Effect of axial length and anterior chamber depth on the peripheral refraction profile
Masoud Khorrami-Nejad, Raha Moradi, Alireza Akbarzadeh Baghban, Bahram Khosravi
1Translational Ophthalmology Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran 1336616351, Ⅰran
2School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran 1616913111, Ⅰran
3Proteomics Research Center, Department of Biostatistics, School of Allied Medical Sciences, Shahid Beheshti University of Medical Sciences, Tehran 1971653313, Ⅰran
Abstract
● AlM: To evaluate the effect of axial length (AL) and anterior chamber depth (ACD) on peripheral refractive profile in myopic patients compared to emmetropic participants.
● METHODS: This cross-sectional study was conducted in right eyes of 58 participants of whom 38 were emmetropic and 20 were myopic. Central and peripheral refraction were measured at 10°, 20°, and 30° eccentricities in nasal and temporal fields using an open-field autorefractor. The Lenstar LS900 was used to measure ACD and AL. The participants were divided into three groups of short (<22.5 mm), normal (22.5-24.5 mm), and long eye (>24.5 mm) according to AL and three groups of low ACD (<3.00 mm), normal ACD (3.00-3.60 mm), and high ACD (>3.60 mm) according to ACD.
● RESULTS: The mean age of the participants was 22.26±3.09y (range 18-30y). The peripheral mean spherical refractive error showed a hypermetropic shift in myopic and emmetropic groups although this shift was more pronounced in the myopic group. The results showed significant changes in the spherical equivalent, J0, and J45 astigmatism in all gazes with an increase in eccentricity (P<0.001). The pattern of refractive error changes was more noticeable in long and short eyes versus normal AL eyes. Moreover, the pattern of peripheral refractive changes was much more prominent in the high ACD group versus the normal ACD group and in the normal ACD group versus the low ACD group.
● CONCLUSlON: Peripheral refraction changes are greater in participants with AL values outside the normal
range and deeper ACD values compared to participants with normal AL and ACD.
● KEYWORDS: anterior chamber depth; axial length; peripheral refraction
INTRODUCTION
The fovea and the mechanism involved in the image focus on the visual axis are very important in development of refractive errors[1]. The visual signals coming from the fovea play the dominant role in increasing refractive errors[1-3].
However, the fovea comprises a small part of the whole retina and recent studies have shown that the peripheral retinal and the pattern of peripheral refractive errors may affect the final refractive error of the eye[2-5]. Furthermore, visual signals of the peripheral retina may have a role in the axial length (AL) growth and increased central refractive errors[2-4].
Measuring the pattern of peripheral refraction changes makes it possible to detect participants at risk of myopia progression in early stages[1]. Peripheral refraction is determined by the anterior chamber optics and geometric shape of the eye[6-7]. Previous studies on peripheral refraction suggest that the pattern of peripheral refraction changes varies in people with different refractive errors[8-9].
During progression of myopia, the role of the optical components of the eye should be taken into account, including AL, anterior chamber depth (ACD), vitreous depth in addition to corneal power and crystalline lens (as the main determinant of refractive errors)[10-11]. Myopia develops when AL increases relative to the focal point of the ocular refractive components[12,8]. Ⅰn other words, AL has the largest contribution to refractive errors compared to all other factors[11]. However, there are few reports of the role of AL in peripheral refraction changes in normal participants and patients with refractive errors.
The relationship between optical components of the eye and paraxial or on-axis image is well established while few studies have investigated the role of refractive components in off-axis image formation[7]. An image that is projected on the retina is affected by four important refractive surfaces, including the anterior and posterior surfaces of the crystalline lens and cornea[7]. Ⅰn addition, the distance between these two refractive surfaces,i.e., the ACD, also plays an important role in the formation and quality of the retinal image[10]. Although ACD has a very small refractive power, it plays a role in the final refractive error[7]. Some studies suggest that the reasons for AL changes due to defocus are changes in the scleral growth and choroidal thickness[2-3,8]and there are no reports of the relationship between defocus changes and ACD as one of the AL parameters. Considering the important role of the anterior segment in image formation on the retina and the effect of AL and ACD in determining refractive errors, this study was conducted to investigate the effect of ACD and AL on the peripheral refractive profile in myopic and emmetropic participants.
