A Case Report of Pemphigoid Nodularis as Masquerader of Neurotic Excoriations
Chee Hian Tan∗and Hong Liang Tey2,3
1National Skin Centre, 308205, Singapore; 2Yong Loo Ling School of Medicine, National University of Singapore, 117597,Singapore; 3Lee Kong Chian School of Medicine, Nanyang Technological University, 308232, Singapore.
Abstract
Keywords: bullous pemphigoid, pemphigoid nodularis, itch, case report
Introduction
Pemphigoid nodularis (PN) is a rare clinical variant of bullous pemphigoid (BP) characterized by both prurigonodularis-like lesions and pemphigoid-like blisters.1It is an autoimmune subepidermal blistering condition with autoantibodies directed against the 180-kDA BP antigen(BP 180)and the 230-kDA BP antigen(BP 230)located in the basement membrane zone(BMZ).1Herein,we report a case of PN in a cognitively impaired patient who has been managed as extensive prurigo nodularis with mood related neurotic excoriations until an inpatient stay.
Case report
A 72-year-old Chinese man has been followed up in a Dermatology outpatient clinic for extensive prurigo nodularis for the past 4-5 years. Physical examination revealed discrete nodules on the trunk(Fig.1A and 1B)and limbs (Fig. 1C) with linear excoriations on the back(Fig.1A).There was sparing of the mid-back demonstrating the “butterfly” sign (Fig. 1A). His face, groin, palms,and soles were not affected.
He had pseudo-dementia with depression and stayed in a destitute home. His mood was labile with an erratic behavior made worse by the intense pruritus that affected his sleep. As it was difficult to manage him in the community, the patient was admitted to the hospital for management of his mood, behavior, and extensive neurotic excoriations.

Figure 1. Clinical presentation of the patient with pemphigoid nodularis.Distribution of discrete nodules on back(A),anterior trunk(B),and right leg (C) on admission, and tense blister on right anterior thigh noted on day 3 of admission (D).
On day 3 of admission, the inpatient team started noticing tense hemorrhagic blisters on his right thigh(Fig. 1D). Histopathological examination of a biopsy specimen taken from the edge of this blister revealed a subepidermal blister with interstitial infiltrate of eosinophils (Fig. 2A). Direct immunofluorescence on periblister skin showed bright linear deposits of IgG and C3 along the BMZ (Fig. 2B). Indirect immunofluoresence on salt-split skin was positive with a roof pattern. Anti-BP 180 IgG antibody titer was elevated at >200RU/mL while anti-BP 230 antibody titer was normal.Hence, we made the final diagnosis of PN. He was treated with prednisolone at 30 mg/day, doxycycline 100mg two times a day, nicotinamide 500mg three times a day, and topical clobetasone propionate,which led to improvement of his skin lesions.The patient has been tapered off prednisolone, and is now doing well with topical clobetasol cream, orally administration with doxycycline and nicotinamide till the writing. His mood has also very much improved during following up.The patient gave his agreement for the case publication.
