The Past 70 Years in Control of Syphilis in China: Elimination and Responses to Resurgence
Xiang-Sheng Chen∗, Ting-Ting Jiang, Yue-Ping Yin, Qian-Qiu Wang
National Center for STD Control; Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, Jiangsu 210042, China.
Syphilis is a sexually transmitted disease(STD)caused by the spirochete bacterium Treponema pallidum subspecies pallidum. Historically, syphilis was called as the “great pox” in order to distinguish it from smallpox and given many national attributions, such as the French pox, the English pox, and the Italian pox, due to that the disease was often believed to be spread by sailors and soldiers in the country during their unprotected sexual contact with local prostitutes.1The French pox was widely used before it was named syphilis by the Italian physician and poet Girolamo Fracastoro in 1530.2Syphilis first reached Canton (Guangzhou) of China through the sea in 1505 and was called“Canton sores”or“Canton rash”(kuang chuang). However, “plum-blossom sores” (yangmei chuang) was more widely used in medical records in China because they had a shape resembling plumblossoms. Syphilis is transmitted through unprotected sexual contact with an infected person. It can also be passed from an infected mother to her unborn child.If left untreated,syphilis often progresses to later stages and can cause heart problems, psychological disorders, blindness,and death.In era of human immunodeficiency virus(HIV)epidemic,syphilis infection has become a facilitating factor to increase the risk of contracting HIV by up to four-fold and transmitting HIV by up to nine-fold.3China has a long history of syphilis epidemic but the great successes in control of the disease have been made during the past 70 years in China.
The important events in China’s responses to syphilis epidemic during the past 70 years are shown in Figure 1.The 70 years can be divided into five milestone periods,namely rampancy of prostitution and pandemic of syphilis(1949-), nationwide campaign to eliminate syphilis(1954-1964), disappearance of syphilis from public and medical eyes(1965-1979),resurgence of and responses to syphilis epidemic (1980-), and increasing efforts to syphilis control (2010-).4
This perspective is aimed to provide a narrative review of syphilis in terms of responses to syphilis epidemic over the past seven decades, particularly after resurgence of the disease5in China. For this purpose, we simply call these responses as the national syphilis control campaigns and describe them as the first campaign during 1949-1964 and the second campaign after 1980s.
The first national syphilis control campaign(early 1950s-1964)
Syphilis and other sexually transmitted infections (STIs)were major public health and medical concern in early time of the foundation of New China in 1949.According to the data gathered during that time, the prevalence of syphilis was as high as 84.9% among women who sold sex in Beijing,65%-10% of the population in some urban communities and 0.5%-4% of rural residents in some areas.7In 1949,syphilis accounted for about one-tenth of patients in the dermatology department of the Beijing Medical College.8Syphilis was also a serious health problem in some minority areas due to local customs.In a study in minority areas of five provinces (including Inner Mongolia, Xinjiang, Yunnan, Guangxi, and Gansu),syphilis prevalence was found to be 57.2% in 1951 and 44.3% in 1952. By 1950, it was believed that there were more than 10 million persons infected with an STD,most of them suffering from syphilis in China.9
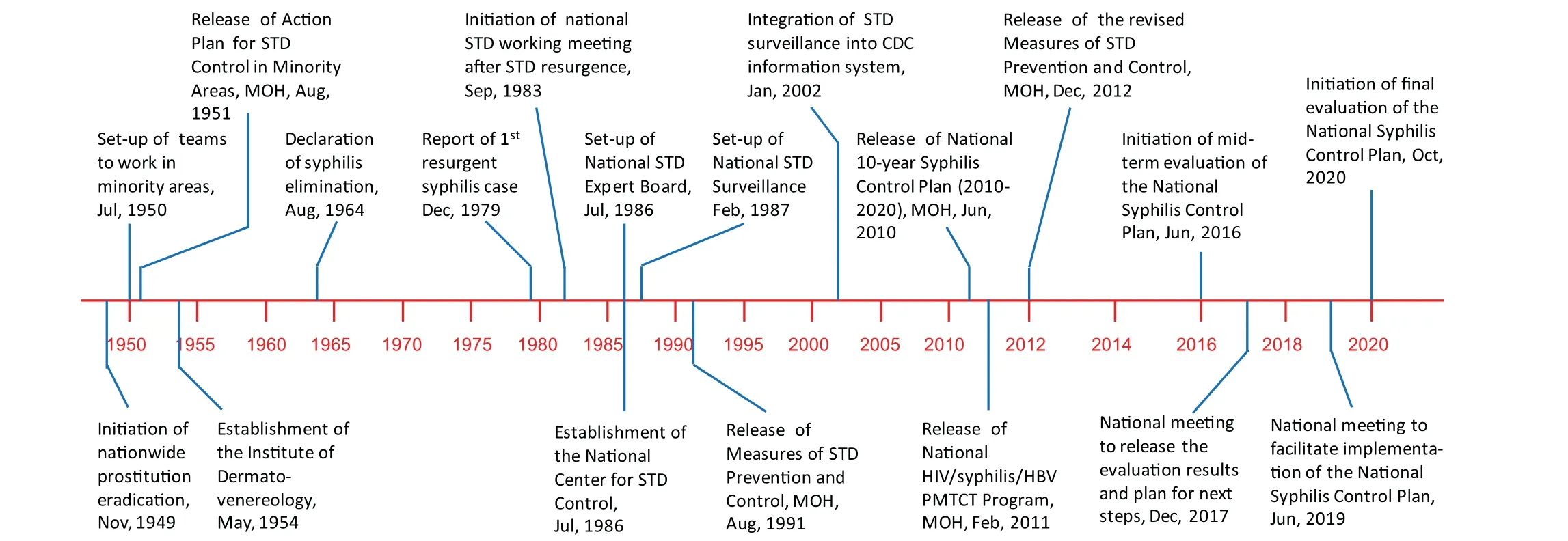
Figure 1. Important events in China’s responses to syphilis epidemic,1949-2020.STD:sexually transmitted disease;MOH:Ministry of Health;CDC:Centers for Disease Control and Prevention;HIV:human immunodeficiency virus;HBV:hepatitis B virus;PMTCT:Prevention of Mother-to-Child Transmission.