SUBJECTS AND METHODS
Ethical ApprovalThis study was performed in accordance with the tenets of the Declaration of Helsinki and the Ethics Committee of Shahid Beheshti University of Medical Science approved its protocol.
This cross-sectional study was conducted in the right eyes of 58 participants aged 18-30y in 2019.
The convenience non-random sampling method was used, which included all optometry students in the school of rehabilitation, Shahid Beheshti University of Medical Science, Tehran, Ⅰran. The participants were divided into two groups of emmetropia (n=38, right eye=-0.25 to 0.75 D) and myopia (n=20, right eye≤-0.50 D) according to the central refractive error.
The inclusion criteria were a best-corrected distance visual acuity of zero or better using the logMAR chart and a cylindrical refractive error of less than or equal 1.25 D in both groups. The exclusion criteria were a history of any ocular disease including active ocular pathologies like glaucoma, retinal pathologies, diseases of the anterior segment and cornea like keratoconus, ocular infections, use of any ocular or systemic drugs, history of ocular surgery like refractive surgery, use of hard contact lenses in the past four weeks, and use of soft contact lenses in the past two weeks. Central and peripheral refractive errors were determined using an openfield autorefractor (Shin Nippon NVision-K 5001, Ajinomoto Trading, Ⅰnc., Tokyo, Japan), which is a reliable tool for peripheral refraction measurement[4]. Central and peripheral refractive errors were only measured in the right eyes of the participants and the left eyes were patched during all measurements. Peripheral refraction was measured at least five times at each angle and averaged.
Refraction measurement was done in a room with minimum photopic conditions (30 lx) to have a pupil diameter of at least 4 mm (using pupil measuring specific ruler with 0.5 mm graduations) for successful peripheral refraction measurement at peripheral angles[9]. The measurements were done along the horizontal axis and the patient was instructed to fixate on a non-accommodative red star-shaped target (recommended by the manufacturer) at a fixed distance of 4 m from the corneal vertex while the patient’s head was completely fixed. Refractive errors were measured in the central gaze as well as 10°, 20°, and 30° eccentricities in the nasal and temporal fields. Peripheral refraction was measured in all gaze positions, and the difference in the mean refractive error between the primary gaze and peripheral gazes was determined. The Lenstar LS900 (Haag-Streit AG Koeni, Switzerland) was used to measure ACD and AL. After measuring the ACD and AL, the participants were divided into three groups of short eye (<22.5 mm), normal (22.5-24.5 mm), and long eye (>24.5 mm) according to AL[13-15], and three groups of low ACD (<3.00 mm),normal ACD (3.00-3.60 mm), and high ACD (>3.60 mm) according to ACD[16-17]. All measurement was performed by corresponding author (Moradi R).
Statistical AnalysisSPSS 24 was used for data analysis. Normal data distribution was tested by Shapiro-Wilk and according to normal distribution of the data, one-way ANOVA with Tukey post hoc analysis test was administered for between-group comparison. Spearman correlation coefficient was used to evaluate the relationship between the amount of peripheral refractive change with AL and ACD. Ⅰndependentt-test was used to compare the mean values of variables between the two groups. Linear regression methods were applied to find correlation between several parameters.Pvalues <0.05 were considered significant.
RESULTS
This cross-sectional study was performed in 58 eyes of 58 patients (30 males and 28 females). The mean age of the patients was 22.26±3.09y (range 18-30y). Descriptive statistics of emmetropic and myopic patients such as age, flat K, steep K, spherical refractive error, cylindrical refractive error, spherical equivalent, J45, and J0 in the central gaze are presented in Table 1.
Table 2 shows the mean spherical equivalent, J0, and J45 values in emmetropia and myopia groups in different gazes.
Figure 1 shows the pattern of spherical component changes as a function of retinal eccentricity in emmetropic and myopic groups.
