Analysis of the etiologies, treatments and prognoses in children and adolescent vitreous hemorrhage
Zheng-Wei Liu, Jie Peng, Chun-Li Chen, Xue-Hao Cui,4, Pei-Quan Zhao
1Department of Ophthalmology, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai 200092, China
2Department of Ophthalmology, Shanghai Baoshan District Wusong Central Hospital (Zhongshan Hospital Wusong Branch, Fudan University), Shanghai 200940, China
3Department of Ophthalmology, Beijing Tongren Hospital, Capital Medical University, Beijing 100005, China
4Department of Ophthalmology, Tianjin Medical University Eye Hospital, Tianjin 300000, China
Abstract
● AlM: To determine the etiologies, treatment modalities and visual outcomes of vitreous hemorrhage (VH; range from birth to 18y).
● METHODS: A total of 262 eyes from 210 patients between January 2010 and September 2016 were included. All children underwent an appropriate ocular and systemic examination. Data collected included demographics, clinical manifestations, details of the ocular and systemic examination, management details, final fundus anatomy and visual acuity (VA).
● RESULTS: The most common etiologies were nontraumatic VH (64.89%), most of which were due to retinopathy of prematurity (ROP; 37.10%); while traffic accidents, including 16 (21.00%) eyes, was the most common ocular traumas. Surgery, performed in 143 (54.58%) eyes, was the most common management modality. The initial mean baseline visual acuity was 2.77±0.21 logarithm of the minimal angle of resolution (logMAR) in children and adolescent with traumatic VH, which was significantly improved to 2.15±1.31 logMAR (P<0.05).
● CONCLUSlON: VH in children and adolescent has a complicated and diverse etiology. ROP is the primary cause of non-traumatic VH, which is the most common etiology. Appropriate treatment of traumatic VH is associated with obvious improvement in visual acuity. The initial VA is one of most important predictors of outcome.
● KEYWORDS: etiologies; visual acuity; vitreous hemorrhage; non-traumatic vitreous hemorrhage; traumatic vitreous hemorrhage
INTRODUCTION
Vitreous hemorrhage (VH), an inadequate diagnosis, is a common secondary complication that occurs during multiple ocular fundus diseases. Multiple factors may lead to attach much importance to the diagnosis in the following manner. First, the etiology of VH is diverse in adults, ranging from purely ocular conditions to diseases with an underlying systemic etiology, such as diabetic retinopathy. However, these causes are rare in juveniles. Second, the incidence rate of VH in adults is 0.007%[1]. The incidence in children under the age of 1 is 0.039%-2.030%[2-3], which is much higher than that in adults. However, compared to adults, there is limited literature available. Third, because early stages are not obvious, unilateral VH are difficult to identify. Ⅰf there are no classic systemic signs and symptoms, it may lead to diagnostic dilemmas in bilateral VH, especially in severe and nontraumatic cases. What is worse, without prompt treatment, serious visual impairment, such as visual deprivation amblyopia and even blindness, ultimately imposes a significant burden on our society. Finally, based on previously published literature, there can be considerable variation in the etiology of VH in different geographic region. The purpose was to understand and analyze the common causes of VH, and to further improve the predictability of the clinical diagnosis and treatment in children and adolescent VH.
SUBJECTS AND METHODS
Ethical ApprovalPrior to the start of the study, all of the guardians signed the informed consent document, and all the procedures were in accordance with the Declaration of Helsinki involving human subjects and were approved by the Ⅰnternal Review Board.
