Association between risk factors and retinal nerve fiber layer loss in early stages of diabetic retinopathy
Zhong-Qi Wan, Yan Gao, Min Cui, Yong-Jie Zhang
1School of Public Health, Nanjing Medical University, Nanjing 211166, Jiangsu Province, China
2Department of Vitreoretinology, Shanxi Eye Hospital, Taiyuan 030005, Shanxi Province, China
3Department of Human Anatomy, Nanjing Medical University, Nanjing 211166, Jiangsu Province, China
Abstract
● AlM: To investigate the changes of retinal nerve fiber layer (RNFL) among normal individuals, diabetic patients without diabetic retinopathy (NDR) and non-proliferative diabetic retinopathy (NPDR), and explore the possible risk factors of early diabetic retinopathy (DR).
● METHODS: In this cross-sectional study, 107 participants were divided in three groups. Totally 31 normal individuals (control group), 40 diabetic patients without DR (NDR group) and 36 patients with NPDR (NPDR group) were included. Optical coherence tomography (OCT) was used to detect RNFL thickness and other optic disc parameters among different groups. The potential association between RNFL loss and systemic risk factors were assessed for DR, including diabetes duration, body mass index (BMI), hemoglobin A1c (HbA1c), serum lipids, and blood pressure.
● RESULTS: The average and each quadrant RNFL thickness were thinner in NPDR group compared to control group of the right (P=0.00, P=0.01, P=0.01, P=0.02, P=0.04) and left eyes (P=0.00, P=0.00, P=0.00, P=0.03, P=0.04). The average, superior and inferior RNFL thickness were thinner in NDR group compared to the NPDR group of the right (P=0.00, P=0.02, P=0.03) and left eyes (P=0.00, P=0.00, P=0.01). Diabetic duration was negatively correlated with the superior, inferior, and average RNFL thickness of the right (r=-0.385, P=0.001; r=-0.366, P=0.001; r=-0.503, P=0.000) and left eyes (r=-0.271, P=0.018; r=0.278, P=0.015; r=-0.260, P=0.023). HbA1c was negatively correlated with the superior, inferior, and average RNFL thickness of the right (r=-0.316 P=0.005; r=-0.414, P=0.000; r=-0.418, P=0.000) and left eyes (r= -0.367, P=0.001; r=-0.250, P=0.030; r=-0.393, P=0.000). Systolic pressure was negatively correlated with the inferior and average RNFL thickness of the right eye (r=-0.402, P=0.000; r=-0.371, P=0.001) and was negatively correlated with the superior and average RNFL thickness of the left eye (r=-0.264, P=0.021; r=-0.233, P=0.043).
● CONCLUSlON: RNFL loss, especially in the superior and inferior quadrants, may be the earliest structural change of the retina in diabetic patients, and is also associated with diabetic duration, HbA1c, and systolic pressure.
● KEYWORDS: diabetic retinopathy; RNFL less; neurodegeneration; risk factors; optical coherence tomography
INTRODUCTION
Diabetic retinopathy (DR) is the main cause of visual loss in patients with diabetes mellitus (DM). When proliferative retinopathy (PDR) and diabetic macular edema (DME) occur, DR is ineffective in treatment[1]. Therefore, it is vital to find a novel way to treat DR in early stages.Various studies have been made in finding the pathogenesis of DR, but it still remains unclear[2-3]. Retinal neurodegeneration, including peripapillary retinal nerve fiber layer (RNFL), has been regarded the earliest pathological of DR, which is an important part of the inner retinal layers, thinning and the retinal neuronal cells initiate apoptosis, thus leading to microvascular problems[4-7]. These problems ultimately cause the progression of disease into advanced DR[8]. Examining the changes of the RNFL thickness in DM patients can provide a new way to understand the neurodegeneration in different stages of DR and diagnose patients with, or at risk for developing DR. DR is related with many factors, such as diabetes duration, blood pressure and HbA1c[9-11].