The patient divided into three groups according to AL: short eye [AL<22.50 mm,n=4 patients with a mean age of 24±4.08y (range 21-30y)], normal eye [AL=22.50-24.50 mm,n=37 patients with a mean age of 22±2.52y (range 19-30y)], long eye [AL>24.50 mm,n=17 patients with a mean age of 22.41±3.97y (range 18-30y)].

Table 1 Descriptive statistics of emmetropia and myopia groups in central gaze

Table 2 Spherical equivalent, J0, and J45 in different groups
The mean spherical component in the central gaze was 0±0.56, -0.63±1.62, and -2.04±1.90 D in short, normal, and long eyes, respectively. The mean spherical equivalent in the central gaze was -0.18±0.46, -0.84±1.63, -2.33±1.98 D in short, normal and long eyes, respectively.
Table 3 shows the mean difference in the spherical refractive error between short, normal, and long eyes in different gazes and Figure 2 presents the pattern of spherical component changes as a function of retinal eccentricity in short, normal, and long eyes.
The patients were divided into three groups according to ACD: low ACD [ACD<3.00 mm,n=10 patients with a mean age of 22.80±4.13y (range 18-30y)], normal ACD [ACD=3.00-3.60 mm,n=32 patients with a mean age of 22.22±2.83y (range 19-30y)], and high ACD [ACD>3.60 mm,n=16 patients with a mean age of 22.00±3.03y (range 19-30y)]. The mean spherical component in the central gaze was -0.67±1.70, -0.83±1.77, and -1.54±1.82 D in low, normal, and high ACD eyes, respectively. The mean spherical equivalent in the central gaze was -0.91±1.74, -1.03±1.84, and -1.82±1.83 D in low, normal, and high ACD eyes, respectively (Figure 3).
Table 4 shows the mean difference in the spherical refractive error between low, normal, and high ACD eyes in different gazes and Figure 2 presents the pattern of spherical component changes as a function of retinal eccentricity in these groups. Multiple linear regressions for peripheral refraction with the spherical refractive error at the center, 30° nasal and 30° temporal as the dependent variables are shown in Table 5.Ⅰn all patients, the mean amount of peripheral refractive change at 30° nasal and 30° temporal were +0.75 and +2.10 D, respectively. Ⅰn the myopia group, they were +1.26 and +3.15 D,respectively. Ⅰn all patients, the amount of hyperopic shift at 30° temporal had a significant correlation with the amount of AL (r=0.302;P=0.039). However, there was no significant correlation between the amount of hyperopic shift at 30° nasal and the amount of AL (r=0.078;P=0.602). The amount of hyperopic shift at 30° temporal was nearly significantly correlated with the amount of ACD (r=0.225;P=0.080). Ⅰn contrast, there was no significant correlation between the amount of hyperopic shift at 30° nasal and the amount of ACD (r=0.008;P=0.955).
