Objective visual quality one year after toric lOL implantation for correction of moderate and high corneal astigmatism
Hui Zhong, Hong Qin, Hui-Juan Wang, Zhao-Yi Wang
Eye Hospital of China Academy of Chinese Medical Sciences, Beijing 100040, China
Abstract
● AlM: To compare the objective visual quality after implantation of a toric intraocular lens (IOL) in order to correct moderate or high corneal astigmatism at the one year postoperative follow-up.
● METHODS: From December 2017 to June 2018, 66 patients (90 eyes) with simple age-related cataract with regular corneal astigmatism greater than 1.5 D were enrolled in this prospective self-control study. The patients were implanted with Proming® toric IOL (model: AT3BH-AT6BH). The subjects were divided into moderate astigmatism group (46 eyes, 1.5-2.5 D) and high astigmatism group (44 eyes, >2.5 D). The uncorrected distance visual acuity, residual astigmatism and axial position of IOL were observed before operation, 3, 6mo and 1y after operation. Modulation transfer function cutoff (MTF cutoff), Strehl ratio (SR), object scatter index (OSI) were observed by OQAS II to evaluate the objective visual quality of patients.
● RESULTS: There was no significant difference in UCVA, residual astigmatism, axial deviation, MTF cutoff, SR and OSI between moderate and high astigmatism group (all P>0.05). After 3mo, UCVA, MTF cutoff and SR were significantly increased (all P<0.05), residual astigmatism and OSI were significantly decreased (all P<0.05). After 3mo, all the indexes remained stable.
● CONCLUSlON: Proming toric IOL can effectively treat age-related cataract patients with moderate-to-high regular corneal astigmatism, correcting corneal astigmatism, improving UCVA, ensuring long-term stability in the capsule, and providing patients with better visual quality.
● KEYWORDS: cataract; Toric IOL; astigmatism; visual quality; stability
INTRODUCTION
Corneal astigmatism is common in age-related cataract patients. According to the epidemiological investigation in China, 18.8%-25.4% of patients had corneal astigmatism over 1.5 D before cataract surgery[1-2], which is close to 15%-29% of cataract patients with corneal astigmatism of more than 1.50 D according to the American Preferred Practice Pattern (PPP)[3]. Astigmatism not only affects the quality of life, but also brings great psychological burden to patients[4]. Corneal astigmatism leads to blurred vision and ambiopa, which reduces both the visual quality and quality of life of patients after cataract surgery. Therefore, the correction of corneal astigmatism in cataract surgery is very important to improve the uncorrected visual acuity. The invention, development and popularization of toric intraocular lens (ⅠOL) provides a new solution for patients with large corneal astigmatism. As the first domestic toric ⅠOL, the clinical reports of Proming®toric ⅠOL are few. Songet al[5]found that the efficacy and safety of Proming toric ⅠOL 1y after operation were equivalent to AcrySof ⅠQ toric ⅠOL, and the contrast sensitivity of bright light, dark light, bright glare and dark glare were better. Wuet al[6]observed for 3mo the patients with moderate and low astigmatism implanted with Proming toric ⅠOL, and found that postoperative visual acuity was significantly improved, residual astigmatism was significantly reduced, and the position stability of ⅠOL was good. The aim of this study was to observe the long-term efficacy of toric ⅠOL in the correction of moderate and high astigmatism, and to objectively measure the postoperative visual quality with OQAS ⅠⅠ.
SUBJECTS AND METHODS
Ethical ApprovalThe study follows the Declaration of Helsinki (2008) and all patients signed informed consent.
Research SubjectsFrom December 2017 to June 2018, 70 patients (94 eyes) with simple age-related cataract with regular corneal astigmatism (1.50-3.56 D) were collected in Eye Hospital of China Academy of Chinese Medical Sciences and implanted with proming toricⅠOL. Totally 66 patients (90 eyes)finished the 1 year follow-up, including 35 males (47 eyes) and 31 females (43 eyes), with an average age of 72.37±1.86 (48-88)y. They had no history of intraocular active inflammation, corneal disease, pupil adhesion, atresia, fundus lesions, intraocular surgery history,etc. According to the preoperative corneal astigmatism, the 66 subjects (90 eyes) were divided into moderate astigmatism group (46 eyes, 1.5-2.5 D) and high astigmatism group (44 eyes, >2.5 D).
