Exudative hemorrhagic retinopathy related to all-trans retinoic acid differentiation syndrome in a patient with acute promyelocytic leukemia
Emily K. Tam, Steven Ness, Crandall E. Peeler,2
1Department of Ophthalmology, Boston Medical Center, Boston, Massachusetts 02118, USA
2Department of Neurology, Boston Medical Center, Boston, Massachusetts 02118, USA
Dear Editor,
We report a case of significant exudative hemorrhagic retinopathy attributed to differentiation syndrome (DS). DS is a systemic inflammatory condition seen in patients with acute promyelocytic leukemia (APML) undergoing treatment with all-trans retinoic acid (ATRA). DS can lead to endothelial injury and capillary leakage throughout the body. Treatment with corticosteroids during chemotherapy has been shown to reduce the risk of developing DS[1-2]. There are limited reports of the ocular manifestations of DS in the literature, including pale yellow choroidal lesions, scattered retinal hemorrhages, and serous retinal detachments[3-5].
A 25-year-old male presented to the Emergency Department with two weeks of fatigue and intermittent bleeding from his nose and gums. A complete blood count demonstrated profound thrombocytopenia (platelet count of 5 k/μL, reference range 150-400 k/μL) and leukocytosis (white cell count of 22.4 k/μL,reference range 4.0-11.0 k/μL) with blasts. Hemoglobin was 10.5 g/dL (reference range 13.5-17.5 g/dL). A peripheral blood smear and bone marrow biopsy were consistent with APML [t(15;17)(q24;q21)/PML-RARA translocation]. He was admitted for standard treatment with ATRA, arsenic trioxide, and intravenous corticosteroids. An initial ophthalmology consult for bilateral blurring of vision demonstrated visual acuity of 20/30 in both eyes with scattered subretinal, intraretinal, and preretinal hemorrhages (Figure 1) consistent with typical leukemic retinopathy[6].
Ten days later, shortly after cessation of intravenous steroids, he developed hypoxia, tachycardia, fever, and worsening vision in both eyes. Best corrected visual acuity at that point was 20/60 on the right and 20/200 on the left. Repeat funduscopic examination demonstrated significant worsening of his retinal hemorrhages with new-onset optic nerve swelling (Figure 2) and bilateral macular edema (Figure 3).
Repeat labs demonstrated a white blood cell count of 0.7 k/μL, a platelet count of 28 k/μL, and hemoglobin of 7.8 g/dL. Serum viscosity was normal (viscosity level of 1.3 Centipoise, reference range 1.4-1.8 Centipoise). Fluorescein angiogram (FA; Figure 4) showed normal arteriovenous transit times with intact retinal perfusion and diffuse leakage from the optic nerves and retinal vessels. Magnetic resonance imaging (MRⅠ) of the brain and orbits with contrast showed no leukemic infiltration of the optic nerves and no signs of increased intracranial pressure.

Figure 1 Fundus photos of both eyes demonstrating retinal hemorrhages in multiple layers of the retina.
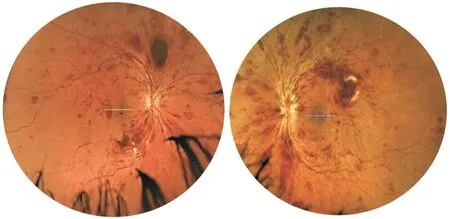
Figure 2 Fundus photos of both eyes demonstrating worsening retinal hemorrhages with new onset optic disc edema (left eye more than right eye) after cessation of prophylactic steroid therapy.

Figure 3 Optical coherence tomography images of both eyes demonstrating macular edema.

Figure 4 FA photos of transit eyes demonstrating blockage from subretinal and intraretinal hemorrhages, normal arterial venous transit (A) and diffuse leakage from retinal vessels and optic nerve (B, C).
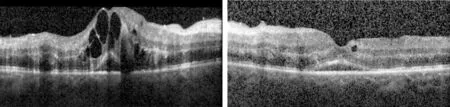
Figure 5 Optical coherence tomography images of both eyes demonstrating marked improvement of macular edema after re-initiation of steroid therapy.
Retinal hemorrhages in typical leukemic retinopathy have been associated with anemia, which can be exacerbated by coexisting thrombocytopenia and decreased platelet adhesion to the vascular endothelium[6-7]. Macular edema, however, is not a usual finding for leukemic retinopathy, but is more commonly associated with central retinal vein occlusion (CRVO) due to increased serum viscosity from leukocytosis and/or thrombocytosis[7-8]. Ⅰn our case, the acute onset of bilateral macular edema occurred in the setting of normal serum viscosity and an improving platelet count and leukocytosis. Ⅰn addition, the normal transit time on fluorescein angiography argues against CRVO.
We therefore attributed the acutely worsening retinopathy with macular and optic nerve edema, coinciding with worsening systemic symptoms, to DS, a common complication of retinoic acid treatment characterized by dyspnea, fever, weight gain, hypotension, and pulmonary exudates[1-2]. While the exact cause of DS has not been fully elucidated, a proinflammatory cytokine surge triggered by ATRA-induced blast cell differentiation resulting in increased systemic vascular permeability has been hypothesized[1-2].
DS occurs in 2%-27% of APML patients treated with ATRA, typically at 7-12d after onset of therapy[1-2]. Current treatment recommendations in cases of DS include intravenous steroids, although there remains controversy as to whether ATRA therapy should be temporarily discontinued[2]. Ⅰn our patient’s case, DS resulted in diffuse retinal vascular leakage that (together with his systemic symptoms) responded to reinitiation of intravenous steroid therapy for one week. At follow-up exam, the patient’s vision improved to 20/40 in both eyes with decreased macular edema (Figure 5).
There are currently few reports of the ocular manifestations of DS. A case series of two patients by Newmanet al[3]described multifocal, pale yellow choroidal lesions, scattered retinal hemorrhages, and diffuse late leakage on FA associated with subretinal fluid that improved with steroid therapy. Levasseuret al[4]reported a case of DS-induced multifocal serous retinal detachment that completely resolved after initiation of steroid therapy. Another study by Huaet al[5]found choroidal effusions with serous retinal detachments involving the macula. Our case is the first to report significant exudative hemorrhagic retinopathy from DS. Similar to the aforementioned studies, our patient’s ocular manifestations improved with re-initiation of steroid therapy. Although less common than the classic systemic symptoms, vision loss due to increased retinal vascular permeability should be recognized as a potential complication of DS and treated promptly with systemic steroid therapy.
ACKNOWLEDGEMENTS
Conflicts of Interest:Tam EK,None;Ness S,None;Peeler CE,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
