Comparison of healing patterns of different side-cut angulations after FS-LASlK
Wei Wei, Xi-Yu Sun, Di Shen, Xiao-Rui Wang, Yu-Qiang Ji, Chang-Ning Zhang
Xi’an No.1 Hospital; Shaanxi Institute of Ophthalmology; Shaanxi Key Laboratory of Ophthalmology; Clinical Research Center for Ophthalmology Diseases of Shaanxi Province, First Affiliated Hospital of Northwestern University, Xi’an 710002, Shaanxi Province, China
Abstract
INTRODUCTION
With improved technology, advanced femtosecond laser systems are superior even to small incision lenticule extraction (SMILE) devices for flap creation[1]. Femtosecond lasers give surgeons more options for customizing flap thickness, flap diameter, and the side-cut angle to improve clinical results[2-3].
However, different side-cut angulations may change laserassisted in situ keratomileusis (LASIK) corneal flap adhesion after surgery. Previous laboratory studies have found that flaps with inverted side-cut angulations are more difficult to dislocate, thereby decreasing the possibility of post-surgical flap displacement[4]. Another study have even suggested that flap adhesion could be strengthened if more inflammation occurred during wound healing, which may be observed with slit-lamp microscopy in the form of obvious scarring around the flap margin[5]. A recent clinical study has found that different side-cut angles have some effect on corneal biomechanical properties, and their Ocular Response Analyzer (ORA) results have shown that corneal deformation is more stable with an inverted side-cut angle[6]. Another study has indicated that inverted side-cut angles are associated with superior corneal sensation recovery compared to flaps made with conventional side-cuts[7].
Using a femtosecond laser to create side-cuts designed to induce activated cornea wound healing might allow for earlier suture removal[8]. However, as far as the present authors know, no available reports compare the clinical wound healing of different side-cut angle profiles. Therefore, to determine methods for better patient outcomes, this prospective study compares the flap margin wound-healing scars of FS-LASIK surgery flaps made with 90° and 120° angulations.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Xi’an No.1 Hospital Institutional Review Board Ethics Committee and the Recommendations of International Committee of Medical Journal Editors (ICMJE), and our trial registration number is ChiCTR1900023568. Detailed informed consent was obtained from each patient, and all patients were treated in accordance with the tenets of the Declaration of Helsinki.
SubjectsThis prospective study included 68 eyes of 34 myopic patients (19 males, 15 females) with or without moderate astigmatism who underwent bilateral femtosecondassisted LASIK between November 2017 and August 2018. Inclusion criteria included age equal to or greater than 18y, anisometropia of less than 1.0 D, astigmatism of less than -2.0 D, a stable refractive error over the last 2y (progressing by less than 0.5 D annually) and willingness to participate in follow-up examinations on time. The exclusion criteria included patients with active ocular inflammation, abnormal corneal topography, systemic diseases, and a minimum stroma bed cornea thickness of less than 280 μm. Rigid, gaspermeable contact lens and soft contact lens wearers were asked to discontinue wearing contact lenses before the study for at least 4 and 2wk, respectively. All procedures were performed in the Laser Vision Center of Xi’an No.1 Hospital by one experienced refractive surgeon.
FS-LASIK ProcedureThe subjects were adults with a mean±standard deviation (SD) age of 26.35±6.35y (range 18-39y), and the mean spherical equivalent (SE) of refraction was -6.23±1.65 D (range -2.50 to -9.38 D). For each patient, corneal flaps were created bilaterally using a WaveLight®FS200 laser (Alcon Labs, Ft. Worth, TX, USA). Flap creation settings were as follows: flap thickness was set to 110 μm and the diameter was 8.3 mm to 8.6 mm; the side-cut angles of flaps were 90° in one eye and 120° in the other eye for each patient; the entire flap creation time was approximately 6s; the stromal ablation was performed using a WaveLight®EX500 excimer laser system, and the optical zone was 6.0 mm; and the minimum residual corneal stromal thickness was set to 280 µm to prevent iatrogenic corneal ectasia.
Postoperative Eye CareAfter the surgery for each patient, a careful slit-lamp microscopy examination was performed to ensure corneal apposition. All patients were asked to perform the regular ocular examinations the next day after the surgery and 1wk, 1, and 3mo postoperatively. All patients were prescribed levofloxacin 0.5% eye drops, corticosteroid eye drops (fluorometholone 0.1%), pranoprofen eye drops, and sodium hyaluronate eye drops four times daily during the first week after surgery. One week after LASIK, all patients were instructed to use artificial tears four times daily and artificial gel twice a day for the following 3mo after surgery.