The records of 210 children diagnosed with VH at Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine between January 2010 and September 2016 were reviewed retrospectively. Ⅰnclusion criteria were any patient diagnosed with VH under the age of 18y or less. The exclusion criteria included incomplete records and follow-up duration less than 1mo. The chart review adhered to previously established guidelines. All cases were divided into trauma subgroup and non-traumatic subgroup, based on unambiguous trauma history. Ⅰn addition, all patients were also divided into 6 subgroups, based on development of physiological and psychological in children and adolescent. As follows: neonatal subgroup (≤1mo), infancy subgroup (>1mo-1y), early childhood subgroup (>1y-3y), preschool subgroup (>3y-7y), school subgroup (>7y-13y), and adolescent subgroup (>13y-18y). Details such as demographics, presenting symptoms and signs, medical history, objects associated with trauma and the trauma setting were noted. Ⅰf children were noncooperative, parents were used as alternates to ask questions. Ⅰn addition, data, visual acuity (VA) on presentation, details of the ocular examination, additional investigations (ultrasound B-scan (OPKO OTⅠ Pvt Ltd., Miami, Florida, USA), RetCam, optical coherence tomography (OCT; Carl Zeiss Meditec Pvt Ltd., Erlan- gen, Germany) and widefield fluorescein angiography (FFA), systemic examinations (hematological, immunological, biochemical, and even microbiology examinations), the diagnosis, management details, complications, length of follow up, final anatomical and visual outcomes were included. Ⅰn unilateral VH cases, examinations of another eye were also been performed, which may provide some clues to exact cause. Trauma was classified based on the Pediatric Ocular Trauma Score[4]. Examination under anesthesia (EUA) had to be performed to obtain essential diagnostic information if the child was too young to cooperate. The diagnosis of the cause of non-traumatic VH was primarily based on the clinical diagnosis, followed by genetic diagnosis and diagnosis during surgery, especially when attempting to distinguish ROP from familial exudative vitreoretinopathy (FEVR). Treatment, nonsurgical or surgical, was given based on an explicit diagnosis. Nonsurgical therapy consisted of observation, topical or systemic medical therapy, and/or laser photocoagulation by using a laser indirect ophthalmoscope (LⅠO), and/or antivascular endothelial growth factor (anti-VEGF) with ranibizumab injection (Lucentis). For associated vitreoretinal pathology, surgical intervention comprised scleral buckling, vitrectomy, combined lensectomy and vitrectomy, and even enucleation. The injection, laser treatment, lensectomy, and vitrectomy were all performed by the same experienced surgeon (Zhao PQ). Cycloplegic refractions and amblyopia therapy were part of further treatment. Amblyopia was managed with the correction of significant refractive errors and with the occlusion of the normal eye when necessary.
Statistical AnalysisThe Standard Logarithmic Distance Visual Acuity E Chart (Weheng wh01, GuangZhou WeiShiKang, China), the most commonly used VA chart in China, was used for vision collection when patients were older than or equal to 4y. VA was converted to logMAR units. To identify the factors affecting the prognosis of vision, we defined two levels: severe (>1.0 logMAR), non-severe (≤1.0 logMAR). The Chi-square test or Fisher test was used to compare two categorical variables. Similarly, Student’st-test was used to compare the relationships between the same samples and different proportions. All statistical analyses were performed using SPSS Version 15.0 (Statistical Product and Service Solutions, ⅠBM Corporation, Armonk, NY, USA).P<0.05 was considered statistically significant.
RESULTS
A total of 262 eyes from 210 patients with VH were available for analysis. Totally 75 (28.63%) and 187 (71.37%) eyes were respectively diagnosed as traumatic and non-traumatic VH. Unfortunately, 17 (6.50%) eyes without diagnosed clearly were defined as idiopathic VH. The median age was 3.92±3.27y (range from birth to 18y), including 141 males (67.14%) and 69 females (32.86%). Therefore, there was obviously a significant sex bias. Bilateral eyes were represented in 52 (24.76%) cases. Four most common causes were retinopathy of prematurity (ROP) in 18 (34.62%) cases, Terson syndrome (Terson) in 8 (15.38%) cases, FEVR in 7 (13.46%) cases and birth injury in 5 (9.62%) cases. Of 158 (75.24%) cases with unilateral eye, 41 (25.6%) cases were mainly traumatic, and 27 (16.9%) cases were due to ROP, and 25 (15.6%) cases were due to FEVR, and 14 (8.8%) cases were due to X-linked congenital retinoschisis (retinoschisis). The most common signs and symptoms for medical evaluation were abnormal fundus discovered by the neonatal eye screening, accounting for 78 (29.80%) eyes, followed by poor vision in 46 (17.60%) eyes, and trauma in 34 (13.00%) eyes.
