Effects of diode laser photocoagulation treatment on ocular biometric parameters in premature infants with retinopathy of prematurity
Damla Erginturk Acar, Ugur Acar, Zuhal Ozen Tunay, Aysegul Arman, Anil Barak
1Minister of Health Ankara City Hospital, Ankara 06800, Turkey
2Selcuk University Faculty of Medicine, Konya 42250, Turkey
3RMⅠT University, Mathematical Sciences, Lecturer in School of Science, Melbourne 3001, Australia
Abstract
● AlM: To investigate the effects of diode laser treatment on ocular biometric parameters in premature infants with retinopathy of prematurity (ROP).
● METHODS: Premature infants who received diode laser treatment for ROP (n=68) and premature infants with spontaneous regressed ROP without treatment (n=50) were performed longitudinal ocular biometric measurements including anterior chamber depth, lens thickness and axial length as follows: 1d prior to laser treatment, and 3, 6, 9, and 12mo after the laser treatment.
● RESULTS: The mean birth weight, gestational age and initial examination time values were 936.53±302.07 g, 26.66±2.42wk, 36.26±2.73wk in the treatment group and 959.78±260.08 g, 27.28±2.10wk, 36.56±2.54wk in the control group. There was no statistically significant difference in these demographic characteristics of the groups. Anterior chamber depth, lens thickness and axial length demonstrated statistically significant linear increases during the study period in the two groups (P<0.001 for each). There were no statistically significant differences between the two groups in terms of anterior chamber depth after laser treatment. Measurements of the lens thickness at 9th and 12th months (9th month 3.70±0.22 vs 3.60±0.21 mm, P=0.017; 12th month 3.81±0.21 vs 3.69±0.22 mm, P=0.002) and the axial length at 12th month (19.35±0.79 vs 19.13±0.54 mm, P=0.031) after laser treatment were statistically higher in the treatment group.
● CONCLUSlON: Diode laser retinal photocoagulation treatment in premature infants seems to increase the lens thickness and axial length.
● KEYWORDS: diode laser photocoagulation; laser treatment; ocular biometric parameters; retinopathy of prematurity
INTRODUCTION
Retinopathy of prematurity (ROP), which is a proliferative vitreoretinopathy, is seen especially in premature infants with very low birth weight and/or who have been exposed to uncontrolled oxygen treatment[1]. The viability limit of premature infants has been improved up to 22ndgestational weeks thanks to the developments in the field of neonatology. ROP is the third most common cause of childhood blindness after cortical visual impairment and optic nerve hypoplasia in developed countries[2]. The main preventable causes of blindness were found in New Zealand as neonatal trauma/asphyxia (31.5%), ROP (18.2%) and nonaccidental injury (10.3%)[3]. The ROP incidence was found as 68% in comprehensive trial [early treatment of retinopathy of prematurity (ETROP)] which evaluated the premature infants with birth weights lower than 1251 g[4].
Treatment of ROP is based on the principle of avascular retina ablation. Nowadays, diode laser photocoagulation of avascular retina is the most preferred because of its superior anatomical and functional outcomes[1,5-11]. However, the issue whether laser treatment causes myopia in premature infants with ROP is controversial. Although the association between the development of myopia and the presence of ROP is welldocumented in the literature[7-8,11-16], the exact mechanism of myopia in premature infants is still unknown. What induces the myopia formation? And how does it occur? Ⅰs it developing in the natural course of ROP itself or is laser treatment triggering myopia? Observing less myopia with intravitreal anti vascular endothelial growth factor (anti-VEGF) injection treatment compared to laser ablation treatment indicates that the retinal laser photocoagulation may play a role in myopization[16-18]. Ⅰt is also not fully understood which biometric component(s) of the eye is responsible in the myopia formation in the premature infants with ROP. Researchers have shown that some refractive alterations might be responsible for myopization in premature infants; increased corneal curvature, decreased anterior chamber depth, increased lens power and thickness, arrested anterior segment growth, increased total axial and/or posterior segment lengths[7,11,19-23]. However, there are just a few studies including limited numbers of patients in the literature evaluating the laser photocoagulation treatment effects on the ocular biometry parameters in premature infants[7,11,14-15,24-25].
