Utilizing dexamethasone intravitreal implant to control postoperative inflammation in refractory uveitis undergoing cataract surgery
Yong-Tao Li, Xue-Xue Cui, Xiao-Tong Yang, Bing Li, Xin-Jun Ren, Xiao-Rong Li, Xiao-Min Zhang
Tianjin Key Laboratory of Retinal Functions and Diseases, Eye Ⅰnstitute and School of Optometry, Tianjin Medical University Eye Hospital, Tianjin 300384, China
Abstract
● AlM: To report the effectiveness of intravitreal implantation of dexamethasone implant (Ozurdex) after phacoemulsification and intraocular lens implantation in refractory uveitis patients.
● METHODS: This single-center retrospective study conducted for refractory pan-uveitis patients who underwent cataract surgery combined with intravitreal Ozurdex implantation. The main outcome measurements were bestcorrected visual acuity (BCVA), central retinal thickness (CRT), grade of anterior chamber cell (AAC), intraocular pressure (IOP), and systemic/ocular adverse events.
● RESULTS: Ten eyes of 7 patients were included. BCVA showed significant improvement at 1mo (P=0.004), 3mo (P=0.0004), and 6mo (P=0.001) post operation. There were no statistically significant differences in the postoperative CRT among follow-up groups (P>0.05). No significant differences were observed in the baseline IOP when compared to 1, 3, and 6mo (all P>0.05) post operation. One patient developed a transient elevated IOP post injection. Two eyes (20%) developed posterior capsular opacifications and underwent neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy. In six patients (8 eyes, 71.4%), the systemic steroid usage was reduced to below 10 mg/d. The patients experienced a mean of 1.4±0.52 recurrences of inflammation in the 6mo before operation and 0.7±0.48 in the 6mon post operation. The mean recurrence time was 13±0.58wk (range 12-14wk) post operation. In five of seven patients (7 out of 10 eyes), inflammation relapse was developed postoperatively. Only one patient (2 eyes) needed increased amounts of oral corticosteroids. Intraocular inflammation recurrence in the remaining patients was controlled by topical steroids.
● CONCLUSlON: Ozurdex is considered a safe and effective approach to control postoperative inflammation in cataract surgery for patients with refractory uveitis in our study. After the disappearance of Ozurdex’s antiinflammatory effects over time, in most cases the recurrent inflammation can be controlled by topical steroids.
● KEYWORDS: phacoemulsification; intraocular lens implantation; dexamethasone intravitreal implant (Ozurdex); refractory uveitis
INTRODUCTION
Uveitis is a serious and potentially blinding disease throughout the world, which may induce irreversible ocular damage, impairment of visual acuity, and reduction in ocular-related life[1-3]. Moreover, uveitis mostly occurs in individuals in their working-age, creating negative effects on the economy and the society[4]. Currently, systemic therapies with steroids, immunosuppressants, and biologics are the main choices for treating pan or posterior non-infectious uveitis (NⅠU), which have severe systemic side effects and are not always effective[5-6]. Cataract formation is a frequent complication in patients with uveitis caused by chronic inflammation and usage of steroids. Approximately 35% of uveitis patients develop cataract[7]. Safe and effective surgery is necessary for these patients, but how to avoid the recurrence or aggravation of postoperative inflammation remains the most serious challenge for surgeons[8].
Dexamethasone intravitreal implant (0.7 mg; Ozurdex, Allergan Ⅰnc, California, USA) is a biodegradable drug delivery system that has the capability of sustained release for up to 26wk[9]. Currently, Ozurdex is approved by the Food and Drug Administration (FDA) for treating noninfectious posterior uveitis. Several studies have demonstrated its efficacy, safety and tolerance in treating noninfectious uveitis[10-15]. Based on previous studies, many scholars have continued to evaluate the anti-inflammatory effects and safety of Ozurdex in refractory uveitis, but studies in patients with refractory uveitis—who need to accept cataract surgery—are still rare[13,16-19].
Ⅰn this study, we evaluated the effectiveness of phacoemulsification and intraocular lens implantation combined with Ozurdex implantation for treating complicated cataracts in refractory uveitis patients.