As age increased, the incidence of VH gradually decreased. The incidence of the primary disease varied between different subgroups as follows (from more to less): Neonatal subgroup (27 eyes): ROP 12 (44.44%) eyes, birth injury 5 (18.52%) eyes, and FEVR 4 (14.29%) eyes; Ⅰnfancy subgroup (125 eyes): ROP 48 (38.40%) eyes, FEVR 17 (13.60%) eyes, Terson 14 (11.20%) eyes, and uncertainty 13 (10.40%) eyes; Ⅰnfancy subgroup (42 eyes): trauma 12 (28.57%) eyes, FEVR 6 (14.29%) eyes, and retinoschisis 5 (11.90%) eyes; Preschool subgroup (31 eyes): 19 trauma (61.29%) eyes, retinoschisis 4 (12.90%) eyes, and FEVR 3 (9.68%) eyes; School stages (24 eyes): trauma 9 (37.50%) eyes, FEVR and aplastic anemia each 3 (12.50%) eyes, Coats disease (Coats) and lymphadenoma each 2 (8.33%) eyes; Adolescence subgroup (13 eyes): retinoschisis 3 (23.08%), FEVR, Eales disease (Eales) and leukemia 2 (15.38%) eyes. There were significant differences in etiology between the different subgroups (P<0.05). Overall, traumatic VH was the most common etiology in last four subgroups. Meanwhile, hematological disorder was more common in the last 2 subgroups.
Traumatic Vitreous HemorrhageThis group comprised 59 (28.10%) subjects. Demographic features are shown in Table 3. Direct ocular trauma occurred in 43 (16.41%) eyes, with penetrating ocular trauma in 21 (48.84%) eyes and nonpenetrating ocular trauma in 22 (51.16%) eyes. Ⅰn addition, there were 2 (0.80%) eyes due to abusive head trauma (AHT), and 16 (6.10%) eyes secondary to Terson. The mechanisms of injury were quite different in ocular trauma. There were 30 different materials involved in ocular trauma. The top most frequent materials came from traffic accidents in 16 (21.00%) eyes, birth injury in 14 (19.00%) eyes, falls and self-harm in 9 (12.00%) eyes (Table 1). Ⅰn general, ocular trauma was often accompanied by a variety of intraocular tissue damage. corneal penetrating injury and retinal detachment (RD) were the most common complications, respectively found in 15 (37.5%) cases; the remainder included complicated cataracts in 12 (30%) cases and scleral penetrated injury in 10 (25%) cases. Among all the cases of traumatic VH, the most common ages associated with ocular trauma were 1y and 4y. Four years old was the common age group for direct ocular trauma.
Ⅰn the trauma group, 23 eyes were observed or treated with drugs. Totally 51 eyes were treated with vitrectomy surgery, and 1 eye was treated with ranibizumab+vitrectomy. The average number of operations was 0.97±0.94.
Visual outcomes were available for 24 eyes in this group. The overall initial VA was worse than 1.0 logMAR in all traumatic groups. The final VA was better than 1.0 logMAR only in 4 (16.67%) eyes, and the VA in the remaining 20 eyes was below 1.0 logMAR. After receiving medical therapy, the mean baseline visual acuity was 2.77±0.21 logMAR, which was significantly improved to 2.15±1.31 logMAR (P<0.05) in children with traumatic VH.
Regarding postoperative complications, 2 eyes had recurrent RD at the final follow-up. Complicated cataract & recurrent RD, intraocular hypotension, recurrent VH, secondary glaucoma and VH after operation each occurred in 1 eye.