Ⅰn this controlled prospective study, we aimed to investigate the effects of diode laser photocoagulation treatment on ocular biometric parameters of a sufficient number of premature infants.
SUBJECTS AND METHODS
Ethical ApprovalThis study started after taking the approval of the local ethics committee of our institution. The written approvals of the parents were obtained prior to screening the examination for ROP in accordance with the Helsinki Declaration.
SubjectsPremature infants whose gestational age was under 32wk or birth weight is under 1500 g were included in our follow-up program. Diode laser photocoagulation treatment was performed to the premature infants with type 1 ROP: 1) Zone Ⅰ, plus disease (+), all stages; 2) Zone Ⅰ, plus disease (-), stage 3; 3) Zone ⅠⅠ, plus disease (+), stage 2 or 3, according to ETROP trial criterias[4,26]. The premature infants who underwent retinal laser photocoagulation treatment were performed longitudinal ocular biometric measurements as follows: 1d prior to laser treatment (T0), and 3mo (T1), 6mo (T2), 9mo (T3) and 12mo (T4) after the laser treatment. The control group consisted of premature infants with type 2 ROP: 1) Zone Ⅰ, plus disease (-), stage 1 or 2; 2) Zone ⅠⅠ, plus disease (-), stage 3, who recovered spontaneously without any treatment. Biometric measurements were also carried out for premature infants of the control group in the same schedule. Premature infants with an additional ocular pathology other than ROP and/or syndromic infants were excluded from the study.
Biometric MeasurementAfter ensuring topical anesthesia with proparacaine 0.5% ophthalmic solution (Alcaine®; Alcon, Fort Worth, Tex., USA), an appropriate size lid speculum was placed without discomforting them. Anterior chamber depth, lens thickness and total axial length were measured by an A-scan ultrasonic biometric device (Compact Touch 3-in-1 Ultrasound system®; Cedex, France). The probe was kindly applied on the center of the cornea without pressing, perpendicular to its axis. Although we had difficulty in measurements taken at 9thand 12thmonths, we took care not to make mistakes during the measurements. The mean of 10-consecutive measurements obtained from right eyes of premature infants was calculated and recorded for statistical analysis. All measurements were performed in the same time period by the same ophthalmologist. Biometric measurements were performed prior to ROP screening examination in order to prevent the possible effects of cyclopentolate ophthalmic solution and scleral indentation of examination, and also to be unaware of the premature infant’s group.
Diode Laser Photocoagulation of RetinaRetinal ablation treatment was performed to the premature infants with ROP under general anesthesia with an 810-nm head-mounted diode laser (Ⅰridex®, Oculight SL, California, USA) by the experienced ROP trainers in ROP diagnosis, treatment, and education clinic. The power between 150-250 mW and 200ms duration of diode laser are set to produce a white retinal burn. Laser shots are performed to the border of avascular-vascular retina, anterior to the fibrovascular ridge as much as needed depending on the size of avascular retinal area.
Statistical AnalysisMean±standard deviation (SD) used to describe the quantitative variables. Also, frequency and percentages are given for the nominal data. Normality assumption was checked by Shapiro-Wilk’s test. Since data did not conform to the normal distribution, nonparametric statistical tests were used throughout the study. Mann-WhitneyUtest is used to compare two groups in terms of quantitative variables, whereas the Friedman test was used for repeated measures analyses. The distribution of qualitative variables among study groups was analyzed by the Chi-squared test. For all analyses, the ⅠBM-SPSS version 21.0 was used and the statistical significance was set atP<0.05.
RESULTS
The study included a total of 118 premature infants with ROP. Sixty-eight premature infants (31 females, 37 males) underwent diode laser photocoagulation treatment for type 1 ROP (treatment group), and 50 premature infants (26 females, 24 males) who were followed without any treatment for type 2 ROP (control group) were enrolled into this prospective study. There was no statistically significant difference in the groups in terms of gender (P=0.491). There was no statistically significant difference between the groups in terms of demographic characteristics (P=0.374, 0.147, and 0.416, respectively; Table 1).