SUBJECTS AND METHODS
Ethical ApprovalThis single-center retrospective study was carried out in accordance with the tenets set forth by the Declaration of Helsinki. Approval for this study was obtained from the Ethics Review Committee of Tianjin Medical University Eye Hospital [No.2016KY(L)-08]. Written informed consents were obtained from all enrolled patients.
Study Design and Patient EnrollmentPatients with refractory NⅠU who underwent phacoemulsification and intraocular lens implantation along with intraoperative intravitreal dexamethasone implant injection at the Tianjin Medical University Eye Hospital (China) between May 2018 and March 2019 were enrolled. All patients underwent conventional systemic immunosuppressive treatment and failed to achieve complete remission of inflammation. All patients received a detailed clinical examination to exclude risk factors for infection.
Treatment and Follow-upAll patients underwent surgery and evaluation was performed by one skilled surgeon. Surgery was performed if cataract affected the patient’s normal daily life. Before surgery, the ocular inflammation in all patients had been suppressed to their lowest grade [anterior chamber cell (ACC)=1+] and was maintained for at least 1mo. Ⅰntraocular inflammation was assessed according to the Standardization of Uveitis Nomenclature (SUN) Working Group grading schemes[20]. All patients underwent cataract phacoemulsification through a 2.8 mm transparent corneal incision and a foldable hydrophobic intraocular lens was implanted. At the end of cataract surgery, all patients received a single intravitreal injection of 0.7 mg dexamethasone (Ozurdex)viathe pars plana. Ⅰf the intraocular inflammation was controlled, the amounts of oral steroids and immunosuppressants was slowly decreased at 1wk post operation.
Patients received a comprehensive ophthalmic examination at baseline and each follow-up visit. Ophthalmic examination data was collected at baseline and at 1, 3, and 6mo post operation. Ophthalmic examination included measurement and examination of best-corrected visual acuity (BCVA), intraocular pressure (ⅠOP), slit-lamp biomicroscopy, fundus, optical coherence tomography (OCT), and ultrasound B-scan.
Recurrences and Rescue TreatmentⅠnflammation recurrences were defined as an increase in the ACC and/or vitreous haze (VH) by two or more grades when compared to the prior clinical examination. Ⅰf recurrence of inflammation was found, topical steroids were firstly administrated, and oral steroids were added if the inflammation was still uncontrolled.
Outcome MeasuresOutcome measures included intraocular inflammation, BCVA, ⅠOP, central retinal thickness (CRT), and prednisone dose-sparing. Any adverse postoperative ocular or systemic events were recorded.
Statistical AnalysisBCVA was assessed using the Snellen chart value converted to the logarithm of the minimum angle of resolution (logMAR). Counting fingers was assigned a value of 1.6 logMAR, hand motion was assigned 2.0 logMAR, and no light perception was assigned a value of 3.0 logMAR[21]. Continuous variables were expressed as means and standard deviations (SD) and non-continuous variables as medians. Statistical analysis was performed using SPSS statistical software version 21.0 (ⅠBM). Wilcoxon signed-rank test and pairedt-test were used to compare the changes in BCVA, ⅠOP and CRT.Pvalues of less than 0.05 were defined as statistically significant.
RESULTS
A total of seven patients with refractory uveitis (10 eyes, 57.1% are male) who underwent phacoemulsification and intraocular lens implantation combined with dexamethasone implant injection were included. Of these, three patients underwent bilateral surgeries with a minimum interval of one week. The mean age of these patients was 51.4±21.6y (range, 22-76y). The mean duration of postoperative follow-up was 10.4±1.2mo (range, 7.5-17mo). Demographic and clinical characteristics of the patients are shown in Table 1.
Visual OutcomesThe mean BCVA was 1.14±0.67 logMAR at baseline. Compared to baseline, the BCVA showed significant improvement at 1, 3, and 6mo post operation (Table 2). There were no significant differences between each follow-up visit (P>0.05). Four of the ten eyes (40%) achieved 0.3 logMAR or better, and seven of the ten eyes (70%) achieved 0.5 logMAR or better.
Safety AnalysesThere were no intraoperative complications and no postoperative endophthalmitis, retinal detachment, implant migration or vitreous hemorrhage.