MeasurementsAll patients underwent comprehensive exams before surgery and again 3mo after the surgery. The preoperative exams included assessments of uncorrected distance visual acuity (UCVA), corrected distance visual acuity (CDVA), manifest and cycloplegic refraction, mesopic pupil size, slit-lamp photography, a dilated fundus examination, and intraocular pressure (IOP) with noncontact tonometry (Topcon, Japan). Grading was performed visually by slitlamp photography with a 45° light angle at 1wk, 1, and 3mo postoperatively. The grading of the scar was classified as follows[8]: Grade 0=transparent scar, Grade 1=faint healing opacity, and Grade 2=evident healing opacity. For several interesting cases, the anterior segment module of the Cirrus HD-OCT (Carl Zeiss Meditec Inc, Dublin, CA, USA) was used to image the side-cut angle of flaps. After 3 times of imaging, picture with the clearest side-cut angle was selected. In vivo confocal microscopy (IVCM) was performed with the cornea module of the Heidelberg HRT3 (Heidelberg Engineering GmbH, Heidelberg, Germany). A carbomer gel was applied on the confocal lens to evaluate wound-healing morphology around the flap edge. Each patient was asked to stare at an external target and both anterior segment optical coherence tomography (AS-OCT) and IVCM images were acquired at horizontal and vertical scan mode. Three months after surgery, higher order aberrations (HOAs, including total HOAs, spherical aberrations, coma, and trefoil), root mean square (RMS) distribution were examined by a Sirius Scheimpflug Analyzer (CSO, Costruzione Strumenti Oftalmici, Florence, Italy). All instrumental examinations were conducted by the same examiner.
Statistical AnalysisAll the statistical data were analyzed using IBM SPSS Version 22.0 (IBM Corp., Armonk, NY, USA). Differences of the preoperative and postoperative data between the two groups were determined by Student’s t test. Mann-Whitney U test was used to compare the scar grades between the two groups at each follow-up visit. In all analyses, the results are expressed as the mean±SD, and a P<0.05 was considered statistically significant.
RESULTS
The study enrolled 68 eyes of 34 patients. Preoperative data showed no statistically significant differences between eyes with 90° side cut and eyes with 120° side cut for all parameters, including UCVA, BCVA, SE, IOP, white to white, scotopic pupil size, and central corneal thickness (all P>0.05; Table 1).
Slit Lamp ObservationSlit lamp images were obtained by an independent doctor. Flap wound was classified and recorded according to the scar grading system as previously described (Figure 1). At 1wk, 1, and 3mo postoperatively, there was no statistically significant difference in the side-cut corneal healing pattern between the two groups according to scar grading systems (all P>0.05; Table 2).