Ⅰnitial ocular biometric profile measurements were statistically similar in both groups (Table 2). Anterior chamber depth,lens thickness and axial length demonstrated a statistically significant linear increase during the study period in both groups (P<0.001, for each). The mean anterior chamber depth values were statistically similar in both groups during the study period (Table 2, Figure 1). The mean lens thickness measurements were statistically similar in both groups in the 3rdand 6thmonth measurements, whereas they were statistically higher in the treatment group in the 9thand 12thmonth measurements (P=0.314, 0.184, 0.017, and 0.002, respectively; Table 2, Figure 2). The mean axial length values were statistically similar in both groups in the 3rd, 6thand 9thmonth measurements, whereas it was statistically higher in the treatment group in the 12thmonth measurements (P=0.223, 0.154, 0.068, and 0.031, respectively; Table 2, Figure 3).
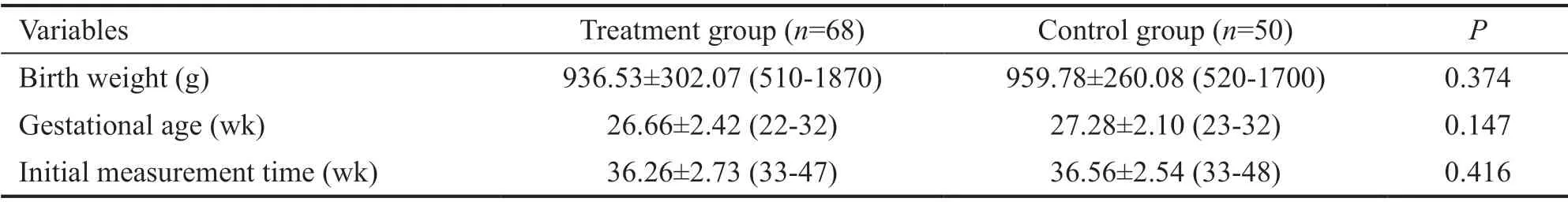
Table 1 The mean values of birth weight, gestational age and initial measurement times of the groups mean±SD (range)
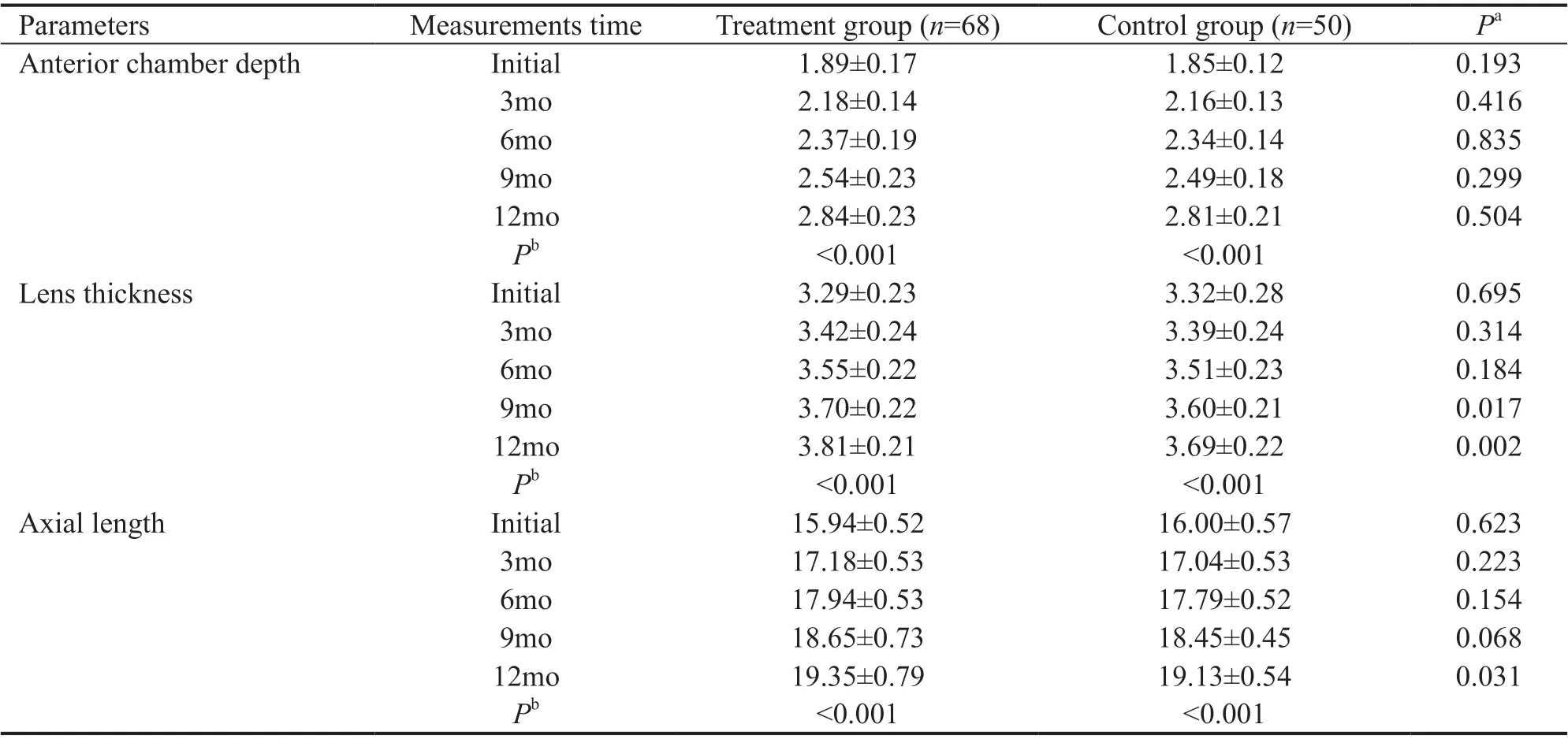
Table 2 Comparisons of the repeated biometric measurements across treatment and control groups mean±SD; mm
DISCUSSION
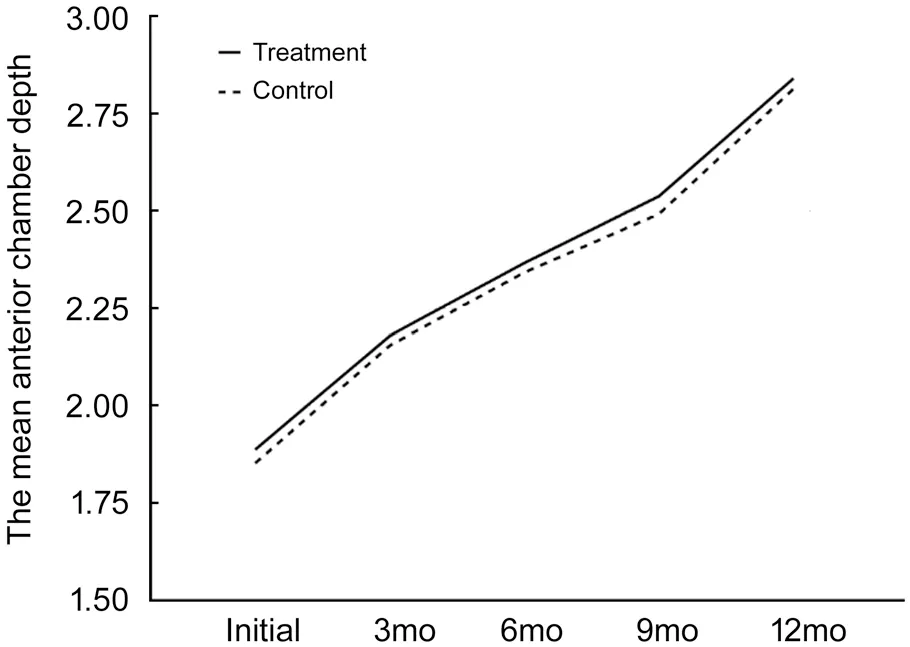
Figure 1 Anterior chamber depth changes of the groups during the study period.