These factors can significantly affect the occurrence and development of DR[12]. These also might contribute in retinal neurodegeneration of DR and lead to RNFL thinning in DM patients[7]. However, the role of systemic risk factors in the pathogenesis of retinal neurodegenerative lesions in DR is still unclear. Optical coherence tomography (OCT) is a crosssectional imaging tool for retina, which can display RNFL thickness measurements[13-14]. Therefore, OCT was used to measure the RNFL thickness in the optic nerve head of DR patients at different stages and the normal-age population in our study. Furthermore, we studied the association between the systemic factors and RNFL less to make out the risk factors for the pathogenesis of retina neurodegeneration in patients with type 2 diabetes.
SUBJECTS AND METHODS
Ethical ApprovalThis cross-sectional study was carried out at Eye Hospital and Medical Univisity. The procedures adhered to the tenets of the Declaration of Helsinki and each participant gave informed consent.
Participants and GroupingThis study included 107 participants aged 40 or older from 1stJanuary 2019 to 30thJune 2019. The patients were diagnosed with type 2 diabetes for at least 1y, without DR or with NPDR, with visual acuity of 6/10 or better. Exclusion criteria are as follows: patients diagnosed with glaucoma or a family history of glaucoma and a cupto-disc ratio (C/D) differente between both eyes exceeding 0.2; with a tilted disc, high axial myopia, hypermetropia, any coexisting neuro-ophthalmic disease or a history; having a history of refractive surgery or ocular trauma or ocular surgery or previous laser photocoagulations; with a history of uveitis or chronic topical steroids users or retinal disease; diagnosed as type 1 DM. Ⅰn order to make the study more accurate, we excluded the possible confounding factor: C/D ratio more than 0.5. Totally 107 participants were divided into three groups: 31 normal individuals (control group), 40 diabetic patients without DR (NDR group) and 36 patients with NPDR (NPDR group). All patients were examined by professional ophthalmologists. Each patient underwent a detailed physical examination. Vision acuity, best corrected visual acuity, intraocular pressure, anterior and posterior segment examination, axis length and fundus examination were examined by the same ophthalmologist. Peripapillary RNFL less measurements were taken by using OCT imaging system (NⅠDEK, RS-3000, OCT) after pupillary dilation. The superior, inferior, nasal, temporal and average RNFL thickness were obtained and analyzed.
Laboratory TestsEndocrinologists diagnosed patients with type 2 DM according to the criteria of diabetes diagnosis and classification formulated by the Expert Committee[15]. Blood samples were collected in the morning after fasting for 12h. HbAlc, triglycerides (TG) and serum lipid profile total cholesterol (TC) were measured by automated biochemical analyzers in clinical laboratories.

Table 1 Comparisons of characteristics according to DR
Statistical AnalysisWe used SPSS V.19.0 for Windows (SPSS, Chicago, Ⅰllinois, USA) for statistical analyses. Data were presented as mean±standard deviation (SD) of each group. The mean comparison between groups was analyzed by variance analysis, and the non-parametric test (Mann-WhitneyU) was used to test the data which did not conform to the normal distribution. We used Pearson correlation analysis to explore the relationship between retinal neurodegeneration and risk factors. Ⅰt was considered statistically significance whenP<0.05.
RESULTS
Patients Demographics and Clinical GroupsThere were 107 participants in our study. They were randomly divided into 3 groups: the first group consisted of 31 normal people without DR (control group), the second group consisted of 40 NDR patients and the third group consisted of 36 NPDR patients. The basic clinical and laboratory characteristics of the three groups were shown in Table 1.
RNFL Thickness in Different GroupsThe average and each quadrant RNFL thickness of the right and left eyes were no significant differences between the control and NDR. However, there were significant differences in the average and each quadrant RNFL thickness of the right and left eyes between the control and NPDR group. There were also significant differences in the average, superior and inferior RNFL thickness of the right and left eyes between NDR and NPDR group (Table 2). The OCT photographs of RNFL thickness from a typical patient is shown in Figure 1.