Figure 1 The grading was performed as observed and registered photographically by slit lamp photography A: Grade 0: Transparent scar; B: Grade 1: Faint healing opacity; C: Grade 2: Evident healing opacity.
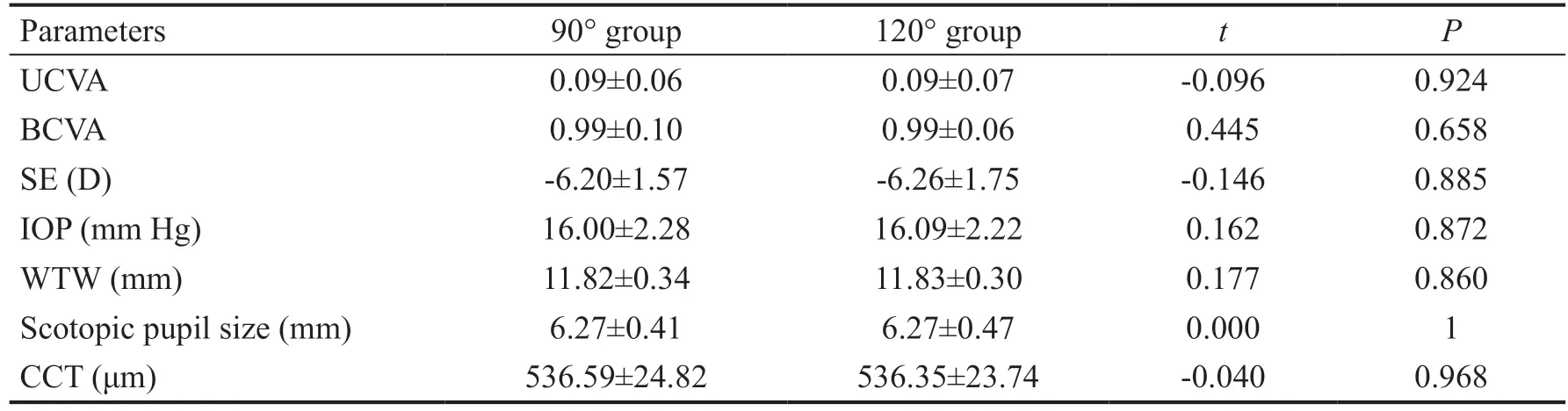
Table 1 Baseline data for 34 patients underwent FS-LASIK
Healing Pattern at the Side CutThree months postoperatively, AS-OCT was used so that side-cut angulation could be clearly observed. For interesting cases, IVCM pictures were obtained to further observe the wound healing patterns. Figure 2 showed flap edge configuration of 90°and 120° side-cut angle in one patient by AS-OCT. Figure 3 and Figure 4 showed side-cut wound margin Grade 0 and Grade 2 by IVCM respectively, which verified that different side-cut wound edges experienced similar healing patterns. In contrast, Grade 0 flap edges showed a less clearly defined periphery with epithelium invasion and faster subbasal nerve regeneration than that Grade 2.
Higher Order AberrationsPreoperatively, there was no significant differences between two groups in HOA, including total HOAs, spherical, trefoil, and coma under different pupil diameters (all P>0.05; Table 3).
Three months after the surgery, under 3 mm pupil diameter, total HOAs, spherical, trefoil and coma in 90° group was 0.14±0.14 μm, 0.02±0.02 μm, 0.09±0.09 μm and 0.04±0.04 μm, and in 120° group was 0.11±0.04 μm, 0.09±0.01 μm, 0.05±0.04 μm and 0.04±0.02 μm, respectively; under 5 mm pupil diameter, total HOAs, spherical, trefoil and coma in 90° group was 0.55±0.30 μm, 0.28±0.11 μm, 0.24±0.22 μm and 0.28±0.18 μm, and in 120° group was 0.50±0.19 μm, 0.28±0.09 μm, 0.14±0.13 μm and 0.31±0.18 μm, respectively; under 7 mm pupil diameter, total HOAs, spherical, trefoil and coma in 90° group was 2.24±0.69 μm, 1.76±0.46 μm, 0.56±0.40 μm and 0.87±0.60 μm, and in 120° group was 2.23±0.84 μm, 1.75±0.54 μm, 0.39±0.35 μm and 0.98±0.61 μm, respectively. There was a significant difference in trefoil aberrations at the 3 mm and 5 mm pupildiameter between the two groups (P<0.05; Table 4). There were no statistically significant differences in total HOAs, spherical aberrations or coma aberrations in any pupil size condition (P>0.05; Table 4).
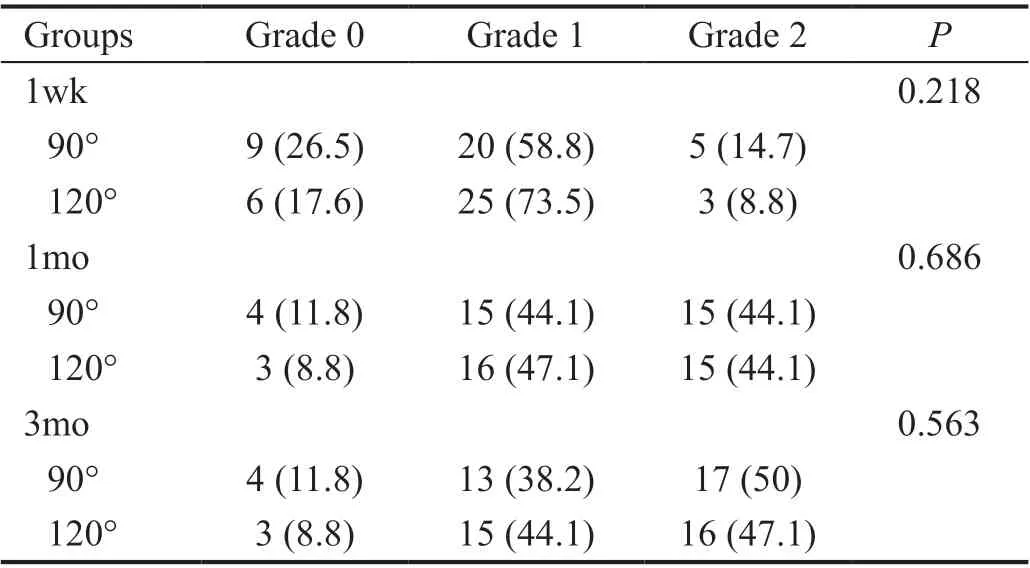
Table 2 Comparison of grade between 90° and 120° side-cut angles eyes (%)
DISCUSSION
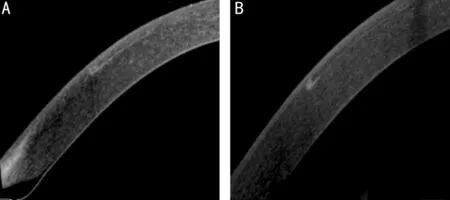
Figure 2 Bilateral eye comparison of one patient Both corneas were classified as Grade 0. A: The flap was created using a 90° sidecut angle; B: The flap was created using a 120° side-cut angle.