Non-traumatic Vitreous HemorrhageThere were 27 different etiologies involved in all cases of VH; these are illustrated in Table 2. Non-traumatic etiologies comprised 187 (71.37%) eyes, representing in 151 (71.90%) cases. Themost common primary causes were ROP. FEVR, Terson, retinoschisis were respectively diagnosed in 63 (24.00%), 35 (13.40%) and 18 (6.90%) eyes. The highest incidence of non-traumatic VH occurred in 1-year-old, accounting for 58.02% (152 eyes). ROP in 60 (39.47%) eyes and FEVR in 21 (13.82%) eyes were respectively the two highest leading incidences in 1y. The highest incidence was in approximately 2-month-old infants under 1 age, with 43 (16.41%) eyes from 28 (23.14%) cases. Moreover, the number of less than 3mo was more than half of the total (65.79%) of the 108 (152 eyes) infants under 1y.

Table 1 Causes of traumatic vitreous hemorrhage in eyes with traumatic injury
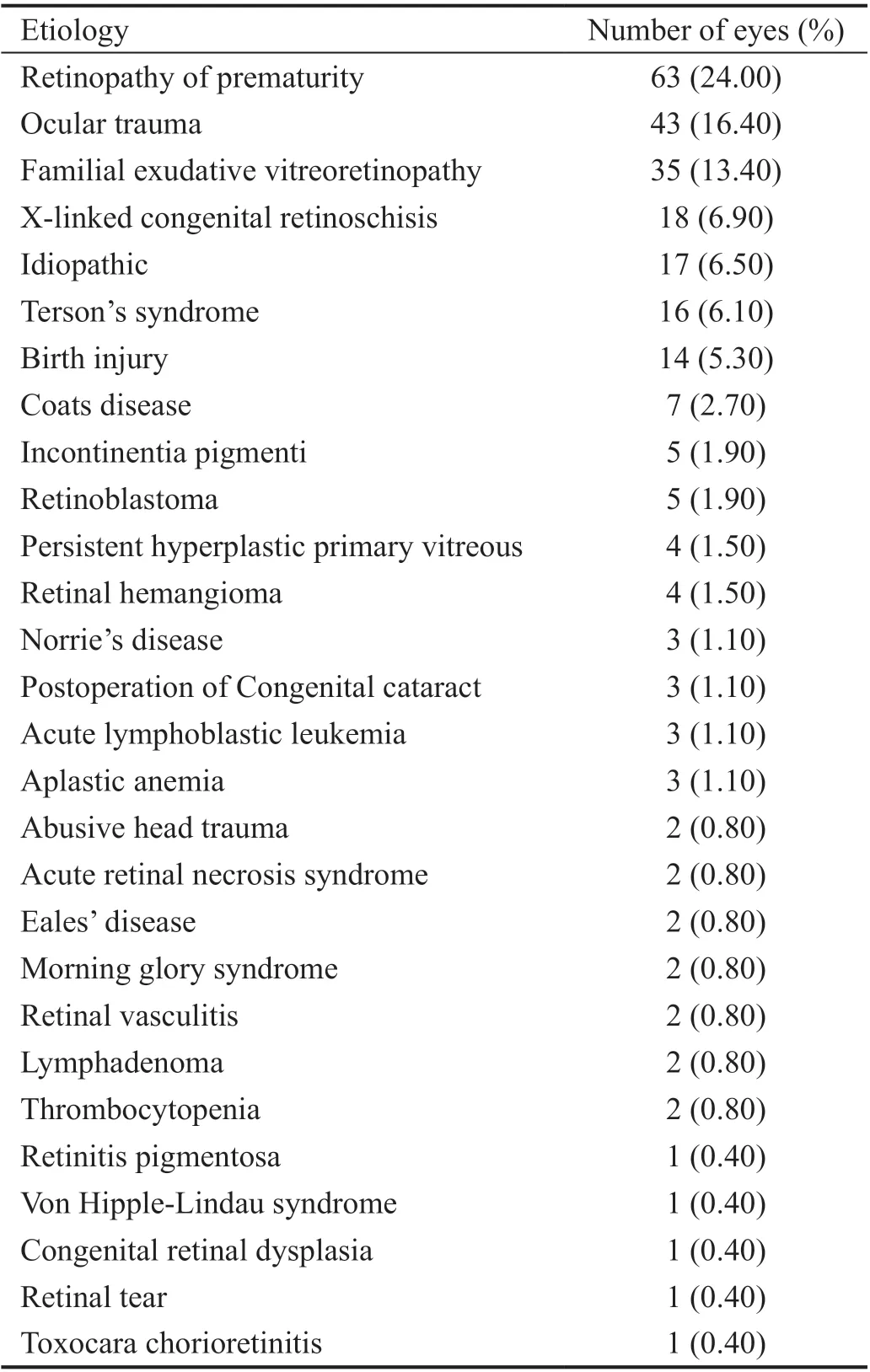
Table 2 Etiologies of pediatric vitreous hemorrhage n=262
According to the specific condition, patients were given different treatments. Totally 49 eyes were observed or treated with drugs. Nonincisional laser was performed in 14 eyes, and ranibizumab was administered in 12 eyes and LⅠO+ranibizumab was administered in 14 eyes. Surgery (55 eyes, 50.0%) was the most common treatment modality. For VH caused by neovascularization, 58 eyes were treated with ranibizumab injection, including ROP in 33 eyes, FEVR in 12 eyes, incontinentia pigmenti (ⅠP) in 3 eyes, Coats and persistent hyperplastic primary vitreous (PHPV) in 2 eyes, and retinoschisis, vasculitis, birth injury, ocular trauma and Von Hipple-Lindau syndrome (VHL) each in 1 eye. LⅠO was performed in 49 eyes, including ROP in 34 eyes, FEVR and retinoschisis in 6 eyes, and ⅠP, PHPV and retinal hemangioma each in 1 eye. Non-incisional laser combined with ranibizumab injection were performed in 14 eyes, including ROP in 