Efficacy of wet-lab training versus surgical-simulator training on performance of ophthalmology residents during chopping in cataract surgery
Ya-Guang Hu, Qiu-Ping Liu, Ning Gao, Chang-Rui Wu, Jian Zhang, Li Qin, Jing-Ming Li
1Department of Ophthalmology, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710061, Shaanxi Province, China
2Affiliated Eye Hospital of Nanchang University, Nanchang 330006, Jiangxi Provnice, China
3Department of Ophthalmology, Shaanxi People’s Hospital, Xi’an 710068, Shaanxi Province, China
Abstract
INTRODUCTION
Almost half of all cases of blindness worldwide are attributed to cataract[1]. As life expectancy has extended, more people in old age select to undertake the cataract surgery in order to continue their visual aptitude[2-5]. Hard nuclear cataracts are always existed in older people, especially in rural population in China[6]. When chopping the hard nuclear cataract in a cataract surgery, it is a crucial step to divide the hard nuclear cataract into two hemispheres. The ophthalmology residents may need more ultrasound energy and higher vacuum, which may cause many complications such as corneal edema, endothelial injury, and capsular rupture. So, it’s a challenge for the ophthalmology residents to completely chop the hard nuclear cataract into multiple small fragments.
Traditionally, ophthalmology residents use pig eyes in a wet-lab to exercise the chopping technique. Although the structure and the size of pig eyes are similar to human eyes, the formation and the hard level of the nuclear cataract make chopping much different from that in a reality human eye. And the obstructive factors with obtain high quality pig eyes and setup a wet-lab limit the residents to improve their surgical skills. For some time, the Eyesi surgical simulators have been presented for cataract surgery[7-8]. And there have been several studies report that the virtual-reality simulation training could improve the performance of ophthalmology residents in the operating room[9-10].
It has come to our knowledge that there was no prospective randomized study compare the effectiveness of wet-lab training (WLT) and surgical-simulator training (SST) in chopping. As chopping is a most challenging part in cataract surgery, we set out a study to analyze whether WLT or SST is better for ophthalmology residents to master the chopping technique.
SUBJECTS AND METHODS
Ethical ApprovalAll procedures adhered to the Tenets of Declaration of Helsinki. Written informed consent was obtained from the participants.
ParticipantsSixty second-year ophthalmology residents and three cataract surgeons from the three teaching hospitals participated in the study. All of the surgeons had performed over 1000 cataract operations and they were asked to separately score the performance of the residents. All of the residents were familiar with the procedure of cataract surgery and had finished the previous curriculum of continuous curvilinear capsulorhexis. The sixty residents were randomly separated into two group, WLT group and SST group.
Surgical SimulatorIn order to assess the chopping skills of the ophthalmology residents, the surgical simulator, Eyesi, was used in this study (VRmagic GmbH, Germany; software version 2.9.2). A model eye was involved in the cataract head of the surgical simulator, and handheld probes simulated vitural instruments when inserted into a virtual eye. Through two oculars, a virtual binocular stereoscopic image was shown. The phaco divide and conquer module (medium level) was used directly: the residents had to chop the nuclear cataract into more than four quadrants. The surgeons could monitor the process on a viewing panel. At the end of each surgery, the simulator would score the surgery on multiply criteria. The score was based on multiple criteria and recorded by the software program.
ProcedureAll of the ophthalmology residents were received one-hour teaching on the purpose and the tips of chopping a lens nuclear cataract. Then a brief orientation to the surgical simulator and wet-lab was given. In advance, each resident in WLT group should finish 10 capsulorhexis using pig eyes and the surgeons confirmed the results. The surgeons could assist the residents to finish the capsulorhexis. Then, each resident perform 10 trials of chopping lens nuclear cataract and the three surgeons separately scored each surgery on multiple criteria, including the number of need attending help, time duration, economy of movement, posterior capsule state and incisional stress. The surgery that had the highest overall score was selected as the final score of the resident. Finally, this group was asked to perform one surgery on the simulator and scored by the simulator automatically. The residents in surgical simulator group were asked to perform 10 trials of chopping directly and the simulator recorded the trial, which had the highest overall score. Then, they were asked to perform one surgery with the pig eye and scored by the surgeons separately.