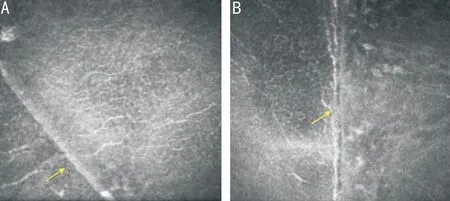
Figure 3 Bilateral eye comparison of the same patient Both corneal flaps were classified as Grade 0. A: 90° side-cut angle wound margin; B: 120° side-cut angle wound margin showed excellent apposition, and subbasal nerve regeneration was observed.

Figure 4 Bilateral eye comparison of another patient Both corneal flaps were classified as Grade 2. Evident hypercellular fibrotic stromal scaring around the wound and an epithelial plug in the wound gap was observed; no nerve regeneration was found. Because the morphology of scar under slit-lamp of bilateral eyes was similar, only the right eye was examined by IVCM to show wound-healing patterns.
McCulley and Petroll[9]have evaluated FS-LASIK corneal wound healing using IVCM, and their results reveal that femtosecond laser could induce evident keratocyte activation, which might be observed as corneal haze under slit-lamp microscopy and could potentially be advantageous in sidecut keratoplasty surgery. Alio et al[8]have discovered that healing at the side-cut is more evident in femtosecond-assisted deep anterior lamellar keratoplasty (DALK) according to the scar grading system. They suggest that scarring at the wound margin could be considered an indicator for earlier suture removal. Prior studies have also demonstrated that different side-cut angles using femtosecond laser may affect flap adhesion and possible epithelial ingrowth because of the different healing processes they would induce around the flap margin. In this study, to verify optimized side-cut angle around the flap margin, we compared 90° and 120° side-cut angles using a slit-lamp microscopy scar grading system and IVCM. To compare the healing outcomes, we analyzed HOA using a Sirius aberration system.
Stromal fibrosis is present at all LASIK flap edges, varying across patients. This fibrosis is helpful for preventing latedislocations of the flap due to minor trauma, which can result in epithelial ingrowth[10-11]. In earlier studies, researchers considered that the degree of flap margin scar might contribute to flap adhesion. Theoretically, a higher energy is more likely to create a stronger scar. Netto et al[12]have found that a highenergy femtosecond laser tends to promote more inflammation, which is visible in slit-lamp photographs as greater scars at flap edges, and they assume that the greater healing of the flap is advantageous for decreasing the incidence of flap displacement. Other studies have demonstrated that the growth factors and cytokines that enhance wound healing processes may increase flap adhesion strength by forming more inflammation. Paradoxically, in a laboratory study, Riau et al[13]have compared different energy levels of femtosecond lasers, evaluating flap strength and tissue responses, but they did not find a significant difference between the low and high-level energy groups. Knorz et al[5]have compared flap adhesion using different side-cut angles and energy levels, and they have also found no significant differences between the normal (0.8 μJ) and high level (1.6 μJ) energy groups. However, they have determined that flap adhesion is significantly stronger when an inverted 140° side-cut angle is used, compared to a 70° standard side-cut angle, and they suggest that side-cut geometry is a far more significant factor in flap cohesive tensile strength than scar inflammation. On the contrary, our study found that a 120° side-cut wound gap was comparable to 90° side-cut flaps, and the epithelial plug was still able to be found beneath the edge three months after surgery. Zhao et al[14]have expressed that the application of bandage contact lenses could reduce wound healing response at the flap margins due to its compression function. Hence, we hypothesize that scarring around the flap margins can have three causes: 1) damage to the epithelium and its membrane, triggering inflammation factors; 2) poor flap edge adhesion creating a wide gap; and 3) tears, containing inflammation factors, flowing into the gap causing more healing responses.
