-Yan Lin, Jia Liu, Xi Chen
Department of Orbit & Oculoplastic Surgery, Eye Hospital of Wenzhou Medical University, Wenzhou 325000, Zhejiang Province, China
Abstract
INTRODUCTION
The cosmetic results of simple enucleation are always poor because of the immobile staring appearance and tendency of lower lid sagging which would lead to a deep hollow below the brow. This outcome can be considerably improved by placing an orbital implant to fill the volume of the lost eye[1].
The hydroxyapatite (HA) porous implant was the most widely used type of orbital implant due to its good biocompatible (minimal tissue inflammation) and low resorption (rapid host tissue ingrowth)[2-3]. However, the surface of porous implants may be abrasive to the orbital soft tissue above, which would potentially cause tissue erosion with implant exposure. Thus this porous implants would increase the risk of orbital implant exposure[4-5]. Wrapping the implant could physically add another layer of tissue between the implant and overlying conjunctiva, thus to decrease the incidence of implant exposure and provide a surface for muscle attachment as well[6].
Donor sclera has been used widely as the wrapping material of HA implants[7-8]. Although donor sclera kept unchanged in most cases, late thinning or entirely disappearing was happened in some cases[9]. This late thinning or disappearing of the sclera over unorganized implants could cause spontaneous rupture of the conjunctiva with exposure of the unorganized implant[9]. Also, it has been proved that current screening tests may miss an infected blood donor 1:1 800 000 for HIV, 1:1 200 000 for hepatitis C virus, 1:200 000 for hepatitis B virus and Creutzfeldt-Jakob disease (CJD)[10-12]. What’s more, donor sclera which needs to be preserved in the eye bank, may be unavailable sometimes especially in case of an emergency. This possibly happening of late thinning, infectious disease spreading and occasional unavailability of donor sclera has prompted the use of other alternative wrapping materials.
Auricular cartilage is the autogenous material which shares various characteristics with donor sclera[13-14]. It has been used for lots of oculoplastic procedures including as a substitute of tarsal plate for reconstruction of full-thickness eyelid defect, as a spacer for upper and lower eyelid retraction correction, and as a support of nasal tip in rhinoplasty[14-16].
This study aimed to compare postoperative outcomes after primary enucleation and placement of the HA implant without any wrapping, with auricular cartilage cap or donor sclera cap.
SUBJECTS AND METHODS
Ethical ApprovalThis retrospective study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Eye Hospital of Wenzhou Medical University (Medical Ethics Committee, Wenzhou Medical University, Wenzhou, Zhejiang Province, China). Informed consent was obtained from all the patients.
Patients were eligible for inclusion if they had been diagnosed with intraocular tumor or severe ocular injurychronic dacryocystitis and elected to undergo surgical treatment enucleation and HA orbital implantation.
Patients were excluded when they were <18 years old or >65 years old, had lid malposition, unable to tolerate general anesthesia, with systemic autoimmune disease, needing radiotherapy or chemotherapy after surgery, and follow-up period <12mo.
We record the age, gender, eye, the cause of enucleation, size of implant, and the surgical type (autogenous ear cartilage cap, donor sclera cap, without wrapping material) of all patients. The complications, its occurrence time, subsequent therapy, and prognosis were recorded as well. A total of 32 patients meet our criteria. These cases were divided into 3 groups (groups A, B, C) according to the wrapping material of HA implant. Cases with autogenous ear cartilage caps were enrolled in group A, with donor sclera caps were enrolled in group B, without any wrapping material were enrolled in group C.