Statistical AnalysisAll the collected data were expressed as mean±SEM. We used SPSS 19.0 software (SPSS Inc., Chicago, IL, USA) for statistical analyses. When two groups were compared, Student’s t-test was used for measurement data, which matched Gaussian distribution. If not match, Mann-Whitney U test was used. Besides, Pearson’s Chi-square test was used for enumeration data. Spearman’s correlation test was used to calculate the correlations between the variables. P value <0.05 was considered as statistically significant difference.
RESULTS
Demographic Characteristics of the Ophthalmology ResidentsThe backgrounds and demographics were summarized in Table 1. All of the sixty ophthalmology residents with 2-year training experience were randomly separated into two group, WLT group (n=30) and SST group (n=30). The demographic characteristics had no significant differences between the two groups. The mean age of the residents in surgical simulator training group and WLT group, respectively, were 26.47±0.29 and 26.60±0.26. The gender distributions (male/female) for SST group and WLT group, respectively, were 15/15 and 19/11. In addition, we investigated the resident’s background. There are 13 in SST group and 14 in WLT group consumed coffee or tea. In SST group, 13 played video games and 14 played musical instrument. And in WLT group, 15 played video games and 13 played musical instrument. There was no significant difference between two groups (P>0.05).
Surgical Simulator Performance ScoresAs shown in Table 2, recorded by the simulator, the residents in SST group got significantly higher overall score (83.90±1.31) than the WLT group (78.73±1.92; P=0.03). As listed, the simulator scored the performance of residents for several aspects, such as injured cornea area value, instrument slipped out of sphere (No. events), time duration, injured lens area value, ultrasonic energy value and posterior capsule torn. The residents in the SST group got less corner area injured, and they spend less time than the WLT group (P<0.05). Moreover, the residents in WLT group used more ultrasonic energy value than the SST group (P=0.03). However, there were no significant differences between the two groups on these aspects, such as frequenciesof instrument slipped out of sphere (P=0.35), injured lens area value (P=0.61), and frequencies of posterior capsule torn (P=0.57). Statistical results of the residents’ performance in surgical simulator training were shown in Figure 1.

Table 1 The demographic characteristics of the ophthalmology residents mean±SEM
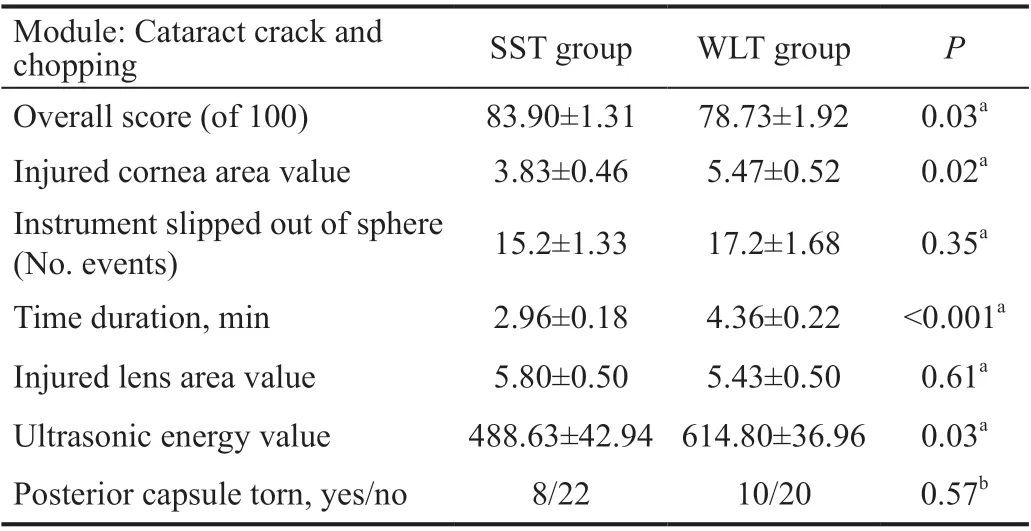
Table 2 The residents’ performance in SST mean±SEM
Wet-lab Performance ScoresBoth of the two groups finished the surgery in the wet-lab using pig eyes, and three surgeons separately scored the performance. The results were shown in Table 3. The residents in the WLT group got overall score 81.37±1.79, and the SST group got 79.87±2.01. There was no significant difference between two groups (P=0.68). The surgeons scored the residents’ performance with several criteria, including the number of need attending help, time duration, economy of movement, posterior capsule state and incisional stress. The residents in the WLT group performed better on the frequencies of posterior capsule torn and incisional stress (P=0.03, P=0.008, respectively). However, they performed nearly the same on frequencies of needing attending help, time duration, and economy of movement (P>0.05). Statistical results of the residents’ performance in WLT were shown in Figure 2.