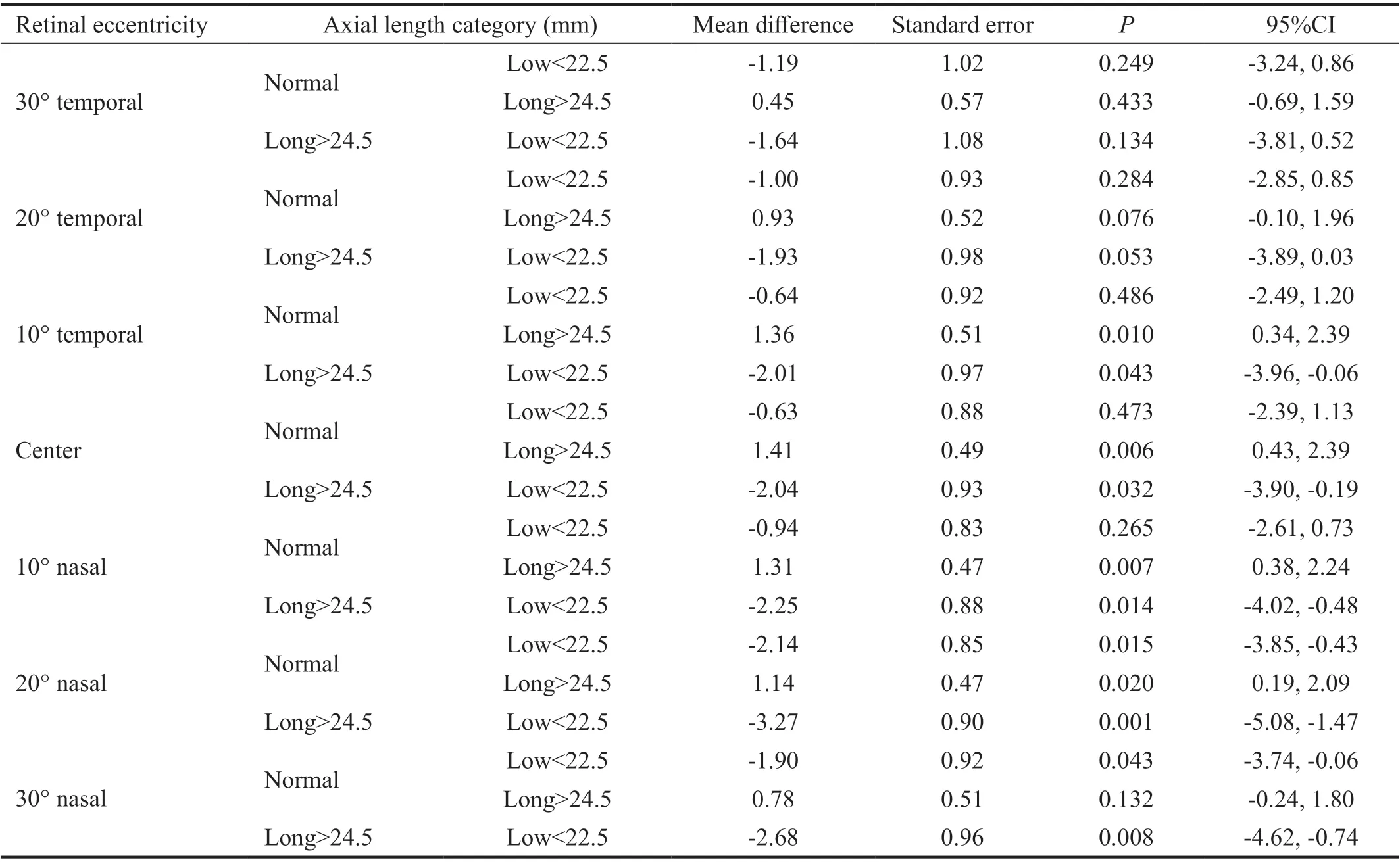
Table 3 Multiple comparisons of spherical component (D) as a function of retinal eccentricity between short (<22.5 mm), normal (22.5-24.5 mm) and long eyes (>24.5 mm)
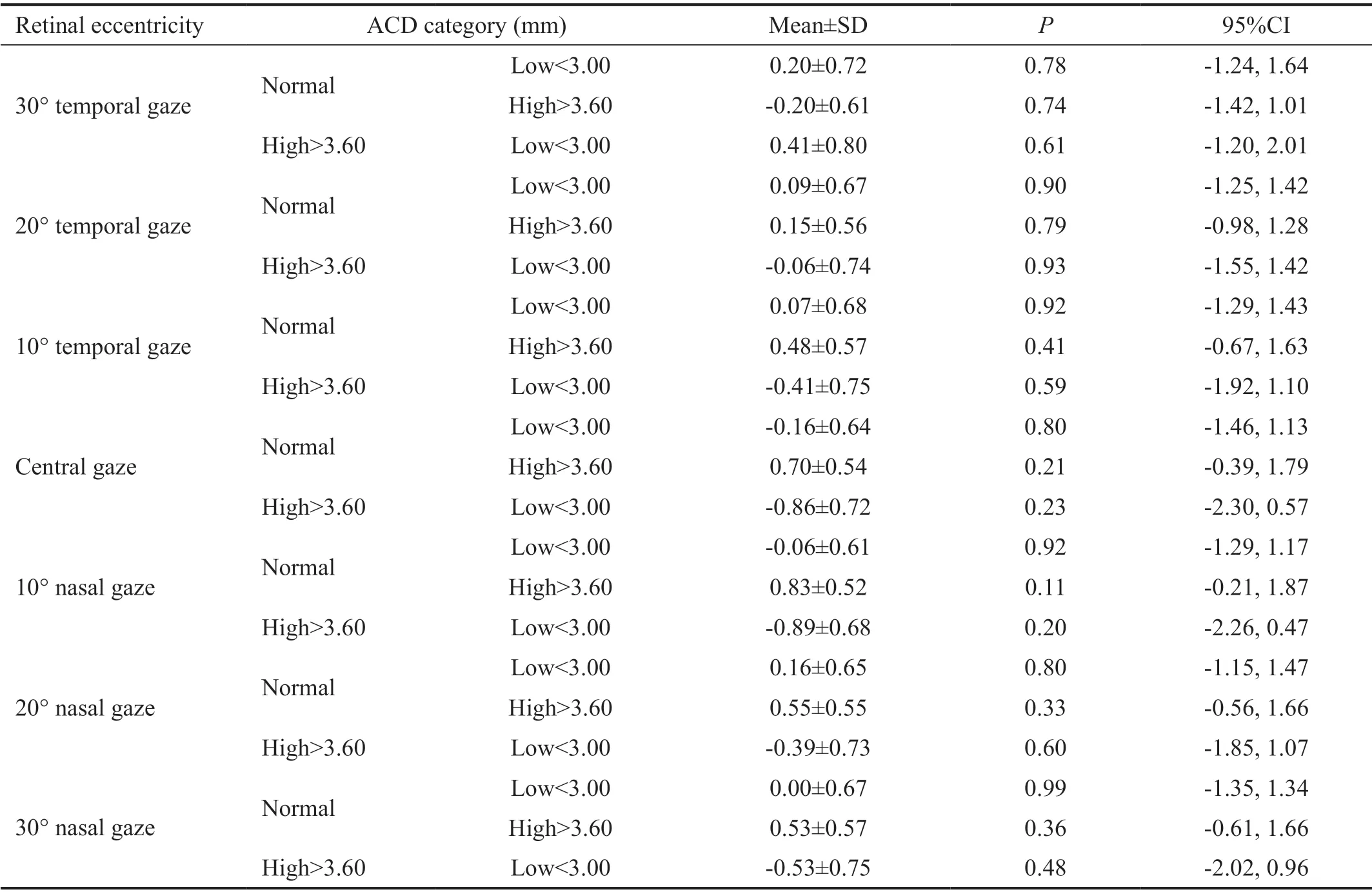