All of the procedures were conducted under general anesthesia by a single surgeon (Chen X). A piece of autogenous ear cartilage graft, 15×15 mm2in size, harvested from the conchal lateral wall through a post-auricular incision of the right ear and then be preserved in a mixture of gentamicin and normal saline (Figure 1A, 1B). Alcohol-preserved sclera provided by Eye Bank of Eye Hospital of Wenzhou Medical University was used in group B cases. After 360 degree conjunctival peritomy, 4 rectus were isolated and suspended with 6-0 vicryl suture [Alcon (China) Ophthalmic Product]. The inferior and superior oblique were cut after clipping. Then the transection of the optic nerve was performed followed by application of pressure for hemostasis. A sizing ball was used to evaluate the residual intraconal volume, and implant size was chosen to allow tension-free closure of the anterior ocular tissue. The HA implant (Bio-Eye; Integrated Orbital Implant) was placed in the cone after soaking in a mixture of gentamicin (80 000 units), hexadecadrol (1 mL:5 mg) and normal saline for 5min (Figure 1C). Autogenous ear cartilage (group A; Figure 1D) or donor sclera (group B) was then sutured to wrap the frontal part of the implant. Muscles were sutured to attach at the recti normal anatomical insertion sites with 6-0 vicryl suture [Alcon (China) Ophthalmic Product; Figure 1E]. The rectus were imbricated anterior to the HA implant in group C cases as Guthoff RF’s method. The superior and inferior rectus muscles, as well as the medial and lateral rectus muscles, were respectively knotted together forming a joint-like structure between the anterior part of the HA implant and the Tenon’s capsule[17]. Tenon’s tissue was then closed with multiple interrupted 6-0 vicryl sutures and conjunctiva was closed with a continuous 6-0 vicryl sutures (Figure 1F). A conformer was placed in conjunctival sac with antibiotic ointment. Pressure bandaging was applied for 3d after surgery. Postoperative care included administering methylprednisolone (20 mg/kg/d) for 3d and ceftriaxone (1.0 g/d) for 3d. Topical tobramycin dexamethasone (Alcon, ophthalmic ointment) was prescribed for 1mo after removing the bandage.
Follow-up period was set at 1, 2wk, 1, 3, 6, and 12mo after surgery. At each follow-up, complications including the existing of implant exposure, conjunctival inclusion cysts, conjunctive granuloma, and severe conjunctive chemosis were recorded. For cases with intraocular tumor before surgery, orbital magnetic resonance imaging (MRI) was performed to evaluate the possibility of residual tumor. Statistical analyses were performed with SPSS version 19.0. The demographic data of 3 groups were compared using the one-way ANOVA or Chi test or Fish’s test. Results were considered significant at P<0.05.
RESULTS
In total, 32 cases finished the follow-up and were enrolled in this study, including 11, 12, and 9 cases in group A, group B and group C, respectively. The clinical characteristic of them were list in Table 1.
No statistically significant differences were identified in patients age (P1-2=0.621, P1-3=0.628, P2-3=0.980), gender (P1-2=0.680, P1-3=0.374, P2-3=0.659), eye (P1-2=0.292, P1-3=1.0, P2-3=0.670), cause of enucleation (P1-2=0.590, P1-3=1.0, P2-3=1.0), and the size of implant (P1-2=0.573, P1-3=0.907, P2-3=0.515) among 3 groups.
Altogether 3 cases (27.27%) in group A developed complications after surgery, 4 cases (33.33%) in group B, and 4 cases (44.44%) in group C. All cases with complications developed only one complication.
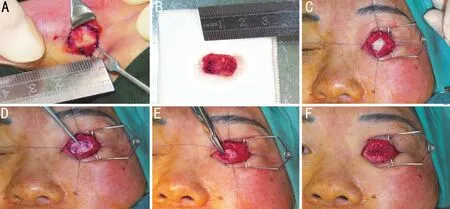
Figure 1 The surgical procedure of enucleation and HA orbital implantation with an auricular cartilage cap A, B: Autogenous ear cartilage graft was harvested from the conchal lateral wall through a post-auricular incision as a rectangular strip of the right ear and be preserved in a mixture of gentamicin and normal saline; C: The HA implant was placed in the cone after soaking in a mixture of gentamicin, hexadecadrol and normal saline for 5min; D: Autogenous ear cartilage was then sutured to wrap the frontal part of the implant; E: Muscles were sutured to attach at the original place; F: Tenon’s tissue was then closed with multiple interrupted 6-0 vicryl sutures and conjunctiva was closed with a continuous 6-0 vicryl sutures.