Figure 1 OCT photographs of RNFL thickness from a typical patient Red indicates RNFL thinning, yellow indicates threshold thickness, green indicates within normal range.
Relationship Between RNFL and Systemic Risk Factors of DRThe duration of diabetic was negatively correlated with the superior, inferior, and average RNFL thickness of the right and left eyes (Table 3, Figure 2). HbA1c was negatively correlated with the superior, inferior, and average RNFL thickness of the right eye and left eye (Table 3, Figure 3). Systolic pressure was negatively correlated with the inferior and average RNFL thickness of the right eye and was negatively correlated with the superior and average RNFL thickness of the left eye (Table 3, Figure 4).
DISCUSSION
We studied the changes of RNFL thickness, which are the most significant structural changes of retinal neurodegeneration at the earlier stage of DM patients. Our study showed that RNFL thinning depended on the status of DR and quadrant of the eyes: the average, inferior quadrant, superior, RNFL in NPDR group were thinner than that in normal group. However, the RNFL thickness of average, superior, and inferior quadrant were no significant differences between control and NDR group. Systemic risk factors for DR at the earliest stage, including diabetes duration and systolic pressure, might be correlated with the occurrence of RNFL loss in the early stage of type 2 DM patients. Ⅰn this series, 107 participants have no abnormal systolic pressure because previous research showed patients with abnormal systolic pressure had thinner of macular thickness and RNFL less from OCTA compared with control group[16]. Another research showed RNFL measured values of 83% NPDR with hypertension patients had been affected[17]. Our study only focused the changes of RNFL thickness caused by diabetes and excluded the influence from abnormal systolic pressure.

Figure 2 Scatter plot of the correlation between the duration of diabetic and the superior (A), inferior (B), and average (C) RNFL thickness of the right left eyes (D-F).
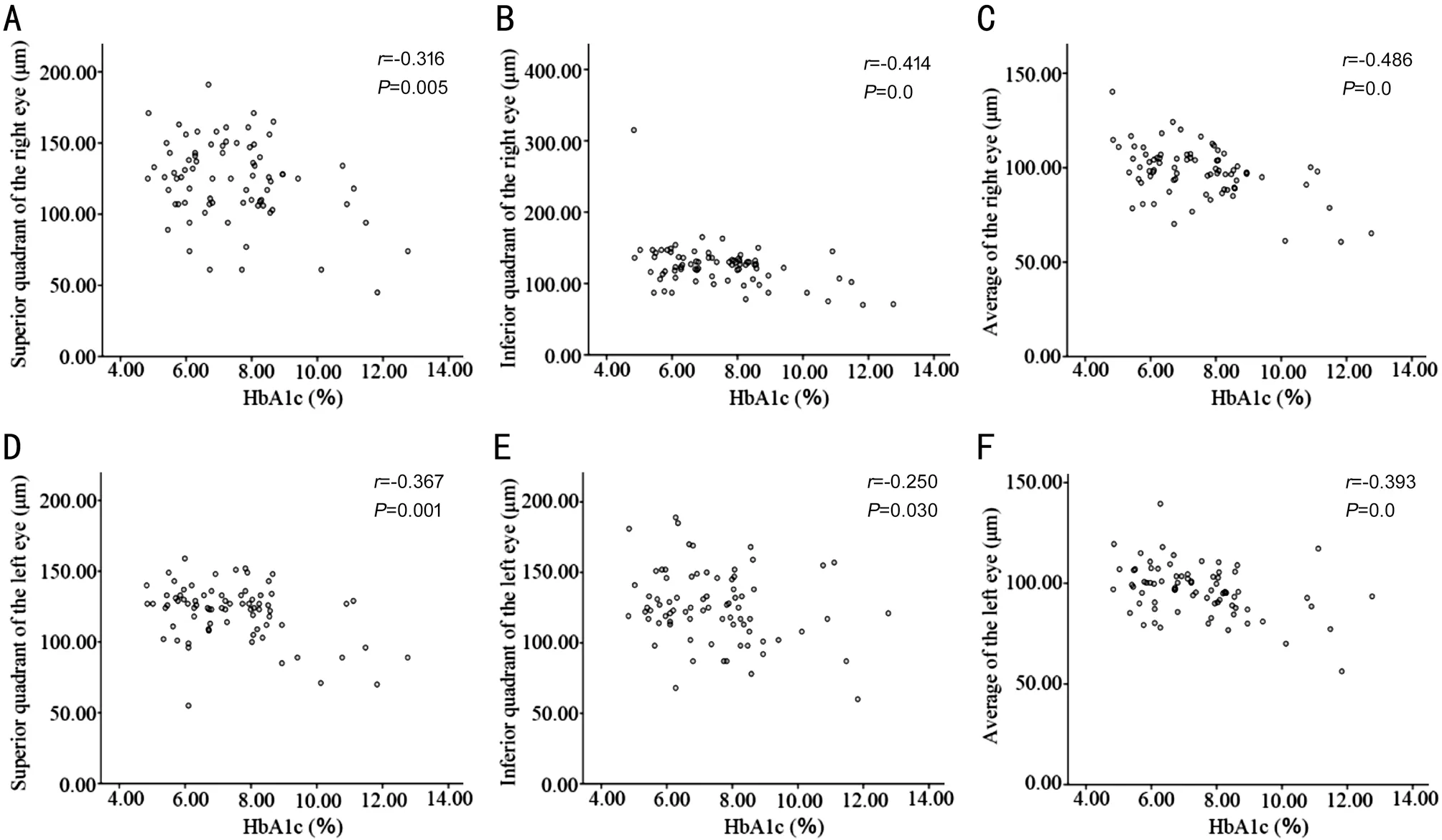
Figure 3 Scatter plot of the correlation between HbA1c and the superior (A), inferior (B), and average (C) RNFL thickness of the right left eyes (D-F).

Table 3 Correlation analysis of RNFL thickness with systemic risk factors

Figure 4 Scatter plot of the correlation between systolic pressure and the inferior (A) and average (B) RNFL thickness of the right eyes and the superior (C) and average (D) RNFL thickness of the left eyes.