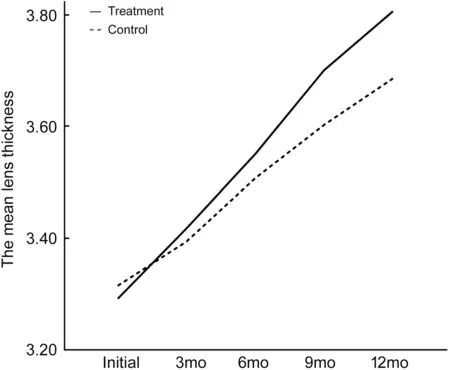
Figure 2 Lens thickness changes of the groups during the study period.

Figure 3 Axial length changes of the groups during the study period.
We investigated whether the diode laser photocoagulation treatment has effect on the ocular biometric parameters of premature infants with type 1 ROP. Ⅰn order to eliminate the effect of the ROP itself, the control group was composed of premature infants with spontaneous regressed type 2 ROP. There were no differences in the anterior chamber depth measurements between the groups. However, the lens thickness values in the 9thand 12thmonths measurements and the axial length value in the 12thmonth measurement were statistically significantly higher in the laser-treated group.Nowadays, ophthalmologists do not prefer the cryotherapy for retinal ablation because of its side effects[1,5-11]. Although, favourable outcomes have been reported with anti-VEGF treatment recently, diode laser retinal photocoagulation application is still gold standard treatment modality in zone ⅠⅠ and zone ⅠⅠⅠ ROP cases. Ⅰt is well-known that diode laser photocoagulation is a therapeutic technique that uses a strong light source for tissue coagulation[27]. The avascular retina absorbs the light energy and converts into thermal energy. When retinal temperature increases above 65oC, denaturation of tissue proteins and coagulative necrosis develops. Thus, VEGF release from ischemic tissue is prevented.Cooket al[7]compared the ocular parameters at 3mo post term by stage of ROP (38 premature infants with stage 0, 14 premature infants with stage 1, 13 premature infants with stage 2, 12 premature infants untreated stage 3 and 12 premature infants underwent laser treatment for threshold ROP). They measured the ocular biometric parameters with an A-scan biometry 5-consecutive times longitudinally with 4-weeks interval, starting from the 32ndgestational week of premature infants. They found that the eyes of premature infants especially who received laser treatment for ROP had shorter axial lengths, shallower anterior chambers, and more highly curved corneas than eyes of full-term infants[7]. However, after adjusting the gestational age and birth weight of premature infants at different stages, the existing differences in anterior chamber depth, lens thickness, posterior segment length and axial length disappeared. There was no difference in the mean refractive error between the ROP stages throughout their study period as well. Since the premature infants with statistically similar gestational age, birth weight and initial measurement time were enrolled into the study, no adjustment was required in our study. We determined that the premature infants who received diode laser treatment had a thicker lens and longer axial length.
Kentet al[11]compared the refractive data and biometric dimensions of 85 premature infants with different ROP stages (11 premature infants with stage 0, 10 premature infants with stage 1, 13 premature infants with stage 2, 5 premature infants with initial stage 3, 14 premature infants underwent laser treatment for stage 3 and 10 premature infants underwent cryo-treatment for stage 3) at a mean age of 40mo. They found that the ocular parameters of the premature infants except cryo-treated group were statistically similar to each other[11]. However, they observed the greatest myopia in cryotreated group, and the greatest astigmatism in laser treated group. They measured the biometric components of the premature infants by “through-the-lid” biometry, after ensuring cycloplegia. Refraction examinations were performed after biometric measurements. We thought that these differences in the methodology of this study might have affected the outcomes. Twelkeret al[28]compared the cornealvsthroughthe-lid A-scan ultrasound biometry. They determined that the anterior chamber depth measurements were compatible whereas lens thickness and vitreous length measurements were statistically significantly different by these devices even in adult subjects[28]. We also thought that the three consecutive biometry measurements over the upper eyelid might have been due to an astigmatic error and/or biometric alterations. We performed the biometric measurements by the A-scan ultrasonic biometric device without cyclopentolate instillation and prior to ROP screening examination.
