Hair Matrix Cyst
Jia-Qi Lv and Jian-Min Chang∗
Department of Dermatology, Beijing Hospital, National Center of Gerontology; Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing 100730, China.
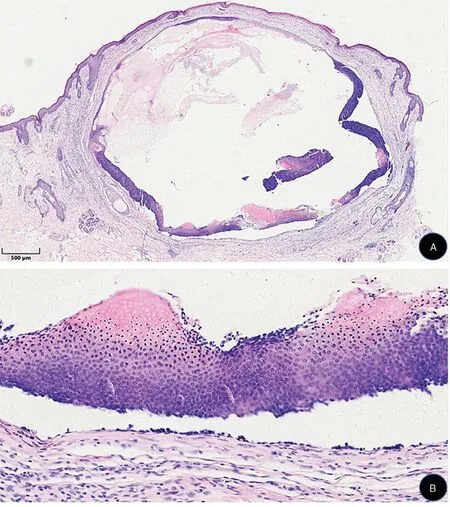
Figure 1. Histopathological characteristics of the lesion of hair matrix cyst. (A) A cystic tumor in the dermis (hematoxylin-eosin staining,×20). (B) The lower part of the cyst wall, which is composed of basaloid cells,transitional cells,and shadow cells(hematoxylin-eosin staining, ×400).

Figure 2. Clinical presentation of the lesion of hair matrix cyst.A 1cm×1cm,dome-shaped,dark-red,well-demarcated,cystic nodule with a lustrous surface and telangiectasis on the left cheek.
Histopathology
Histological examination reveals that the hair matrix cyst(HMC)is located in the dermis,and keratin is visible in the cystic cavity(Fig.1A).Part of the cyst wall is composed of stratified squamous epithelium that contains a granular layer without atypia, while the other part has the appearance of pilomatricoma composed of basaloid cells,transitional cells,and shadow cells(Fig.1B).The cyst wall is surrounded by a fibrous capsule, with peripheral inflammatory cells in a palisade arrangement. HMC is characterized by the presence of pilomatricoma-like changes (basophilic and shadow cells) within the epidermal cyst wall. The histological combination of pilomatricoma and an epidermal cyst is rare, and was first described in 1983.1Similar conditions have been reported 15 times in the English-language literature; however, in most cases,the entities were described as follicular hybrid cysts.Herein,we first name these entities as HMCs,which are special variants of hybrid cysts.The original concept of a hybrid cyst was the coexistence of infundibular and trichilemmal cysts,2which then expanded to describe a cyst that contained more than two different components of the pilosebaceous units.3HMCs have the following five pathological features.4(1) The cyst wall is composed of several layers of basal-like cells. (2) Small cystic spaces are visible between the cyst walls.(3)The cystic content contains amorphous keratins.(4)If the epithelial wall is ruptured,a foreign-body inflammatory granulomatous reaction is seen due to the release of the cyst contents into the surrounding dermis. (5) Immunohistochemistry reveals beta-catenin accumulation within the cyst wall. Beta-catenin may be involved in the regulation of proliferation and maturation of hairmatrixcells.Thereisahighnuclearexpressioninthehair matrix cells of cutaneous tumors with matrical differentiation, marking the activation of the Wnt signaling pathway within them,which drives tumorigenesis.5
HMCs are easily misdiagnosed as several cutaneous adnexal neoplasms. The differential diagnoses include epidermal cysts, pilomatricoma, trichilemmal cysts, steatocystoma,trichofolliculoma,cystic trichoblastoma,and cystic panfolliculoma, which clinically present as subepidermal nodules. At present, histopathologic examination is most helpful in attaining the correct diagnosis. The prominent feature of a HMC is shadow cells,in addition to the structure of an epidermal cyst. A HMC can be differentiated histologically from other cutaneous adnexal neoplasms based on the following features.The wall of a trichilemmal cyst consists of squamous epithelial cells with no granular layer,and the capsule is filled with keratinized material like the outer root sheath.Trichoblastoma is composed solely of basal-like cells and has no other structural differentiation.Trichofolliculoma typically demonstrates a single cystic hair follicle structure filled with keratin,with a distinct granular layer on the cyst wall. In trichofolliculoma, the epithelium with bundle-like hyperplasia is radially arranged from the center of the cyst. Panfolliculoma can differentiate into all parts of a hair follicle, with components including corneocytes in basket-woven and laminated array, trichohyalin granules of the inner root sheath, germinative cells,matrical cells,shadow cells,and papillae.6
Clinical features
HMCs most commonly occur in children and adolescents,and the exact origin is unknown.Pilomatricoma is derived from the hair matrix, whereas epidermal cysts originate from follicular infundibular epithelium. However, although pilomatricoma and epidermal cyst are derived from diverse hair follicular components,they coexist in the same entity in a HMC. Clinical examination usually reveals a dark-red, dome-shaped, well-demarcated, cystic nodule with a lustrous surface and telangiectasis (Fig. 2).Pilomatricoma-like changes are more common in the epidermal cysts of patients with Gardner syndrome1,7;however,these changes have also been reported in patients without Gardner syndrome.8Gardner pilomatricoma accompanied by cysts may arise from follicular stem cells.7The treatment of a HMC is surgical resection and careful follow-up.
- 国际皮肤性病学杂志的其它文章
- Kidney Stones Are Prevalent in Individuals with Pseudoxanthoma Elasticum, a Genetic Ectopic Mineralization Disorder
- Adverse Skin Reactions to Personal Protective Equipment Among Health-Care Workers During COVID-19 Pandemic: A Multicenter Crosssectional Study in Indonesia
- Complete Draft Genome Sequence of Cutibacterium (Propionibacterium) acnes Type Strain ATCC6919
- The Immune Function of Keratinocytes in Anti-Pathogen Infection in the Skin
- A Case Report of Pemphigoid Nodularis as Masquerader of Neurotic Excoriations
- Co-occurrence of Vitiligo and Psoriasis in an 11-Year-Old Girl: A Case Report