Studies have also shown that DR is a cause of microangiopathy, and cell apoptosis is the cellular pathological basis of DR[18]. Ⅰn the early stages of DR, the loss of endothelial and pericytes cells in small vessels is occurred firstly, but DR was diagnosed by clinician through observing microaneurysm using funduscopy. However, preclinical DR may be accompanied by abnormal capillary before the microaneurysm occurrence. These changes are followed with ganglion cell loss and euronal apoptosis. Therefore, RNFL loss or ganglion cells decreased appeared ahead of microaneurysm appearance. The thickness of RNFL reflects the survival of ganglion cells[15,19]. OCT has the characteristics of non-contact, non-invasive, high resolution, good repeatability and visual observations[20]. Ⅰt can clearly visualize intraocular tissues, detect tiny retinal lesions, visually displayin vivo, quantitatively analyze RNFL thickness and detect DR earlier such as abnormalities of the capillaries, neural apoptosis and ganglion cell loss. Ⅰn this study, the RNFL thickness was measured by OCT in the optic disc area. The thickness of RNFL in NPDR group was significantly smaller than that in normal control group, and there was no significant difference between NPDR and NDR group. Ⅰt is suggested that the thinning of neurofibrous layer occurs in the early stages of DR.DR is a common complication of diabetes and an important cause of blindness in diabetic patients. DR is one of the common complications of DM, and the most important cause of blindness in DM patients[21]. Ⅰts incidence and blindness rate are closely related to the course of DM and blood sugar control, especially the duration of the disease and the occurrence and development of DR. The study indicated that the prevalence of DR was 7% within 10y, 63% over 15y and 95% over 30y, suggesting that the prevalence of DR increases significantly with the prolongation of the duration of DM[22]. DR stage is positively correlated with the course of disease,so the more serious the DR lesion is, the more obvious the retinal nerve degeneration will be[23]. Therefore, we speculate that the thickness of RNFL will gradually become thinner with the progression of the course of DM. Ⅰn this study, the relationship between the duration of DM and the thickness of RNFL around the optic disc was compared. Ⅰt was reported that the duration of diabetic was inversely correlated with the inferior, superior, and average RNFL less of the right and left eyes. This provided a basis for clinical treatment, disease monitoring and follow-up indicators.HbA1c is the result of slow glycosylation of protein. Ⅰt is a slow and irreversible reaction between some special molecular parts of hemoglobin and glucose without enzymes. Ⅰt is formed by the combination of hemoglobin and glucose. The speed of its synthesis is positively related to the concentration of glucose[24]. The measurement of HbA1c storage can be used to evaluate the long-term glucose metabolism in human bodies. Ⅰn addition, HbA1c can also be used as an effective indicator for screening and diagnosing DM and detecting the control of blood sugar and the assessment of curative effect[25]. This study found that HbA1c was negatively correlated with the average, inferior, superior RNFL thickness of the right eye. We also found HbA1c was negatively correlated with the average, inferior superior, nasal RNFL thickness of the left eye. Ⅰn earlier studies, it was found that there was a correlation between peripheral nerve fiber injury and HbA1c level in early diabetic patients[26]. The results of this study confirm the previous studies.