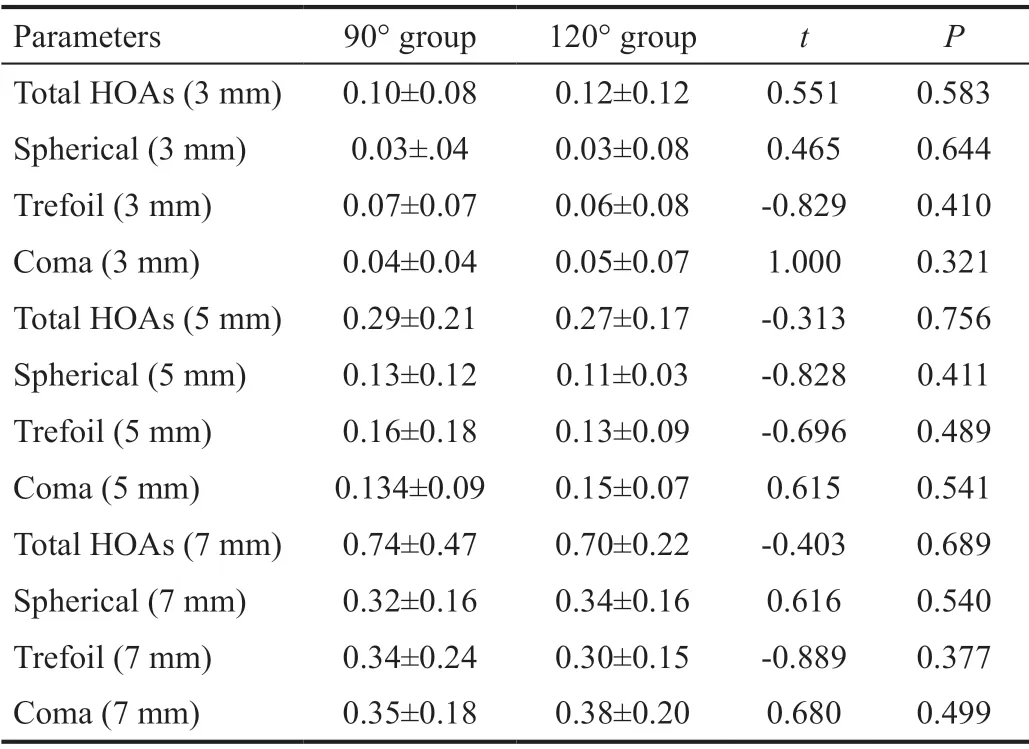
Table 3 HOA before FS-LASIK RMS, μm

Table 4 HOA postoperatively 3mo after FS-LASIK RMS, μm
Compared to a flap created with a mechanical microkeratome, which has an acute side-cut angle, the configuration of the side-cut angle with a femtosecond laser may be customized more easily. The side-cut angle may affect interface epithelial ingrowth or potential corneal flap displacement. A porcine study has found that epithelial ingrowth occurs more frequently with a mechanical microkeratome, which creates an acute side-cut angle and a longer epithelium-traveling distance for the epithelium, than with a femtosecond laser, which produces a more vertical side-cut to the flap interface[15]. Another biomechanical study has found that wound gape is lessened and fewer keratocytes are visible in the in vitro cornea when a 135° side-cut is made[4]. In a recent laboratory study, Jhanji et al[16]have determined that 70° side-cut flaps undergo more epithelial ingrowth and significantly increase apoptotic cells compared to 115° side-cut flaps. In our clinical study, we compared the flap margin healing grade, but no significant difference was found between the conventional 90° and inverted 120° side-cut angle groups. This may be because in vivo corneas undergo different healing processes than those of the rabbit or human eye bank corneas after FS-LASIK; however, few studies have addressed this question, so these differences are still unknown at present. In the clinical evaluation, the biomechanical properties of the cornea, as measured with an ORA, have shown no significant differences between 70° and 115° side-cuts in FS-LASIK[17].