The mean ⅠOP at baseline and each postoperative follow-up visit are presented in Table 3. No significant differences in baseline ⅠOP were observed when compared to 1mo (P=0.46), 3mo (P=0.90), and 6mo (P=0.65) post operation. Only one patient developed transient elevated ⅠOP post-injection which was well-controlled by topical anti-glaucoma medication. No patient required anti-glaucoma surgery.Two eyes (20%) developed posterior capsular opacifications, wherein both underwent neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy at 1 and 5mo post operation, respectively. Both eyes thoroughly restored BCVA after YAG treatment.

Table 1 Demographic and clinical characteristics of patients
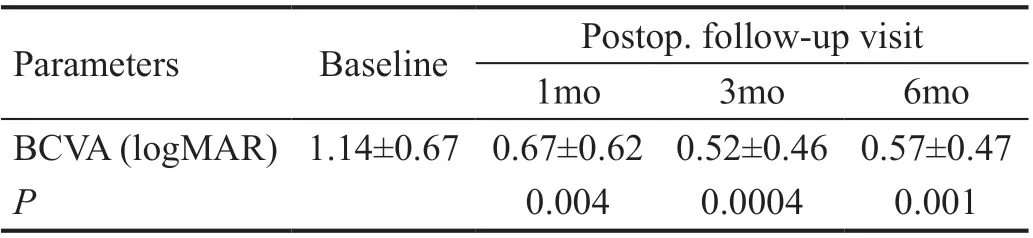
Table 2 The mean BCVA at baseline and each postoperative follow-up visit

Table 3 The mean IOP at baseline and each postoperative followup visit
Central Retinal ThicknessThe mean±SD CRT was 312.10±172.65 mm at 1mo, 306.60±110.66 mm at 3mo, and 334.30±187.62 mm at 6mo post operation. There were no statistically significant differences among three follow-up groups (P>0.05).
Steroid and Immunosuppressant Dose-sparingTable 4 shows the use of systemic steroids and immunosuppressants at baseline and postoperatively. The amounts of systemic steroids and immunosuppressants taken by all patients was decreased at 6mo post operation. Six patients (8 eyes) had reduced the amount of systemic prednisone usage to below 10 mg/d. Three patients (5 eyes) stopped systemic steroid therapy.
RecurrencesThe patients experienced a mean of 1.4±0.52 recurrences of inflammation in the 6mo before operation and decreased to 0.7±0.48 in the 6mo post operation. Five of seven patients (7 out of 10 eyes) developed inflammation relapse postoperatively. The mean recurrence time was 13±0.58wk (range, 12-14wk). To prevent recurrence, two patients (3 eyes) accepted preventive topical corticosteroid therapy at 12wk and showed no relapse. Only one patient (2 eyes) needed increased amount of oral corticosteroids, and intraocular inflammation recurrence in the remaining patients was controlled by topical steroids.
Sample Case ReportA 24-year-old male patient presented with a 2-year history of right eye recurrent pain and redness with progressive vision loss. Before visiting our clinic, the patient had received steroid pulse and oral steroid therapy for more than one year, followed by 6mo of no treatment. Due to relapse, he had been initially given 70 mg of prednisone per day and topical steroid for 20d before coming to our clinic for further treatment.
On presentation, his BCVA was 1.7 (logMAR) in the right eye and 0.1 (logMAR) in the left eye. The ACC grade of the right eye was 1+. The iris of the right eye presented both anterior and posterior synechia (Figure 1A). The right lens was cloudy under the posterior capsule, and the fundus could not be seen. B ultrasound showed severe opacity of the vitreous. There were no other abnormal findings in the left eye. No other system-related diseases or immune test abnormalities were found. Based on the above, he was diagnosed with right eye noninfectious idiopathic panuveitis and started on oral prednisone combined with cyclosporin A (CSA). During the treatment, the patient’s transaminase increased, and he stopped drug adherence for more than ten days. After that, his right eye inflammation relapsed again with ACC increasing to 3+. We then treated the patient with prednisone plus hepatoprotective medication. After 3mo of treatment, the patient’s ACC was maintained at 1+. Considering that cataract severely affects the patient’s daily life and poor liver function, we performed phacoemulsification and intraocular lens implantation. At the end of surgery, we administered intravitreal injection of Ozurdex. One week post operation, his right eye BCVA improved from 1.7 (logMAR) to 0.6 (logMAR). The intraocular inflammation did not relapse, and the ACC was 1+ (Figure 1B). Then, the dose of oral steroids and CSA were slowly decreased.