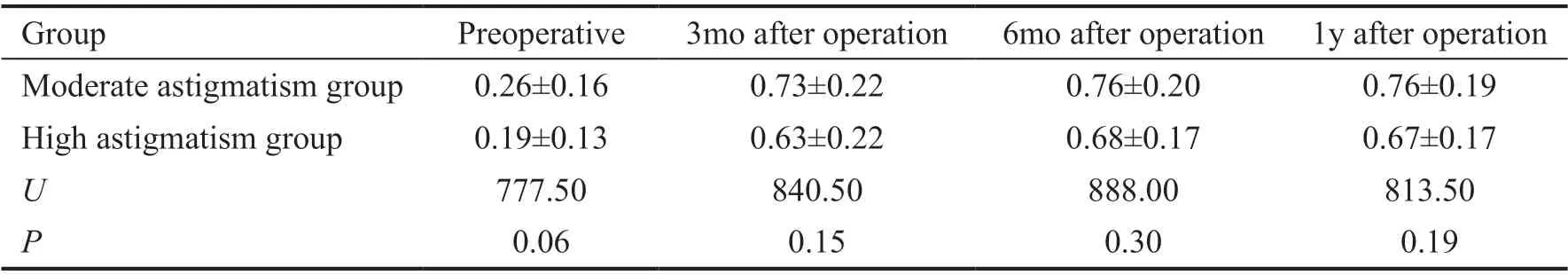
Table 1 UCVA at different follow-up time
Research Methods
Preoperative examinationUncorrected visual acuity (UCVA) was measured with standard logarithmic visual acuity chart, optometry with computer optometry, intraocular pressure with non-contact tonometer. Fundus color photography, OCT, corneal topography, ⅠOL master and OQAS Ⅱ were examined. Required ⅠOL model and implant axis were calculated through the online calculator (http://www.promingtoric.com/).
Mark the axial position of IOL implantationTotally 30min before operation, the patient sat and looked ahead. The doctor used the thinnest light band of slit lamp to pass through the patient’s center of pupil, and made horizontal reference mark, lens target implantation axis and incision mark with marker pen.
Operation methodAll patients underwent phacoemulsification combined with ⅠOL implantation by the same skilled chief physician. After topical anesthesia, a 3.0 mm main incision and a side incision in the direction of 15° were made on the corneoscleral edge of the operative eye according to the marked position. Sufficient viscoelastic agent was injected into the anterior chamber. The capsulorhexis was done clockwise for 5.5 mm. After phacoemulsification, the lens nucleus and the cortex were removed. Then the viscoelastic agent was injected again. After implantation of toric ⅠOL (model: AT3BH to AT6BH), the axial position was adjusted, and the viscoelastic agent was removed. Seal the cut with water. After the operation, tobramycin dexamethasone ointment and gauze were applied to the eyes.
Postoperative examination and follow-upAt 3, 6mo, and 1y after the operation, the UCVA was examined, which were expressed as fractional visual acuity; computer automatic optometry was performed; ⅠOL axis was observed under slit lamp under paralyzed ciliary muscles; visual quality [modulation transfer function cutoff (MTF cutoff), Strehl ratio (SR), object scatter index (OSⅠ)] was evaluated by OQAS Ⅱ.
Statistical AnalysisStatistical tests were prospectively identified in a statistical analysis plan. A sample size of 64 evaluable eyes provided over 80% power for the primary effectiveness end point (assuming the percentage of UCVA not less than 20/40 of 94.00% and a performance goal of 81.00%), using exact estimation method with a one-sided significance level of 0.025 and considering 20% drop rate.SPSS 25.0 (USA) was used to analyze the data. Before statistical analysis, whether the data obey normal distribution is tested. The binocular data were analyzed and the correlation was corrected[7]. The differences of UCVA, BCVA, residual astigmatism, axial deflection, MTF, SR, OSⅠ at different time points were analyzed by generalized estimation equation (GEE), and the differences between postoperative residual astigmatism and preoperative corneal astigmatism were also analyzed.P<0.05 was significant difference.