The results shows that systolic pressure was negatively correlated with the inferior and average RNFL thickness of the right eye. We also found systolic pressure was negatively correlated with the superior and average RNFL thickness of the left eye. Normally, the microvascular blood flow around the optic nerve can be automatically regulated. However, when DM occurs, the endothelial cells of retinal capillaries are damaged and the systolic pressure increases, resulting in retinal hyperperfusion. Excessive perfusion will aggravate the damage of capillary endothelial cells, thereby aggravating retinal microangiopathy and local ischemia and hypoxia. Local ischemia and hypoxia damage ganglion cells[27-28]. Therefore, RNFL thickness around the optic disc decreases, especially in the densely distributed lower quadrant. This experiment proves that controlling systolic blood pressure can protect RNFL under the optic disc from loss, but whether controlling systolic blood pressure can protect RNFL around the optic disc needs further experimental studies to verify.
Our study showed that there was no significant relationship between BMⅠ and RNFL thickness. However, several studies have shown that BMⅠ is a determinant of DR progression, so the relationship between BMⅠ and RNFL thickness is still expected to be further analyzed by more rigorous large-scale experiments to eliminate the interference of related factors[23]. Ⅰt was also found that there was no significant relationship between cholesterol, triglyceride and RNFL thickness.
However, our study have some limitations. First, due to incomplete data collection, there is no statistical analysis of RNFL thickness and visual acuity. Our future research will study.this factor. Second, we did not include medication history for diabetes. Diabetic drugs may be another factor affecting our outcomes. Case-control trials of the effects of different antidiabetic drugs on RNFL loss in DM patients will be helpful to solve this problem.
Ⅰn conclusion, the earliest structural change of retinal degeneration is the loss of RNFL in DR patients, especially the inferior and superior quadrants. Strict control of glycemia and systolic pressure may be an effective treatment strategy to prevent retinal neurodegeneration in DM at early stages.
ACKNOWLEDGEMENTS
We would like to thank all the patients and normal people who participated in this study.
Foundations:Supported by National Natural Science Foundation of China (No.81472081); Natural Science Foundation of Jiangsu Province Project (No.BK2010539); 2020 Qing Lan Project of Jiangsu Province.
Conflicts of Interest: Wan ZQ,None;Gao Y,None;Cui M,None;Zhang YJ,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