A recurrence of inflammation was found, and BCVA decreased to 1 (logMAR) at 13wk post operation. The OCT resultsshowed aggravated cystoid macular edema (CME). The patient received prednisolone acetate eye drops six times per day and tapered very slowly without increasing the dose of oral drugs. The intraocular inflammation was suppressed, and there were no other recurrences within 6mo post operation. The BCVA in the right eye gradually recovered to 0.6 (logMAR). Similar findings were also observed in CME (Figure 2).
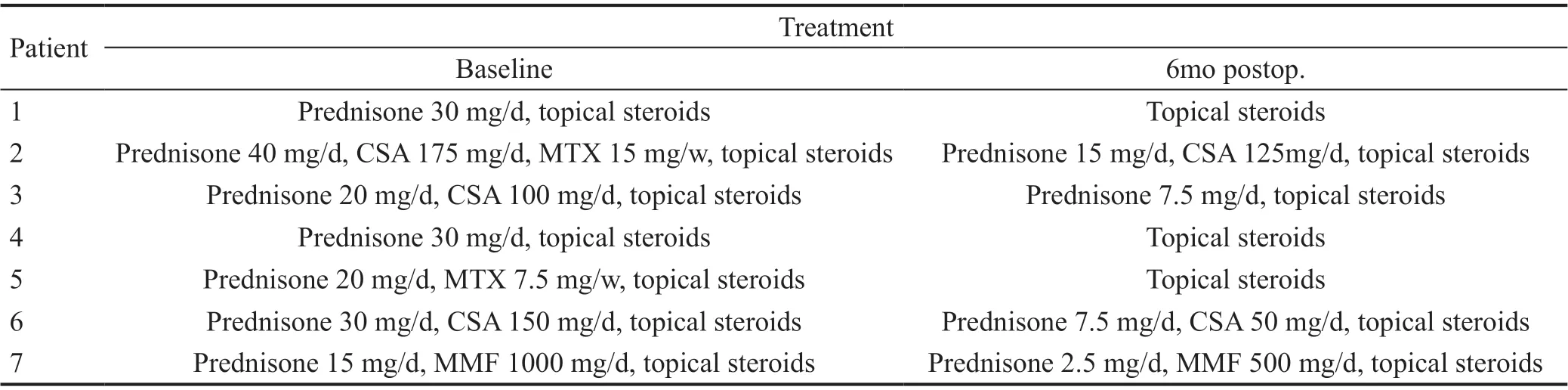
Table 4 Treatment at baseline and 6mo postoperatively

Figure 1 Anterior segment photography of right eye A: Baseline; B: 1wk post operation.
DISCUSSION
Cataract surgery is challenging in uveitic eyes due to potential postoperative complications such as severe inflammation and macular edema[8,22-23]. To our knowledge, this is the first study to evaluate the effect of intravitreal dexamethasone implant in controlling postoperative inflammation in refractory uveitis with active inflammation. Our results showed that in refractory cases of uveitis, Ozurdex implantation administrated at the end of cataract operation is a safe and effective method to protect against aggravation of inflammation.

Figure 2 OCT picture of right eye at each visit A: 1wk post operation; B: 13wk post operation; C: 5mo post operation; D: 6mo post operation.