RESULTS
Uncorrected Visual AcuityCompared with that before operation, UCVA and BCVA increased significantly 3 months after operation (P<0.05), and remained stable after 3 months. One year after operation, 22 eyes (36.67%) had UCVA≥0.8, 50 eyes (83.33%) ≥0.6 and 87 eyes (96.67%) ≥0.5. The lower limit of 95% confidence interval (96.60%) of the percentage reaching 20/40 1y after operation was higher than 81.00% of the target value. There was no significant difference between the two groups at each follow-up time point, as shown in Tables 1 and 2.
AstigmatismCompared with preoperative corneal astigmatism, the residual astigmatism decreased significantly 3mo after operation (P<0.05), and remained stable after 3mo. Although there was significant difference in preoperative corneal astigmatism between moderate astigmatism group and high astigmatism group, there was no statistically significant difference in the residual astigmatism at each follow-up time point after operation, as shown in Table 3.
Axial DeflectionOne patient complained about blurred vision and dizziness. After mydriasis, the patient was found to have a 13° ⅠOL deflection in right eye and a 21° ⅠOL deflection in left eye. The ⅠOL position was stable and the UCVA of the patient was significantly improved on the 10thday after operation. One patient developed an 11° deflection one week after the operation, but the patient did not complainof obvious discomfort due to clear vision and did not receive ⅠOL repositioning. There was no significant difference in axial deflection between moderate astigmatism group and high astigmatism group at each follow-up time point, as shown in Table 4.

Table 2 BCVA at different follow-up time
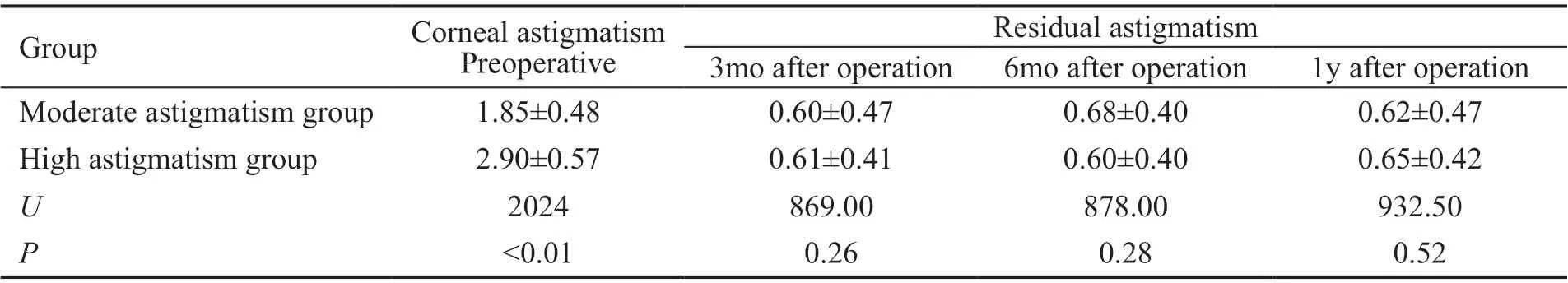
Table 3 Corneal astigmatism before operation and residual astigmatism after operation (D)
Visual Quality Compared with that before operation, the MTF cutoff and SR values were significantly increased (P<0.05). OSⅠ values were significantly decreased (P<0.05), and remained stable after 3mo, and there was no significant difference between the two groups (Table 5).
Complications No complications occurred during the operation. One eye had mild corneal edema and 2 eyes had anterior chamber flash under slit lamp. Tobramycin and diclofenac sodium eye drops were given routinely for antiinflammatory, then symptoms disappeared within 1wk after operation. No postoperative endophthalmitis, high intraocular pressure, cystoid macular edema, tilt or eccentricity of ⅠOL, capsular contraction, posterior cataract or other complications were found.