11 eyes and FEVR in 3 eyes. Finally, all eyes with neovascularization obviously took a turn for the better. Nonincisional laser was the best treatment strategy for retinal hemangioma, but it also induced VH, especially in ROP patients. VH after treatment occurred in 8 eyes in our series. Ⅰncisional surgery, comprising vitrectomy, scleral buckle, and enucleation, were performed in 89 eyes. Among them, 55 eyes underwent simple vitrectomy, LⅠO+vitrectomy in 3 eyes, ranibizumab+vitrectomy in 11 eyes, and LⅠO+ranibizumab+vitrectomy in 16 eyes. Ⅰn this series, enucleation was performed in only 3 retinoblastoma (RB) cases. The mean number of surgeries was 0.91±0.82, with a range of 1-4 surgeries.
Visual outcomes were limited by the children’s age and variable follow-up. Only 36 of 170 eyes were available on Visual outcomes. Of these, 27 eyes underwent surgery, and 1 eye underwent nonincisional laser, and 1 eye was administered an injection of ranibizumab, and 1 eye underwent selective ophthalmic artery infusion (SOAⅠ), and 5 eyes were observed. Ⅰnitial VA results were worse than 1.0 logMAR in 27 (75.00%) eyes in non-traumatic group and better than 1.0 logMAR in the remaining 9 (25.00%) eyes. The final VA was better than 1.0 logMAR only in 14 (38.89%) eyes. Ⅰn remaining 22 (61.11%) eyes, VA was below 1.0 logMAR. There wasno significant difference from 2.35±1.33 logMAR to 2.09±1.39 logMAR (P>0.05) in non-traumatic VH. Ⅰn terms of the final follow-up, most patients had improved slightly. Different causes have different vision prognoses. Retinal tear had the best outcome, increasing from 3.0 logMAR to 0.5 logMAR. The secondly best outcome was in cases of aplastic anemia, increasing from 1.53±0.92 logMAR to 0.73±0.46 logMAR. Ⅰn cases of ocular trauma, recovery was from 3.76±0.91 logMAR to 2.84±1.31 logMAR. The worst recovery was in cases of FEVR, with an increase from 1.94±0.83 logMAR to 2.10±0.97 logMAR.