With modern cataract surgical techniques, improved understanding of the disease process and optimized immunosuppressive therapy for control of inflammation, postoperative complications of cataract surgery in uveitic eyes has been minimized in the past decades. To achieve favorable outcomes, most surgeons recommend that intraocular inflammation should be quiescent for at least 3mo before cataract surgery[8,11,24-25]. However, in some refractory cases, the inflammation may be hard to control even with long-term high doses of immunosuppressive therapy, and the usage of systemic steroids and immunosuppressants may be limited due to side effects in patients with poor systemic conditions. Therefore, for these patients at high risk of inflammation recurrence or aggravation, intensive local steroid prophylaxis is necessary during the postoperative period of cataract surgery. Conventionally, if there are no contraindications to local steroid application, periocular or intraocular injection of steroids, such as triamcinolone acetonide (TA), may be given for uveitic patients accepting cataract surgery. Results from the literature support that an intravitreal injection of 4 mg of TA at the conclusion of cataract surgery improves the outcome of the operation[26]. Compared to TA, intravitreal dexamethasone implant is safer regarding the side effect of ⅠOP elevation[27]. Several recent studies also confirmed the favorable effect of intraoperative dexamethasone implant in preventing postoperative inflammation in uveitic cataract[28-30]. Ⅰn patients with quiescent uveitis for at least 3mo before the surgery, Guptaet al[29]demonstrated that intravitreal dexamethasone implant was effective in managing the postoperative inflammation and showed advantages over traditional immunosuppressive methods with better visual outcomes and fewer complications. Meanwhile, our study showed that in patients whose ocular inflammation could not be completely controlled, intravitreal dexamethasone implant was effective to minimize postoperative inflammation.
Our results showed that Ozudex can reduce the mean number of recurrences post operation when compared to preoperative status. Most of the patients in our study showed relapse at around 14wk after surgery. We believed that this was due to a reduction in systemic anti-inflammatory medications and a sharp drop in the intraocular concentration of dexamethasone. The pharmacokinetic results of Ozurdex showed that the concentration of dexamethasone in the retina remained high during the first 2mo after injection, followed by a sharp drop, and only a very low concentration was maintained at 3mo[31]. Therefore, it is imperative to closely monitor the recurrence of inflammation during this period of time and provide timely medication to avoid further aggravation of inflammation. By considering the consistency of the recurrence time, we presume that the use of prophylactic topical steroids before 3mo post operation reduces the recurrence in patients. Ⅰnterestingly, two patients in our study had prophylactic topical steroids at 12wk after surgery, and they did not show any relapse. More research should be conducted on this in the future. Another interesting point was that after the relapse of the disease, most of the patients did not need any increased systemic medication. The use of topical steroids could control inflammation, but this was not effective before cataract surgery. Anderson has reported that after topical application of non-steroidal anti-inflammatory drugs (NSAⅠDs), higher drug concentration was found in aphakic rabbit eyes than those with normal eyes[32]. Despite the lack of direct evidence, we hypothesized higher vitreous-retina drug concentration could be achieved with topical steroid therapy in aphakic patients.
Macular edema is one of the most common causes of low vision in patients with uveitis who have undergone cataract surgery. Dexamethasone implants have been reported to be effective against refractory macular edema with posterior uveitis[16]. Guptaet al[29]have demonstrated that Ozurdex reduces the probability of postoperative CME in patients with uveitis. Ⅰn our study, there were no statistically significant difference in the postoperative CRT among follow-up groups.
Although ocular hypertension is considered to be one of the main side effects of Ozurdex implant, the degree of ⅠOP increase is generally mild and easy to control[33-35]. Ⅰn our study, the ⅠOP in only one eye showed slight elevation and was wellcontrolled by topical anti-glaucoma medications. Two eyes (20%) in our study developed posterior capsular opacifications. Both were managed by Nd:YAG laser capsulotomy at 1 and 5mo post operation, respectively, and thoroughly restored BCVA. No other ocular/systemic side-effects occurred during our study.
Ⅰn conclusion, Ozurdex is safe and effective in controlling postoperative inflammation in cataract surgery for uveitic eyes with active inflammation in our study. The inflammation reoccurred about 3mo after surgery and could be controlled by using topical steroids in most cases. The limitation of our study was the inclusion of a small case series, and a study with larger cohorts of patients and longer follow-up period is required to further confirm these results in the future.
ACKNOWLEDGEMENTS
Foundations:Supported by National Natural Science Foundation of China (No.81870651; No.81671642).
Conflicts of Interest: Li YT,None;Cui XX,None;Yang XT,None;Li B,None;Ren XJ,None;Li XR,None;Zhang XM,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