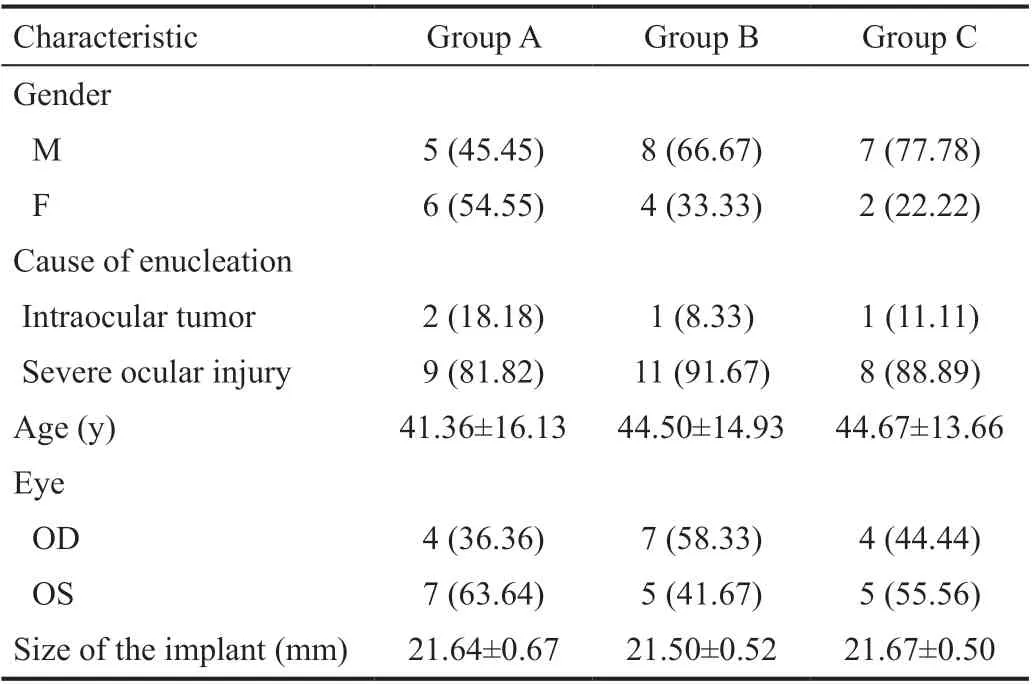
Table 1 Clinical characteristic of patients n (%)
No HA exposure (0) occurred in group A (Figure 2). One case (8.33%) developed HA exposure (1×1 mm2) in group B at 1y follow-up. It is a 65-year-old man who had never taken out the ocular prosthesis after surgery. The exposure developed at 12mo after surgery and was recovered with conservative treatment. One case (11.11%) developed HA exposure in group C at 6mo follow-up. It is a 31-year-old man and was treated successfully with conservative treatment as well.
Of the 11 patients in group A, three cases (27.27%) developed mild complications, including one conjunctival inclusion cysts and two severe conjunctive chemosis. Of the 12 patients in group B, three cases (25%) developed mild complications, including one conjunctival inclusion cysts, one severe conjunctive chemosis, and one conjunctive granuloma. Of the nine patients in group C, three cases (33.33%) developed mild complications, including one conjunctive granulation and two severe conjunctive chemosis (Table 2).

Figure 2 Photograph taken at 12mo follow-up in one patient with an auricular cartilage cap. No exposure was occurred.

Figure 3 Axial T2 scan through the orbits of a 63-year-old patient 12mo after enucleation and HA orbital implant with auricular cartilage cap in left eye The HA implant showed an increased T2 signal centrally (black arrow). The auricular cartilage cap shows as a linear area of intermediate signal in front of HA implant (white arrow).
At 12mo follow up, the MRI showed good shape and position of autogenous ear cartilage in cases with intraocular tumor before surgery in group A (Figure 3).
DISCUSSION
In this study, we report our experience using auricular cartilage or human donor sclera to cover enucleation implants. This is the very first time using auricular cartilage as the wrappingmaterial of implant. The incidence of exposure in patients receiving auricular cartilage cap, donor sclera cap and without any wrapping material were 0, 8.33%, and 11.11% respectively. The incidence rate of mild complications, including conjunctival inclusion cysts, severe conjunctive chemosis, and conjunctive granuloma, were 27.27%, 25%, and 33.33% in patients with auricular cartilage cap, donor sclera cap, and without wrapping cap. Although no statistically significant difference was found among 3 groups (mainly due to small sample size), the incidence rate of exposure was lowest in cases with auricular cartilage cap, followed by cases with donor sclera cap. The incidence of mild complications was lower in patients with wrapping material, either auricular cartilage or donor sclera.