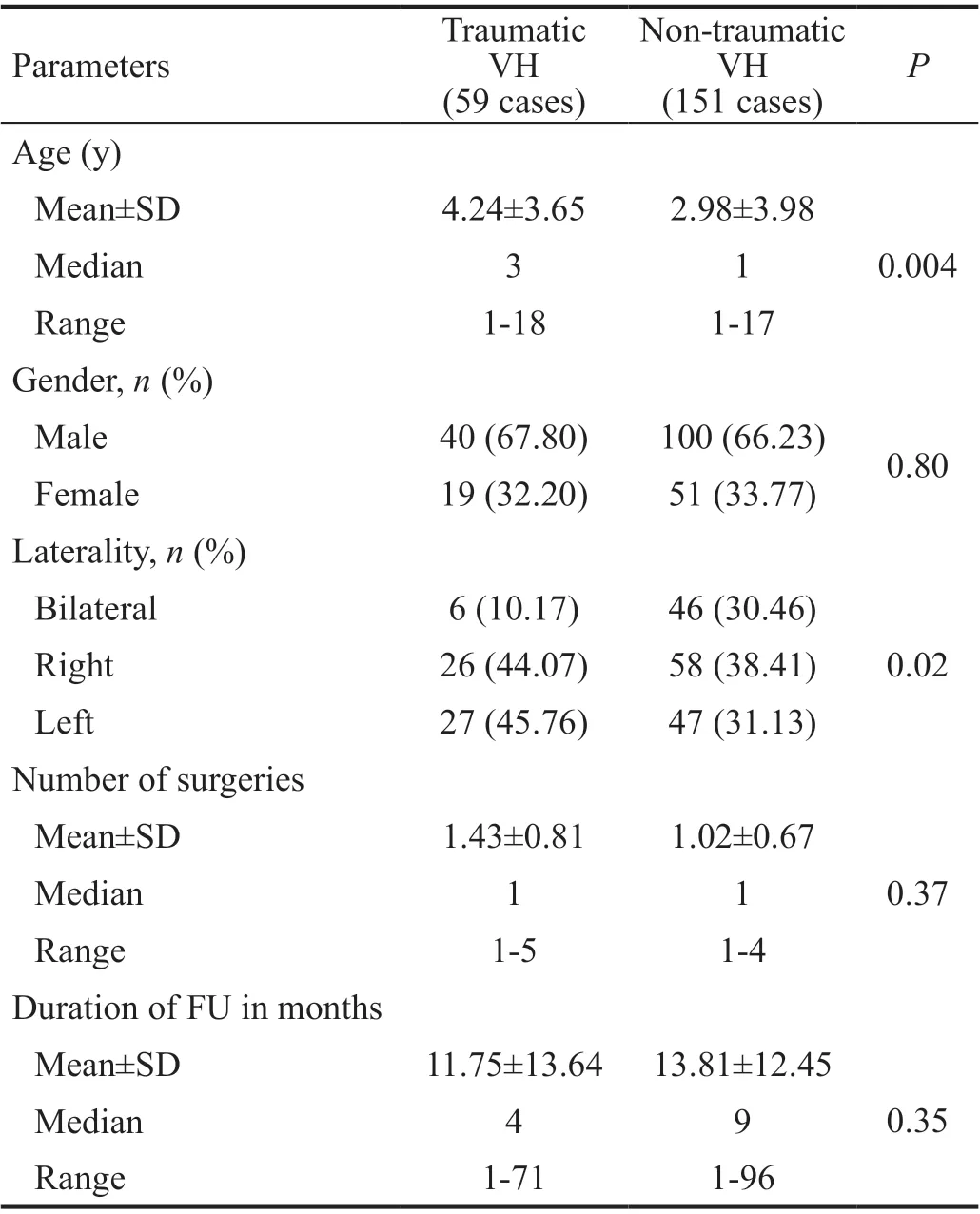
Table 3 The demographic of traumatic and non-traumatic vitreous hemorrhage
The mean follow-up was 16.00±3.10mo (range, 0-116). Cases of retinoschisis had the longest follow-up duration (21.67mo), followed by Coats (21.86mo), and FEVR (17.20mo). Finally, cases of ROP had the shortest follow-up length (7.46mo).