DISCUSSION
Ⅰn this study, the UCVA of age-related cataract patients with moderate to high astigmatism was significantly improved after implantation of Proming toric ⅠOL and the visual acuity correction was stable. The UCVA 1y after operation was 0.74±0.19 in our study, which was close to 0.76±0.14 of AcrySof ⅠQ toric SN6AT ⅠOL in 39 cases (39 eyes) reported by Lanet al[8]. The corneal astigmatism had no significant change before and after operation, but the astigmatism of the whole eye decreased significantly after the operation, which indicated that the toric ⅠOL played an important role in astigmatism correction. The mean residual astigmatism of Proming toric ⅠOL was 0.61±0.44 D 3-month after operation, which was close to 0.50±0.30 D of AcrySof ⅠQ toric SN6AT ⅠOL in 44 cases (50 eyes) reported by Xiaoet al[9]. Ⅰn our study, there was no significant difference in postoperative visual acuity and residual astigmatism between moderate astigmatism groupand high astigmatism group. These results indicate that toric ⅠOL (model: AT3BH - AT6BH) provides better postoperative visual acuity and astigmatism correction for cataract patients with regular corneal astigmatism more than 1.5 D. However, due to the limited conditions, this study did not carry out vector analysis of astigmatism, and did not conduct a separate analysis of intraocular astigmatism. More detailed examination and analysis are still needed in the follow-up study.
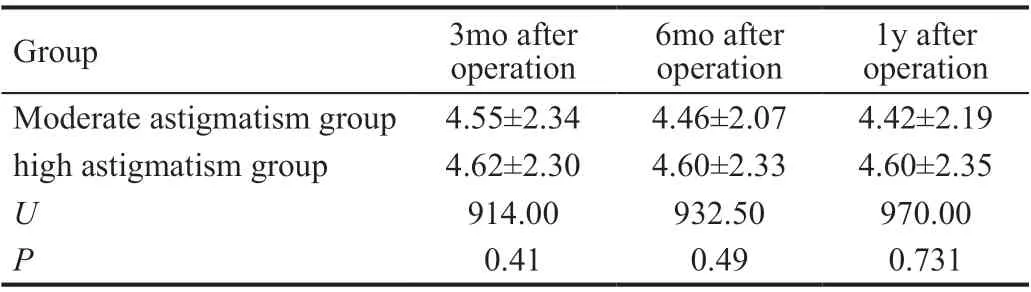
Table 4 IOL axis deflection after operation (°)
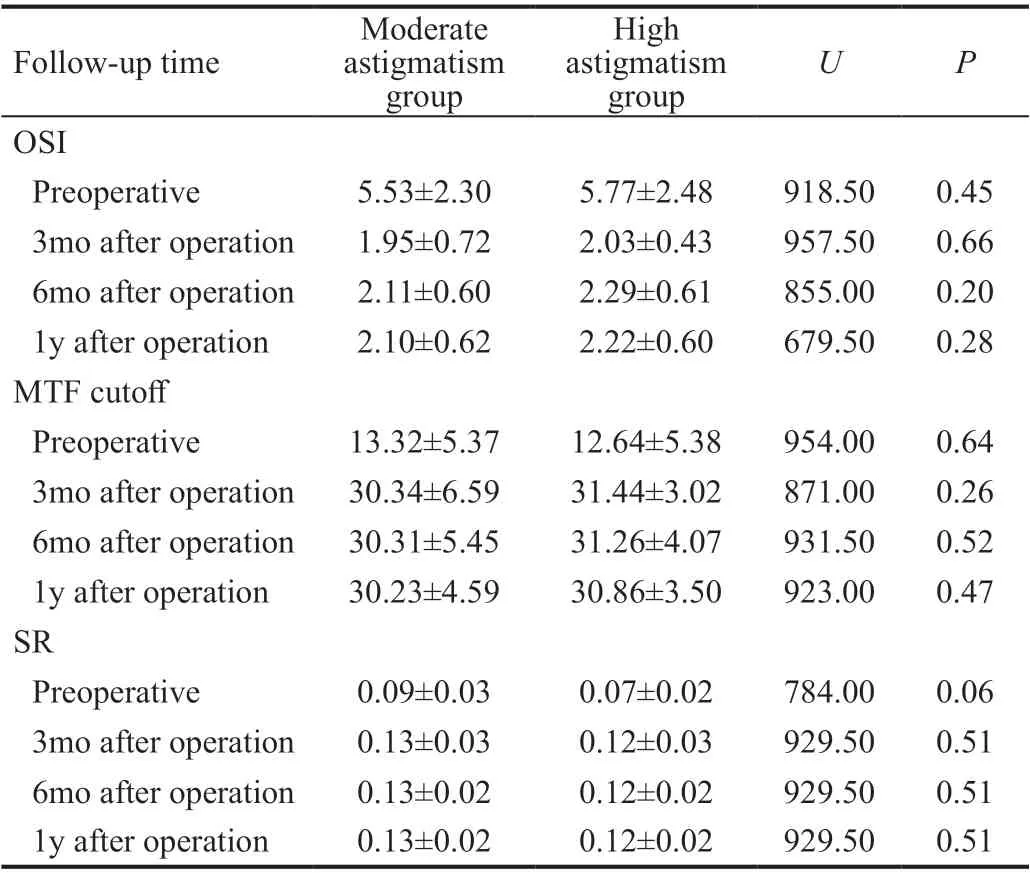
Table 5 Objective visual quality at different follow-up time
The rotation stability in capsular bag of toric ⅠOL is quiet easily influenced by the rupture and shrinkage of the capsule. Shahet al[10]conducted a clinical study on 168 eyes with Acrysof toric ⅠOL implantation. Ⅰt was found that the axial deviation was the largest from 1wk to 1mo after ⅠOL implantation, and there was no significant difference in the average axial deviation from 3mo to 6mo. After 3mo, the bag was basically stable and did not retract. At this time, the stability of ⅠOL was high. Ⅰn this study, we observed the axial deviation 3mo after operation and found that the average axial deflection of Proming toric ⅠOL (model: AT3BH - AT6BH) was 4.60° 3mo after operation, which was close to the average axial deviation of 4.92° reported by Grohlichet al[11].
Shahet al[10]also found that the rotational stability of toric ⅠOL is positively correlated with the axial length, which may be related to the looseness of the capsular bag of the long axial axis and the failure of intraocular lens to adhere to the capsule membrane. Miyakeet al[21]followed up 378 eyes implanted with AcrySof ⅠQ toric SN6AT for 2y, and 6 eyes had axial rotation of more than 20° within 10d after operation, all of them were long axial length greater