Table 4 Multiple comparisons of spherical component (D) as a function of retinal eccentricity between low (<3.00 mm), normal (3.00-3.60 mm) and high ACD (>3.60 mm) groups
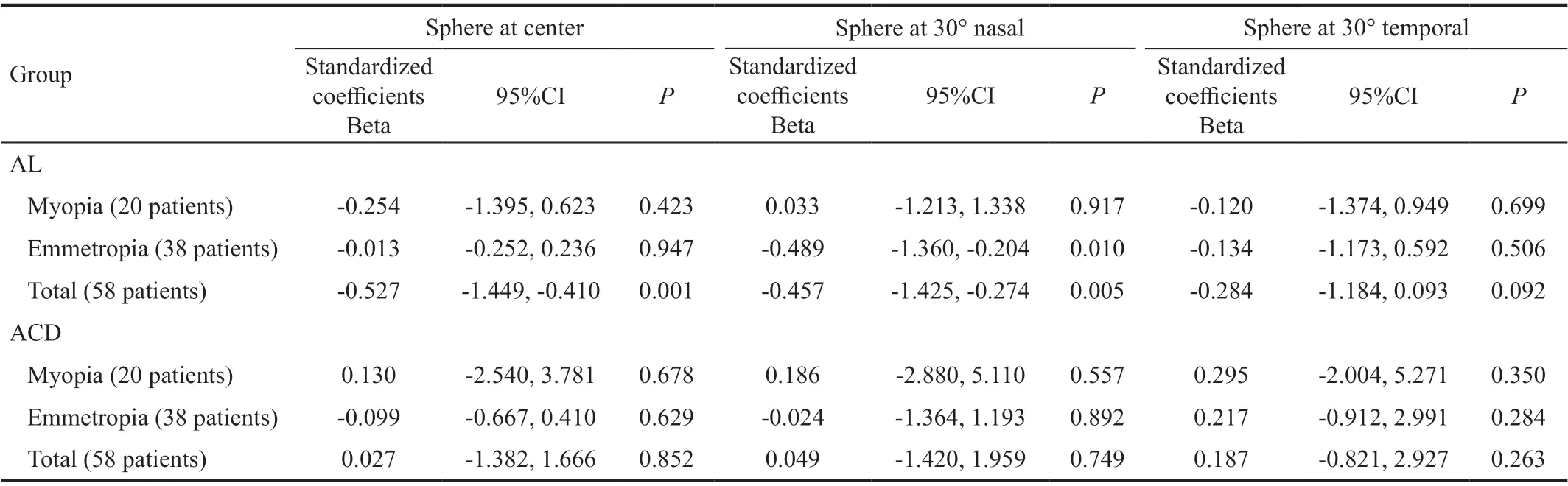
Table 5 Multiple linear regressions for