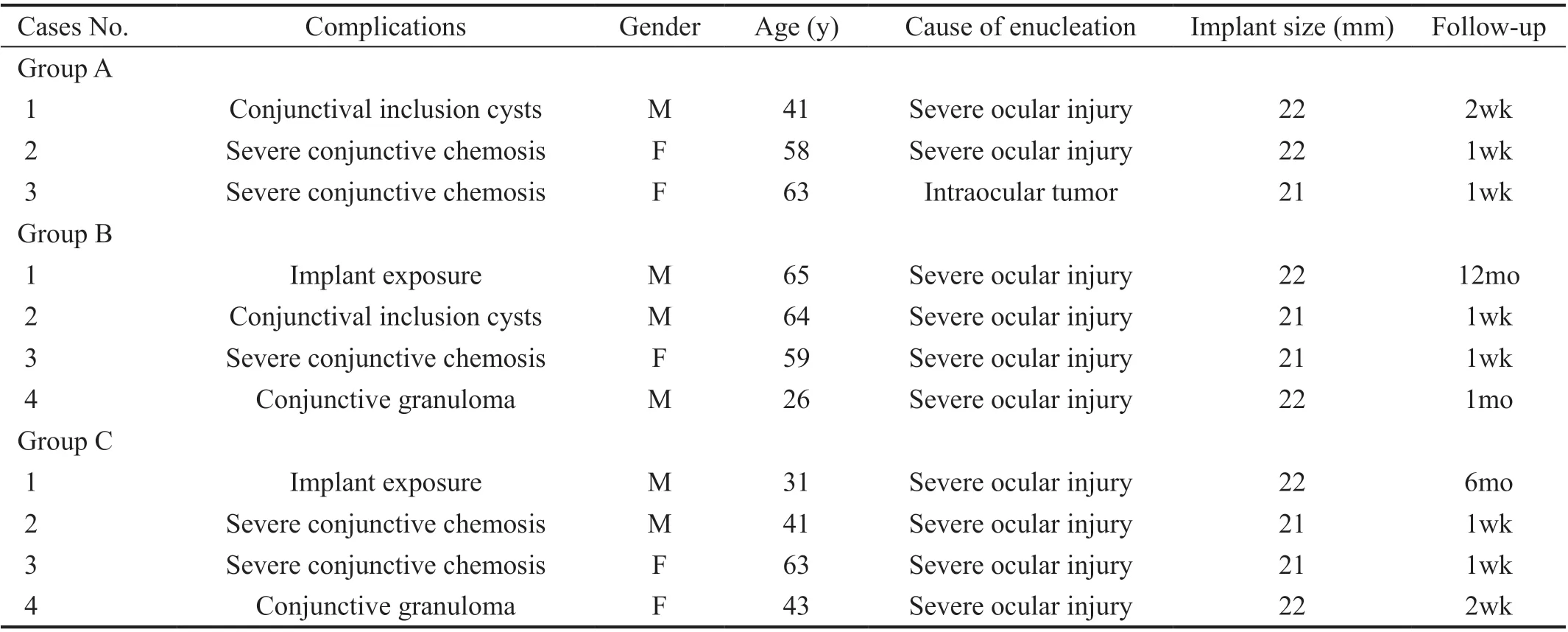
Table 2 The clinical data of patients with complications in three groups
The cosmetic results of simply enucleation are always poor. Therefore placing an orbital implant would be the necessary procedure in most cases to improve the appearance. However, implant exposure is the main complication after it, which could lead to poor prognosis. Rates of HA implants were reported to range from 9.6% to 28%[3,18-19]. The factors of development of exposure could mainly be categorized into 3 groups: implant related, patient related, and surgery related[20]. Thus, factors such as poor surgical technique, excessively large size of implant, and implant infection play important roles in implant exposure[21].
In this study, we excluded patients <18 years old or >65 years old, with systemic autoimmune disease or needing radiotherapy or chemotherapy after surgery, thus to remove patient-related factor. All surgical procedure was performed by a single experienced surgeon (Chen X). A sizing ball was used during surgical procedure to evaluate the residual intraconal volume, and implant size was chosen to allow tension-free closure of the anterior ocular tissue. This procedure could prevent the usage of excessively large implant. Also, the averages of the implant size were 21.64±0.67, 21.50±0.52, and 21.67±0.50 mm in 3 groups respectively. No statistically significant differences were found among 3 groups. The factors related to poor surgical technique and excessively large size of implant were excluded as well.
Wrapping the implant was believed to significantly decrease the incidence of implant exposure by adding another layer of tissue between the implant and overlying conjunctiva[6]. We found higher exposure rate in cases with no wrapping material than cases with wrapping cap. Besides, for cosmetic purpose, it is essential not only to correct the tissue defect of these cases by inserting an orbital implant, but also to ensure the movement of ocular prosthesis. The wrapping material could provide a surface for muscle attachment which would ensure the movement of ocular prosthesis[6].