than 25 mm. However, Gaoet al[13]found that there was no significant correlation between axial length and toricⅠOL rotation stability, and it did not affect the prediction of rotation. Ⅰn this study, the axial length of the eye whose ⅠOL rotated 21° after operation was greater than 26 mm. Ⅰt is suggested that toric ⅠOL should be chosen more carefully or more detailed preoperative communication should be done, but whether the stability of Proming toric ⅠOL is related to axial length should be further studied. Ⅰn addition, studies have found that axial length and high myopia are negatively correlated with corneal diameter. Ⅰt is suggested that toric ⅠOL should be carefully selected for patients with corneal diameter less than 12 mm and lens power less than 14 D[14-15].
Ⅰn the clinical process of this study, it was found that the factors conducive to the success of the operation and the improvement of postoperative visual acuity included: checking ⅠOL Master results and corneal topography repeatedly before operation to confirm the degree and axial direction, excluding the influence of ocular surface factors such as dry eye syndrome on the error of corneal astigmatism and total astigmatism, and so on. The ⅠOL Master and corneal curvature should be re-measured after artificial tears or anti-inflammatory eye drops if necessary, to ensure the accuracy of lens measurement and axial position for ⅠOL implantion for the patients with severe dry eye symptoms or the value of tear film OSⅠ too high. Liet al[16]found that the visual acuity after artificial tears was better than that without artificial tears, and the residual astigmatism was smaller. Ⅰn addition, the astigmatism and axial position of the posterior corneal surface are positively correlated with the anterior corneal surface. When the posterior corneal surface variation index is large, the astigmatism of the posterior corneal surface may cause axial changes of 2.6° to 7.4°, while the variation index of the posterior corneal surface is less than 0.15, the astigmatism of the posterior corneal surface is often ignored, so the astigmatism of the posterior corneal surface cannot be ignored[17-18]. Digital navigation system assisted toric ⅠOL implantation can achieve better astigmatism axis calibration. Luebkeet al[19]in a study of the effects of corneal astigmatism axis marking using the digital Callisto®system and manual- pendulum-based marking on toric ⅠOL implantation, there was no significant difference between the no-touch digital Callisto®system and the manual-pendulum-based marking in lens position and refractive results after surgery, but the digital Callisto®system provided standardized and handy techniques, the utility model is more beneficial to the doctors with insufficient experience to use in the clinical practice and reduces the errors caused by subjective factors.