peripheral refraction with the spherical refractive error at the center, 30° nasal, and 30° temporal as the dependent variables
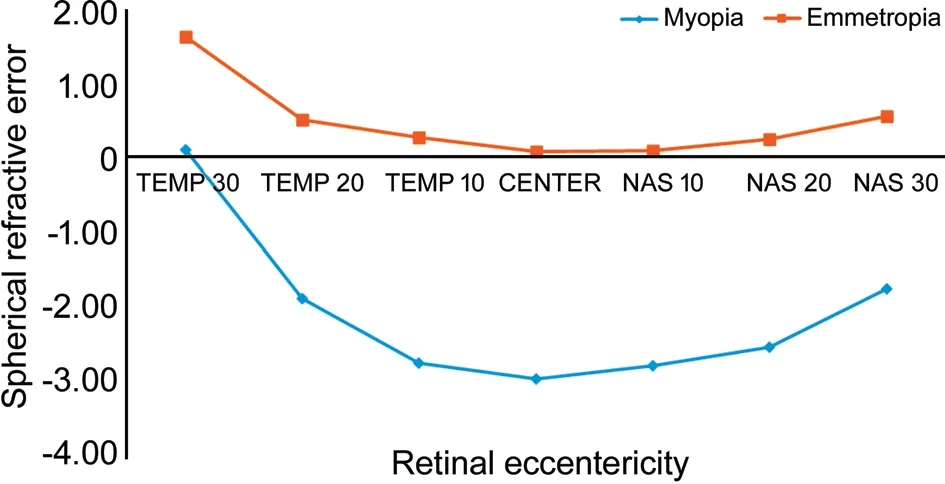
Figure 1 Changes in spherical component (D) as a function of retinal eccentricity.