Satisfaction Questionnaire SurveyAs listed in Table 4, we set five questions to investigate the residents’ satisfaction about the training. The residents in two groups held the same opinion that the training was helpful and they strongly recommended this training. Moreover, all of them enjoyed the training, and enjoyed being randomized in their own group (P>0.05). However, with respect to the realistic character, the residents thought that the WLT was better than the surgical simulator training (P<0.001). Statistical results of the satisfaction questionnaire survey were shown in Figure 3.

Figure 1 Statistical figure of the residents’ performance in surgical simulator training aP<0.05, cP<0.001.

Figure 2 Statistical figure of the residents’ performance in WLT aP<0.05, bP<0.01.
DISCUSSION
Cataract surgery is one of the most common surgical procedures in the world. Traditionally, training has been done using a master-apprentice approach of supervised surgery on patients[11]. And this training way is still dominant in many countries[12]. Thus, much more complications were happened in the beginning of the apprentice’s surgery[13]. In order to avoidthis, virtual reality-based surgical simulators and animal eyes in wet-lab are increasingly being used in recent year.
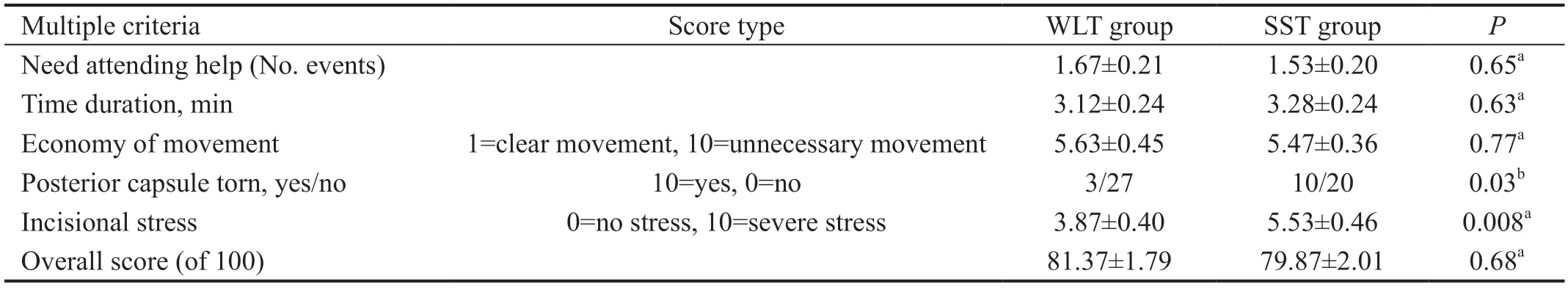
Table 3 The residents’ performance in WLT mean±SEM

Table 4 Results of the satisfaction questionnaire survey mean±SEM

Figure 3 Statistical figure of the satisfaction questionnaire survey cP<0.001.
Previously, the surgical simulator Eyesi, designed to simulate intraocular surgery in a virtual environment has been validated as a perfect scoring tool for cataract surgical skill training[14-15]. And WLT has also been shown to be an effective method for mastering surgical skills and is an important training tool that helps residents in performing cataract surgery[16]. Successful cataract surgery for hard nuclear cataract might depend on how well the surgeon divided the lens nuclear cataract into multiple small fragments. And chopping is the most crucial and challenging step. Our present study compared the performances of the residents in chopping by using the surgical simulator and wet-lab.