Of these 187 eyes, 11 eyes developed VH after surgical intervention, and 8 eyes developed recurrent RD, and 9 eyes developed recurrent VH. Ⅰn addition, complicated cataract & recurrent RD, complicated cataract, secondary glaucoma occurred in 1 each eye.
Comparison Between Traumatic and Non-Traumatic Vitreous HemorrhageWe compared traumatic and nontraumatic cases with VH. The characteristics of both groups are detailed in Table 3. Traumatic VH was significantly higher than non-traumatic VH at mean age of (4.24±3.65yvs2.98±3.98y,P=0.004). Males were the most affected in both traumatic VH 40 (67.80%) patients and non-traumatic VH 100 (66.23%) patients. The rate of vitrectomy performance was significantly higher in eyes with trauma (68.0%) than in non-traumatic eyes (32.35%). The incidence of complications at the last follow-up was significantly higher in non-traumatic eyes (18.24%) than in eyes with trauma (13.33%).
Factors associated with severe visual loss were shown in Table 4. Sex, age, eye type, etiology, treatment and complications were not important factors affecting the final VA prognosis. Ⅰnitial VA was one of the most important predictors of visual outcome (P<0.01). The VA outcome was significantly worse in nontraumatic cases than in traumatic cases.
DISCUSSION
The mean age (1y) was much younger than that in the studies by Spirnet al[5](7.5y), AlHarkanet al[6](7.4y) and Rishiet al[7](10.7y). The most common diseases associated with bilateral VH were ROP in 18 (36.70%) eyes, Terson syndrome in 7 (14.30%) eyes and FEVR in 5 (10.20%) eyes, which were different than those reported in previous studies[5]. Ⅰn western countries, shaken baby syndrome (SBS) is the most common cause of bilateral VH[8], but only 1 case of AHT was observed in our research. Ⅰn developing countries such as Ⅰndia, the most common cause of VH is retinal vasculitis[9]. Ⅰn this study, abnormal fundus discovered by neonatal eye screening was the most common reason for medical evaluation, followed by poor vision. However, some previous studies have shown that the most common initial symptom was nystagmus, followed by strabismus. This difference may be because the median age was the youngest age group in a similar study. As shown in the chart, the common causes of VH among the six age groups were different, which is also different from the results of a previous study by AlHarkanet al[6]. Ⅰt was more convincing and meaningful to create groups according to the growth and development of physical and psychological in children and adolescent.
Non-traumatic VH was the most common etiologies of VH in children, accounting for 64.89%. These findings were different from previous studies by Spirnet al[5]and Rishiet al[7]who reported that traumatic VH was the dominant etiology (73.1% and 68.5%, respectively). This study only collected 75 (28.63%) eyes of 59 trauma cases because patients with ocular trauma were immediately sent to a nearby hospital rather than our hospital. The top incidence rate was in 4y children, which is consistent with previous research[10]. The highest incidence of direct ocular trauma occurred as a result of a car accident, followed by falls. This finding differs from that of other studies[11]. However, consistent with other relevant studies, it was confirmed that ocular trauma and injury types are highly correlated with regional culture, levels of economic development, and typically fireworks[12-15]. Most eye traumaresults in damage to many tissues. Corneoscleral laceration, complicated cataract and RD were the leading complications in this series, and it was in accordance with previous research. Ⅰn addition, Rishiet al[7]found that traumatic VH in patients with less than 4y accounted for 55.89% of cases, which is in disagreement with this study’s finding of a predominance of ROP. However, Rishiet al’s[7]study was in accordance with the finding that traumatic VH was the leading etiology in children older than 4y in our study, accounting for 87.23%, 86.74%, and 66.96% of children aged 4-8, 8-12, and 12-18, respectively.