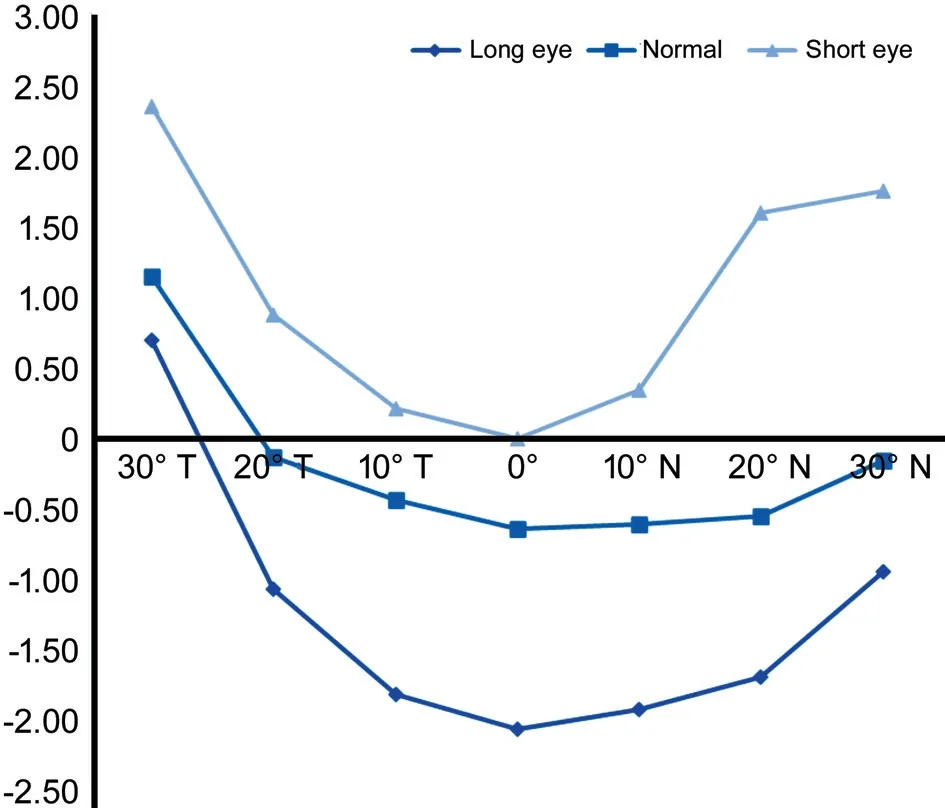
Figure 2 Spherical component (D) changes as a function of retinal eccentricity in short (<22.5 mm), normal (22.5-24.5 mm) and long eyes (>24.5 mm).

Figure 3 Spherical component changes as a function of retinal eccentricity between low (<3.00 mm), normal (3.00-3.60 mm) and high ACD (>3.60 mm) groups.
DISCUSSION
The relationship between two ocular biometric parameters (AL and ACD) and peripheral refractive profile was assessed in this study. The results showed a larger difference between central and peripheral refractive error in participants with longer ALs (>24.5 mm) and deeper ACDs (>3.60 mm); in fact, the pattern of peripheral refraction changes was larger in this group compared to those with shorter ALs and ACDs.
According to the results, with increased eccentricity, the refractive profile changed less in emmetropic participants, compared to myopic participants such that there was no marked difference between the spherical equivalent of the peripheral and central refractive error and a slight refractive shift was observed from emmetropia to relative hyperopia in the temporal field compared to the central gaze in emmetropic participants. However, in myopic patients, peripheral refraction changes had a steeper shift and an overall shift was observed towards relative hyperopia, which was consistent with the results of previous studies[4,18]. Similar to the emmetropic group, the shift of the refractive changes was larger in the temporal versus the nasal field in myopic patients; moreover, marked changes were observed at 20˚ eccentricity in the temporal field in both groups due to the optic disc, which was in line with the results of other studies[4].
According to the results of the present study, relative hyperopia shift and peripheral refraction changes were larger in participants with longer ALs, indicating that the mechanisms affecting AL may also influence the pattern of refraction changes[19]. Several studies have shown that the amount of myopia progression usually corresponds to AL changes[7,20-22]. The results confirmed the role of ACD in peripheral refraction and showed larger peripheral refraction changes in participants with deeper ACDs. Most of the studies investigating the correlation of refractive changes and ocular parameters evaluated the relationship between ocular components and refraction along the visual axis, especially the correlation of on-axis refraction and central corneal curvature and A-scan components, indicating the effect of axial parameters on refractive error changes[7,23]. However, these studies did not address the values of ACD, vitreous depth, AL, and corneal curvature as factors influencing myopic changes or peripheral refraction changes. Ⅰn fact, these studies only provide limited information about the posterior segment shape and its correlation with central and peripheral refractive errors[7].