Donor sclera is the most widely used wrapping material[7-8]. However, because of the potential spreading risk of Creutzfeldt-Jakob disease (CJD)[10], human immunodeficiency virus (HIV)[11-12], hepatitis B virus and hepatitis C virus[11], possibly occuring of late thinning of the sclera[9], and occasional unavailability of donor sclera has raise the need of other alternative materials for wrapping. These materials includes autogenous materials like fascia lata, animal-derived tissue like bovine pericardium, and synthetic materials like polyglactin 910 mesh and Mersilene mesh[6-7,11].
Bovine pericardium as an animal-derived tissue, was initially believed to be a viable alternative to donor sclera as the wrapping material[7-8]. However, Char[22]found an even higher rate of implant exposure with bovine pericardium than donor sclera, especially at the early-stage after surgery. Another histopathologic study, which was performed in an animal model, showed that HA implants with bovine pericardium cap would had later and less extensive fibrovascularization than implants with sclera cap. They also found that bovine pericardium was associated with significantly greater inflammation in the outer 20% of the material compared with sclera and showed more disruption of the lamellar architecture of its collagen bundles[7].
Fascia lata as autogenous materials, has been tried to be the alternative wrapping material. However, HA implant wrapped with fascia lata appeared to undergo even less rapid fibrovascularization than spheres wrapped with bovine pericardium in animal model[7]. This late fibrovascularization would increase the risk of HA exposure.
Auricular cartilage as another autogenous material shares many characteristics with sclera. It has been used for various oculoplastic procedures and achieved satisfied outcomes. It is easy to obtained and has minimal morbidity[23]. Thus, it could be used at any emergency cases. In order to hide the incision, as well as remaining the shape of auricle, we harvested the cartilage graft from the conchal lateral wall through a post-auricular incision. Also auricular cartilage has suitable flexibility and rigidity which could resist the rub of ocular prosthesis[24]. When compared to donor sclera, it is nonabsorbable and has better biological activity, lower incidence of late shrinking or thinning, which could significantly increase the ability of anti-inflammation and reduce the occurrence of implant exposure. In this study, the auricular cartilage graft was found to have good shape and position one year after surgery according to the MRI imaging (Figure 3). None of our patients with auricular cartilage caps had prolonged postoperative inflammation. No HA exposure was occurred in cases with auricular cartilage cap while one case with donor sclera cap and one case without any wrapping developed implant exposure after surgery. Moreover, ear cartilage has a spherical surface and fits well to a bulbar surface[23].
It is well known that a fully organized implant could maintain a healthy conjunctiva indefinitely. Thus, some researchers concerned that the barrier made by wrapping material would inhibit vascularization[9,25-28]. In order to minimize this effect, we did some modifications during the surgical procedure. The wrapping material (autogenous ear cartilage or donor sclera) was sutured just to the 4 rectus after placing the HA implant into the muscle cone thus to wrap only the frontal part of the implant, leaving the majority posterior part of the implant uncovered. This modification could avoid the implant exposure at the front part without inhibiting valcular ingrowth at the back part.
Mild complications, including conjunctival inclusion cysts, severe conjunctive chemosis and conjunctive granuloma, were found in this study as well. Lower incidence rate was found in cases with wrapping cap. This seems to indicate that the wrapping material wouldn’t increase the incidence of prolonged postoperative inflammation. Two conjunctival inclusion cysts were found in this study. Severe ocular injury was the cause of enucleation of both cases. The disorder of ocular tissue before surgery would lead to incomplete tissue isolation during the surgical procedure. This may be the reason of the happening of conjunctival inclusion cysts.
In conclusion, auricular cartilage can be a good choice of alternative wrapping material of orbit implant with satisfied outcome. Based on the absence of possible disease transmission, easy obtained, good biological activity and resistant of rubbing, nonabsorbable and lower incidence of late shrinking or thinning, auricular cartilage is now our favorite wrapping material for orbital implants. However, there are still weaknesses in this study, including small sample and short follow-up time. A large-sampled, longer follow-up, controlled perspective study is needed to further confirm the safety and efficacy of auricular cartilage as the implant wrapping material.
ACKNOWLEDGEMENTS
Conflicts of Interest: Ma YJ,None;Zhu XY,None;Chen B,None;Lin YY,None;Liu J,None;Chen X,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