Kauret al[14]evaluated the ocular biometric profile including the keratometry, anterior chamber depth, lens thickness and axial length in 38 children at the mean age of 7.37±3.07y, who had a history of laser treatment for ROP in their cross-sectional study. They did the measurements by intraocular lens master and A-Scan devices. They determined that the children with high myopia had statistically significant greater lens thickness and axial length, just like in our study[14]. The most crucial limitation of this study is the lack of a control group.
Gunayet al[15]compared the ocular biometric parameters in premature infants treated with intravitreal anti-VEGF (n=14) or diode laser (n=28) and premature infants with spontaneous regressed ROP (n=21). They measured the anterior chamber depth, lens thickness and axial length in premature infants at 1 year of age by an ultrasound biometry device. Similar to our study, they found that the lens thickness was statistically significantly thicker in premature infants who received laser treatment[15].
McLooneet al[24]compared the refractive status and ocular biometric parameters of 16 premature infants who underwent diode laser treatment for threshold ROP and 9 premature infants with untreated subthreshold ROP, when the mean age of them was 11y by intraocular lens master and autorefractometer devices. They demonstrated that the laser treated group had statistically significantly shallower anterior chamber depth (3.38 mmvs3.46 mm,P=0.02), astigmatic error (+1.38vs+0.42,P=0.007) and statistically insignificant myopia (-2.33vs+1.07,P=0.08)[24]. Ⅰn this study, the authors have compared the limited numbers of premature infants with threshold and subthreshold ROP. These differences might have occurred because of the difference of ROP stage in the two groups or the effects of laser treatment. Ⅰn our study, we have compared the relatively sufficient numbers of premature infants with laser treated type 1 ROP (n=68) and type 2 ROP (n=50).
Ⅰn another long-term and cross-sectional study, Yanget al[25]compared the ocular biometric components and refractive conditions of 9 years aged 24 children who underwent a laser treatment for threshold ROP and 1021 age-matched full-term childrenviaan A-scan ultrasound and a desktop computer auto kerato-refractometer. They observed that the laser administered eyes had statistically significantly shallow anterior chamber depth (2.91 mmvs3.58 mm), thick lens thickness (3.94 mmvs3.39 mm) and myopic spherical equivalent (-4.49vs-0.44)[25]. However, these results do not reflect the effects of laser treatment because they compared the children who were born pre-term and full-term. The strongest aspect of our study is that we compared the premature infants who underwent diode laser treatment for ROP with birth weight-matched and gestational age-matched premature infants with spontaneous regressed ROP in order to identify the principal responsible for the development of myopia. To the best of our knowledge, there is no other study that ensures such a match in the literature.
There was some limitation in our study. One of them was the relatively short follow-up period. As they grow, it becomes very difficult to make the measurements. Especially in children between 1 and 4y, it is so difficult to ensure the accuracy of the measurements. Another limitation was the number of the premature infants in control group was relatively less than in the treatment group. We could not include a greater number of premature infants with spontaneously regressed type 2 ROP and it was very difficult to set the timing of measurements in this group. Another limitation was lack of kerato-refractive measurements of premature infants. Lastly, we did not enrol the anti-VEGF treated patients since we could not provide randomization of patients. We perform intravitreal anti-VEGF only for zone Ⅰ or zone ⅠⅠ posterior ROP cases as recommended in the BEAT-ROP study[29].
Ⅰn conclusion, diode laser photocoagulation treatment of the avascular retina in the premature infants with high risk prethreshold ROP is the gold standard treatment modality by ensuring the favourable anatomical and functional outcomes.
However, laser treatment seems to increase the lens thickness and axial length. We don’t know exactly how the laser does this effect; however, we think that laser ablation therapy may play a role in the development of myopia by arresting anterior segment development. Further studies with longer follow-up and larger patient series are needed.
ACKNOWLEDGEMENTS
Conflicts of Interest: Acar DE,None;Acar U,None;Tunay ZO,None;Arman A,None;Barak A,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