Kung et al[7]have discovered that LASIK flaps with inverted side-cuts are associated with superior corneal sensation recovery compared to flaps with conventional side-cuts, indicating that an inverted side-cut angle might offer better wound apposition or faster nerve recovery. However, in our study, there was no significant difference for scar grading between the side-cut angles, which indicated that changing side-cut angulations made little difference in wound-healing patterns. We used IVCM to observe the corneal wound edge, determining that corneas with Grade 0 wound-healing patterns had better apposition and faster nerve regeneration, while Grade 2 wound-healing patterns had an evident hypercellular fibrotic stromal scar around the wound, and if there was an epithelial plug in the wound gap, no nerve regeneration would be found. According to an eye bank cornea study, wound margin scars with epithelial cell ingrowth are approximately one-third as strong as those without epithelial ingrowth[18]. Following injury, surviving corneal stromal keratocytes (CSKs) are activated to stromal fibroblasts (SFs). Proteins uniquely present in serum-free conditioned media (SFCM) report neuroregulatory activities and are predicted to regulate neurogenesis, focal adhesion, and wound healing[19]. We insist, therefore, that further studies should be carried out to determine the relationship between regeneration and flap adhesion.
Another significant finding of this study was the high order outcomes three months after FS-LASIK procedures. There was a significant difference showing less trefoil aberration at the 3 mm and 5 mm pupil diameter and a tendency toward less trefoil aberration in the 120° side-cut group. Issa and Al Hassany[20]have created different flap side-cut angles of 110°, 90°, and 45° using a VisuMax femtosecond laser system, and have found no clinically significant differences in refractive, visual acuity, or wavefront outcomes. This may be because they selected the ablation optical zone diameter according to the mesopic pupil diameter and changed the corneal flap thickness from 80 μm to 120 μm, while in our study, we set all optical diameter to 6.0 mm and flap thickness to 110 μm. Most previous studies have demonstrated that HOA increase after LASIK. In an early study, researchers found an RMS distribution for significantly higher trefoil aberrations in mechanical keratome LASIK than in femtosecond laser LASIK[21]. However, another study has found that femtosecond laser-assisted LASIK results in more trefoil aberrations postoperatively than does mechanical LASIK[22]. At present, the exact mechanism of trefoil aberrations is still not entirely clear. Furthermore, based on most studies, HOA are mainly affected by ablation rather than flap creation. Therefore, we hypothesized that tensile strength will be stronger in inverted 120° side-cut flaps, which can enhance flap adhesion and induce less trefoil aberration after surgery, although it cannot be identified by slit-lamp microscopy, IVCM, or even an ORA.This study has presented some limitations. First, we observed and classified corneal flaps up to three months postoperatively and because of some patients’ unwilling to undergo IVCM examination, we failed to observe flap wound morphology classified as Grade 1, therefore, the long-term healing appearance could not be thoroughly evaluated. Second, the sample size might be sufficient for revealing potential differences in wound-healing patterns with different side-cut angles. Third, we used Sirius to compare corneal aberrations. Though trefoil aberration differences were found, we could not elucidate the exact mechanism behind these differences. In future studies, we should introduce additional aberration devices, such as Tracy, to confirm the results.
In conclusion, although this study found that FS-LASIK with 90° or 120° side-cut angulations had no differences in wound-healing patterns, the flap edge scar classified as Grade 0 had excellent apposition and fast nerve regeneration, while Grade 2 presented obstructed nerve regeneration. Less trefoil aberrations in 120° flaps indicated that corneal stability might be enhanced with a 120° side-cut angle corneal flap.
ACKNOWLEDGEMENTS
Authors’ contributions:Wei W was responsible for study design; Sun XY and Wang XR were responsible for literature search and screening as well as data analyses and interpretation; Shen D was responsible for literature screening and data analyses; Ji YQ was responsible for checking data and analyses; Zhang CN was responsible for revising the manuscript. All authors read and approved the final manuscript.
Foundations:Supported by the Science and Technology Program of Xi’an, China [No.201805097YX5SF31(2)]; the Foundation of Shaanxi Province Key Research and Development Project (No.2018SF-216).
Conflicts of Interest: Wei W,None;Sun XY,None;Shen D,None;Wang XR,None;Ji YQ,None;Zhang CN,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