Discussion
PN is a prurigo variant of BP first described by Provost et al.2in 1979. The pathogenesis of PN is not well elucidated.2It is believed that prurigo nodules are induced by rubbing and scratching in individuals with subclinical pruritic BP.Another theory is that trauma(scratching)and localized inflammation release self-antigens within BMZ,inducing pemphigoid antibodies2in predisposed individuals such as the elderly in whom the immune aging processes increase the risk for the activation of autoaggressive T cells and formation of IgG autoantibodies.3
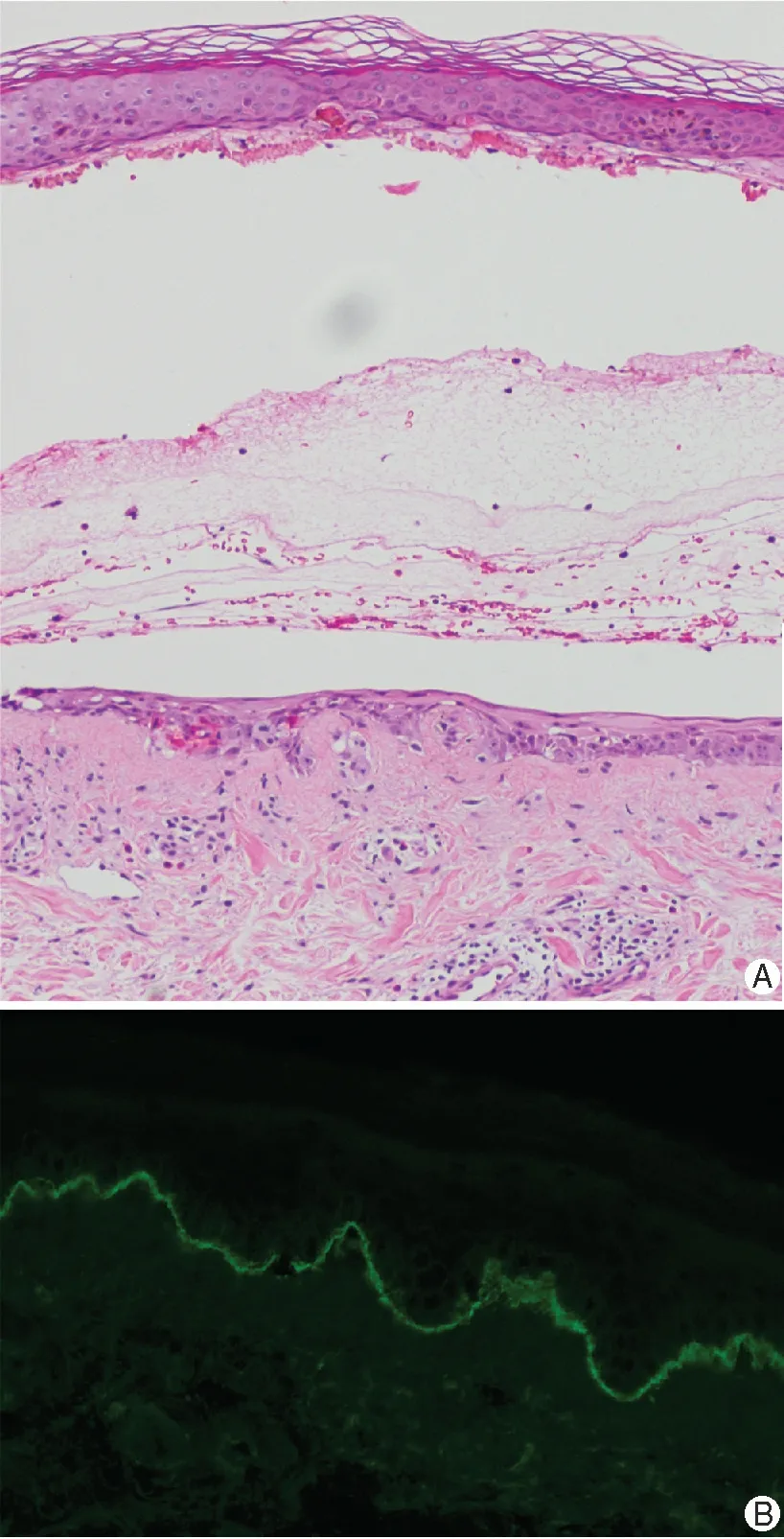
Figure 2. Histopathologicalexaminationofthepatientwithpemphigoid nodularis.A biopsy specimen taken from the edge of the tense blister notedonday3ofadmission.(A)Hematoxylinandeosinstainsdisplaying subepidemal cleft with its blister floor composed of a partially regenerated epidermis.Therewassuperficialperivascularandinterstitial infiltrate of lymphocytes with increased numbers of eosinophils(×10).(B)Direct immunofluroscence on perilesional skin revealed bright linear deposits of IgG along the basement membrane(× 20).
Clinically, PN can be easily misdiagnosed as prurigo nodularis.The condition may present as lesions classical of prurigo nodules for several years before bullae develop5or are being noticed. Bullae if present, may arise at sites of nodular lesions or on previously clinically uninvolved skin.1,4-5Nonetheless, there may be some clinical clues that could raise the suspicion of an underlying immunobullous disorder. Individual PN nodules may be more erythematous,6with a much larger surface area being affected by central erosion and ulceration.6These were evident in our patient’s skin lesions(Fig.1).Itch associated with larger areas of erosion and ulceration are clues that the lesions can be more than mere excoriations, and the physician should investigate for secondary causes of pruritus.
In conclusion,it is important for clinicians to be aware of the presentation of prurigo nodularis in association with BP, such that effective treatment can be promptly instituted. Our patient continued to improve not only in terms of skin lesion recovery,but his mood and behavior had also improved dramatically with the resolution of itch.
- 国际皮肤性病学杂志的其它文章
- Kidney Stones Are Prevalent in Individuals with Pseudoxanthoma Elasticum, a Genetic Ectopic Mineralization Disorder
- Adverse Skin Reactions to Personal Protective Equipment Among Health-Care Workers During COVID-19 Pandemic: A Multicenter Crosssectional Study in Indonesia
- Complete Draft Genome Sequence of Cutibacterium (Propionibacterium) acnes Type Strain ATCC6919
- The Immune Function of Keratinocytes in Anti-Pathogen Infection in the Skin
- Co-occurrence of Vitiligo and Psoriasis in an 11-Year-Old Girl: A Case Report
- Erosive Adenomatosis of the Nipple Masquerading as Paget’s Disease:A Case Report