By using the surgical simulator Eyesi, the SST group got better performance than the WLT group because they got higher overall score. In detail, the SST group got less injured cornea area value, and used less ultrasonic energy value. Meanwhile, they used less time to finish the procedure of chopping lens nuclear cataract. However, in the matter of frequencies of instrument slipped out of sphere, injured lens area value and poster capsule torn, the residents in two groups did nearly the same.
By using the pig eyes for training, although the WLT group got higher overall score, there was no significant difference between the two groups. While, the WLT group performed less frequencies of posterior capsule torn and less incisional stress than the SST group. In the matter of frequencies of needing attending help, time duration and economy of instrument movement, the residents in two groups did nearly the same.
Obviously, each group got a higher score when the residents were evaluated by their familiar way, which they had practiced for ten times. The WLT group performed better when using the pig eyes as evaluation, while the SST group did well in using the surgical simulator Eyesi. Thus, we wondered that whether the proficiency accumulated in training affected their performance. Moreover, the reason of less frequencies of posterior capsule torn and less incisional stress in WLT group might be the pig eyes were veritable things. If the incisional stress increased, the cornea would be deformed, which may blurred the clarity of visual field under surgical microscopy. The residents would notice this phenomenon. However, the residents in the SST group might ignore it.
At the same time, it is worth noting that criteria used by three surgeons merits critical evaluation, as some indicators are subjective and not well quantified, such as economy of movement, need attending help and incisional stress in wetlab performance scores. Moreover, the study needs to perform a baseline trial to make sure there was no statistical difference in residents’ operational ability. And precautions should be taken before making any certain conclusions, as it can be questionable whether transfer of skills between medical students and surgeons can be reliable. Increasing the number of surgeons for evaluation and setting up an inspection standard may be helpful to ensure more consistent results.
Generally, two training ways both improve the residents’ chopping ability and each has its own advantages. Moreover, all the residents enjoyed the training. The SST can reduce the use of ultrasonic energy, time duration and injured cornea area value. After the WLT, the residents significantly avoid posterior capsule torn. The training cannot only be used in chopping technique but also in other surgery skills. Commonly barriers to traditional teaching of ophthalmologic surgery are limitation of the number of instructors and patients. SST and WLT represent an ideal solution for practicing technical skills out of the operating room. Multiple studies have reported that SST and WLT could improve the surgical performance in ophthalmology, shortens the learning curve of the residents and surgical time and decreases the risk of complications[17-20].
For future practice, the combination of the Eyesi surgical stimulator and the wet-lab could be considered to be a part of the training curriculum for new residents, making them more suited to finish surgery in real life. And further investigation is needed to gain more insight into how we can best optimize the use of the simulator to improve upon ophthalmic surgery.
ACKNOWLEDGEMENTS
Foundations:Supported by Natural Science Foundation Grant from Jiangxi Science and Technology Department (No.20192BAB205049); Young Talent Scholar Grant (No.2016KJXX-12) from Shaanxi Science and Technology Department, Teaching Reform Grant (No.JC2020-0309; No.JG20190330).
Conflicts of Interest:Hu YG,None;Liu QP,None;Gao N,None;Wu CR,None;Zhang J,None;Qin L,None;Li JM,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Protective effects of riboflavin-UVA-mediated posterior sclera collagen cross-linking in a guinea pig model of form-deprived myopia
- Effect of zymosan on the expression and function of the gap-junction protein connexin 43 in human corneal fibroblasts
- LRG1 promotes epithelial-mesenchymal transition of retinal pigment epithelium cells by activating NOX4
- Comparative evaluation of rotational stability of toric lOLs with four-eyelet vs two-eyelet capsular tension rings in eyes with high myopia
- An Ex-Press implant versus trabeculectomy in a fibrotic bleb with late failure after previous trabeculectomy
- Dynamic versus static ultra-widefield fluorescein angiography in eyes with diabetic retinopathy: a pilot prospective cross-sectional study