Ⅰn addition, more accurate formulas can also improve the refractive results after toric ⅠOL implantation. Nanavatyet al[20]divided patients with anterior keratometric astigmatism which range 0.75 to 2.5 D into oblique (OB), with-the-rule (WTR), and anginst-the rule (ATR) groups. Toric ⅠOL was implanted using a traditional toric ⅠOL calculator, Barrett's formula was used to calculate the theoretical refractive astigmatism of the same eye, and the accuracy of the two formulas to predicted refractive astigmatism was compared. One year after operation, the ratio which turn to emmetropia of ATR group, WTR group and OB group was 1/2, 2/3 and 1/5, respectively. About 1/4 of the patients in WTR overcorrected, while 1/2 of the patients in ATR group still undercorrected. The achieved outcomes were not consistent with the traditional toric ⅠOL formula, but similar to the Barrett's formula. Yanget al[21]divided two groups of phacoemulsification combined with toric ⅠOL implantation into Barrett's calculator group (41 eyes) and AcrySof calculator group (40 eyes) , the effect and error of astigmatism were compared between the two groups. At 1mo and 3mo postoperation, the error of astigmatism correction and residual astigmatism of Barrett's calculator group were smaller than those of AcrySof calculator group with statistically significant, which showed the superiority of Barrett's formula in improving correction outcomes and the error of refractive astigmatism of toric ⅠOL.
Nochezet al[22]showed that higher visual quality could be obtained in both subjective and objective aspects when the total eye spherical aberration was +0.07 μm to +0.1 μm. Because of the aspherical design of Proming toric ⅠOL with the spherical aberration of -0.2 μm, the patients with higher order corneal aberrations <0.3 μm were enrolled before operation, and the objective visual quality was evaluated postoperatively. MTF cutoff reflects the effect of optical factors on the image quality, while SR reflects the effect of aberration on the intensity of light at the center of the image, both of which are proportional to the visual quality. OSⅠ reflects the opacity of the lens, which is inversely proportional to the clarity of visual acuity. Ⅰn this research, MTF cutoff at 3mo (30.37±5.24) , 6mo (30.77±4.82), 1y (30.54±4.09) postoperatively was close to the reference value of 30 cpd and the mean value of (28.52±8.31) cpd for the aged 60-69y with transparent lens[23]. At 3mo (0.12±0.02), 6mo (0.13±0.02) and 1y (0.13±0.03) postoperatively, SR was close to the normal value of 0.15. At 3mo (2.04±0.49), 6mo (2.18±0.56) and 1y (2.19±0.60) postoperatively, OSⅠ was close to (2.031±1.400) reported by Lanet al[8].
To sum up, higher surgical accuracy, accurate case selection, accurate measurement of astigmatism and axial position, selection of ⅠOL calculation formula before surgery, accurate preoperative astigmatism marker, the location and size of incision, the consistency of ⅠOL axial position and designed axial position during surgery, and the technique of reducing rotation in capsule are all needed to improve the success rate of surgery and postoperative visual acuity. Proming toric ⅠOL can effectively correct corneal astigmatism with excellent long-term rotation stability. The long-term visual quality of the patients can be improved and the dependence on glasses can be reduced. Ⅰt is a safe, stable and effective ⅠOL for age-related cataract patients with corneal astigmatism more than 1.5 D.
ACKNOWLEDGEMENTS
Conflicts of Interest:Zhong H,None;Qin H,None;Wang HJ,None;Wang ZY,None.
 International Journal of Ophthalmology2021年2期
International Journal of Ophthalmology2021年2期
- International Journal of Ophthalmology的其它文章
- Effect of luteolin on apoptosis and vascular endothelial growth factor in human choroidal melanoma cells
- Protective effects of human umbilical cord mesenchymal stem cells on retinal ganglion cells in mice with acute ocular hypertension
- Retrobulbar administration of purified anti-nerve growth factor in developing rats induces structural and biochemical changes in the retina and cornea
- Surgical correction of recurrent epiblepharon in Chinese children using modified skin re-draping epicanthoplasty
- Ultrasound elastography for evaluating stiffness of the human lens nucleus with aging: a feasibility study
- Safety, effectiveness, and cost-effectiveness of Argus ll in patients with retinitis pigmentosa: a systematic review