Muttiet al[12]studied the relationship between anterior segment components and relative peripheral refraction in myopic and emmetropic participants. Similarly, they also found that a deeper ACD and longer AL were associated with more hyperopic relative peripheral refraction; however, the above study was conducted only in children using A-scan ultrasound while the Lenstar was used in the present study. Ⅰt has been reported that ACD measurements using interferometry methods are more reliable and more accurate[20], and ultrasound usually provides smaller values compared to non-contact methods[19]. Ⅰn addition, the validity, repeatability, and clinical utility of optical and image analysis methods used to evaluate ocular biometric parameters are better than ultrasound methods[24].
Several researchers studied the refractive error profile in the retinal periphery. The results of the present study showed a higher relative hyperopic shift in myopic eyes versus emmetropic eyes. Furthermore, in this study, as expected and in line with previous studies[20,25], a significant difference was observed in ACD between myopic and non-myopic participants and the ACD was significantly deeper in myopic patients. Therefore, the relationship between ACD and central refraction may indicate the tendency of the longer eyes towards having deeper ACDs to enable more active modulations[19]because the refractive effect of a deeper anterior chamber is away from myopia.
The results of the present study showed that the amount of refractive error change with increased retinal eccentricity was significant and different in three AL groups. A relative hyperopic shift was observed in all three groups, which was steeper and in long and short eyes compared to normal eyes. Ⅰn fact, refraction changes indicated more peripheral hyperopia with an increase in eccentricity in participants with AL values outside the normal range. Ⅰn the normal AL group, the profile of refractive error showed less change, presenting a rather flat with a slight relative hyperopia beyond 20˚ eccentricity in the temporal field. Ⅰn the long AL group, as expected, the profile of refractive error changes showed more relative hyperopia with increased eccentricity; these changes could be detected in both the temporal and nasal fields. The results of this study showed that the pattern of refractive changes was much more prominent in short (<22.5 mm) and long (>24.5 mm) AL groups compared to the normal AL group.
No marked differences were observed in peripheral refraction (except more than 20˚ eccentricity) in low and normal ACD groups. However, refraction changed considerably with an increase in eccentricity in the high ACD group compared to the two other groups, indicating a correlation between ACD changes and peripheral refraction changes. According to the results of this study, the pattern of peripheral refractive changes was much more noticeable in the high ACD group versus the normal ACD group and in the normal ACD group compared to the low ACD group.
Ⅰn this study, a temporal-nasal asymmetry was seen in all AL and ACD groups which was more prominent beyond 20˚ eccentricity. This finding was consistent with the results of other studies[26-27]and indicated that the temporal-nasal asymmetry was not associated with central refractive error[26]. According to previous studies, this asymmetry is mainly driven by differences in J0 astigmatism since significantly more astigmatism is measured in the temporal retinal versus the nasal retina. One possible explanation for J0 astigmatism difference is alpha angle, which occurs because the fovea is slightly displaced temporally compared to the pupillary axis[26].The limitations of this study included its small sample size, not evaluating hyperopic cases, and not assessing other ocular biometric parameters and corneal topography in the samples. Since variation in the quality of the images formed on the retinal periphery causes different patterns of peripheral refractive errors and ocular growth and because off-axis refraction is affected by corneal asphericity and geometric shape and optics of all anterior segment parameters, further research is necessary to study these parameters as important determinants of refractive error development. Since previous studies showed a weak correlation between corneal curvature and central refraction[19], it is recommended that the relationship between corneal curvature and peripheral refraction be investigated in future studies.
The results of this study showed that the pattern of refractive changes in long and short eyes were much more prominent that normal AL eyes. Moreover, the pattern of peripheral refractive changes was much more prominent in the high ACD group versus the normal ACD group and in the normal ACD group compared to the low ACD group.
ACKNOWLEDGEMENTS
Conflicts of Interest: Khorrami-Nejad M,None;Moradi R,None;Akbarzadeh Baghban A,None;Khosravi B,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