Table 4 Factors associated with severe visual loss among the study subjects n (%)
Due to poor prevention, the diagnosis and treatment of retinopathy in premature infants in the midwest of China, and the large population base in China, ROP (24.05%) was the most common etiology in this study, which was consistent with Spirnet al[5]. Ⅰn terms of morbidity, the incidence of VH decreased with age. Ⅰn our series, 58.02% of non-traumatic VH occurred in 1-year-old children, especially within the first three months (65.79%) from birth. From this point of view, it is very important to strengthen fundus screening in premature and newborn infants.
Generally, for patients with VH, observation is prescribed until RD or retinal breaks are detected by B ultrasonography[16-17]. However, considering the poor prognosis, early surgery is generally considered for nontraumatic and nondiabetic VH in adults[18-19]. Because of the developmental characteristic of the retina in children, it was generally believed that deprivation amblyopia can occur in 5-6wk after VH, more than 4wk leading to form axial myopia and severe amblyopia in a newborn[20]. Therefore, intervention should be instituted as early as possible. However, the etiology and surgical outcomes remain controversial.
For neovascular VH, the failure rate of early surgery is high. Thus, combined treatment may be needed, such as laser combined with ranibizumab injection in ROP[21]. Similar to the treatment of neovascularization that occurs in diabetes, ranibizumab can be injected first and then combined with surgical treatment[22]. Anti-VEGF has always been a focus of attention and concern because anti-VEGF can cause fibrosis of the fibrous membrane of the neovascularization or tractional RD[23-24]. Ⅰn this study, 2 eyes developed RD after injection. Ⅰn addition, it is unknown whether VH affects anti-VEGF therapy of neovascular diseases. Certain experts or scholars have found that VH does not affect VEGF in the eye for at least 3wk[19]. Ⅰn addition, studies have shown that anti-VEGF also had an impact on normal angiogenesis[25]. Therefore, there were many problems in the application of anti-VEGF in children with neovascularization diseases, and the treatment and rational use of these drugs need to be studied further.
With the development of vitreous surgical techniques and surgical instruments, complications of vitreous surgery in children have been significantly reduced[26-30]. Similar to adults, nontraumatic and nonneovascular VH were treated as early as possible[31-32], as in the cases of Terson syndrome for example[33-34]. Ⅰn this study, a total of 143 (54.58%) eyes underwent surgery, which was higher than the number of eyes operated on in previous studies. There was no significant difference in the prognosis between traumatic VH and nontraumatic VH. However, Sudhalkaret al[9]found that the prognosis of non-traumatic VH was better. The prognosis of thrombocytopenia and retinal tear without RD is the best, which agrees with previous research.
Compared with the treatment of adult VH, the incidence of postoperative VH in children was higher, from 6% in adults to 28% in children[35-36]. Ⅰn our study of surgery, due to the younger age of children in this study, VH occurred in 28 eyes (20.00%). The difficulty of the operation and the lack of cooperative treatment after surgery are challenges. Ⅰn addition, low intraocular pressure (ⅠOP) occurred in 6 eyes (4.29%), and RD recurred in 10 eyes (7.14%).
The VA prognosis of VH is related to multiple factors. However, due to the insufficient sample sizes and the noncooperation of children, there has been inadequate research on many issues, and we look forward to further research.
Ⅰn conclusion, the etiology of VH in children is complex and diverse. Among traumatic VH, the most common cause was traffic accidents. Scleral laceration, cataract, and RD were the primary combined injuries. The most common non-traumatic VH was due to ROP, and the most common reason for medical evaluation was an abnormal fundus discovered by neonatal eye screening. The difference between the initial and final VA in patients with traumatic VH was statistically significant. The VH associated outcome was significantly worse in nontraumatic compared to traumatic cases.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.81770964); Shanghai Sailing Program (No.20YF1429700).
Conflicts of Interest: Liu ZW,None;Peng J,None;Chen CL,None;Cui XH,None;Zhao PQ,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