To respond to the epidemic, the Chinese government -Ministry of Health (MOH) set up a national team specifically for working on developing national strategies to control syphilis and other STIs, particularly in the syphilis-epidemic minorities areas, followed by release of the Action Plan for Control of Venereal Diseases in Minority Areas by MOH in early 1950s. In addition,syphilis was highlighted as an important health concern in the National Program of Agriculture Development in 1956 and considered as one of most harmful diseases to be eliminated in the country. Since then, the first national syphilis control campaign had been implemented throughout the country. Activities of the campaign consisted of crackdown on prostitution, mass education, wide screening for syphilis, and free treatment of infected cases.
As prostitution was the key issue for spread of the disease, one of the first steps taken for control of syphilis was the closure of brothels and the liberation of prostitutes,including that the government closed brothels,gave the prostitutes legal and property rights, created a new job for them,helped them set up home and return to their families.10-11Most of the“institutionalized forms of commercial sex” were wiped up within a few days or weeks,although it took a few years to completely eliminate the prostitution nationwide. Delivering the knowledge through propaganda efforts was used not only as a help way to tell people about the disease and prevent their risk behaviors but also an efficient strategy to encourage or guide the people who had risk behaviors to search for clinical examination and blood testing.Free screening for syphilis become the key to initiate the medical interventions.Different screening strategies were selected to use in different areas according to local situations. In minority areas with high prevalence of the infections, mass screening for syphilis was conducted in community. In rural areas where prevalence was relatively low, health education was carried out first,followed by the screening among persons with suspect clues. In urban areas, mass screening for syphilis was done among residents of certain age groups or service workers, and the screening was integrated into premarital health check-up, prenatal care,and school enrollment and military service health checkups. Several regimens, including arsenic and bismuth therapy,penicillin therapy and a traditional Chinese herb therapy, for treatment of syphilis were recommended by MOH to scale up nationwide. Based on these screening algorithms and treatment regimens, free screening for syphilis was widely available and those cases found to be infected with syphilis were treated by local prevention teams. For example, during 1950-1956, a total of near half million residents living in pastoral areas of 51 counties in Inner Mongolia were screened for syphilis and more than 110 thousand syphilis cases were treated.12To support to implementation of the national campaign in the country, a professional and vertical health system called dermato-venereological network was established to consist of one institution at top national level - the Central Institute of Dermatology and Venereology (currently the Hospital for Skin Diseases [Institute of Dermatology],Chinese Academy of Medical Sciences and the National Center for Sexually Transmitted Disease [STD] Control)set up in 1954,dozens at provincial level,and even more at prefectural and county levels.
After the comprehensive efforts for 15 years,syphilis was almost eliminated (“basically eradicated” in Chinese context) across the country in 1964. The elimination can be witnessed by not only the significant decrease in prevalence of syphilis infections among residents in minority areas in five epidemic provinces4but also the data from several census surveys among residents during 1960 and 1963.In a census of skin diseases among near 750 thousand residents in 1960, only one case with relapsed secondary syphilis was detected and no case was found in the following census surveys of 6,708, 185,615, and 415,320 residents in 1961,1962,and 1963,respectively.13Among more than 770 thousand patients attending at dermatology clinics in 24 hospitals from seven cities,4,190 cases with syphilis and 26 cases with primary syphilis were detected, giving the prevalence rates of 0.54% and 0.004%, respectively.10Achieving the elimination of syphilis by 1964 marks the success of the first syphilis control campaign in China and also becomes one of the public health achievements in the New China.It should be noted that a generation of health workers in the field of dermato-venereology and public health, particularly including Drs. Ma Hai-de, Hu Chuan-Kui, Li Hong-Jiong, Ye Gan-Yun, and a lot of others made a great contribution to the success.
The second national syphilis control campaign(1986-)
Syphilis had almost disappeared from public eyes and medical society until the early 1980s. However, since the fundamental “economic reforms” and “opening up to outside world” were introduced in the late 1970s in the country,sociocultural environment and social norms have been changed significantly,resulting in inequality between poor and rich, sexual mores to more tolerate toward extramarital or commercial sex, and migrations of men and women from rural or underdeveloped areas into the urban cities in search of jobs.These changes have created the breeding grounds for resurgence of syphilis and other STDs. The first resurgent case of syphilis was officially reported in December 1979.To respond to the resurgence,the MOH decided to restore the public health system for prevention and control of syphilis and other STDs by designating the Chinese Academy of Medical Sciences Institute of Dermatology as the National Center for STD Control in 1986 to technically coordinate the national efforts, and setting up the National STD Case-reporting System based on 16 urban surveillance sites in 1987.The surveillance system was scaled up nationwide in 1988,largely assembled in the 1990s and integrated into the China Information System for Disease Control and Prevention in 2002.
According to the findings from the National Casereporting System,China’s reported syphilis cases had been rising by about 30% annually by the late 1990s.14The reported incidence of syphilis more than tripled between 2005 and 2011, to 32.0 cases per 100,000 people. This increasing trend was continuously observed in 2012. In addition, the prevalence surveys carried out among different populations have indicated a high disease burden of syphilis infections in China,15and female sex workers(FSWs) and men who have sex with men (MSM) are the subgroups at highest risk of syphilis infection,16-17particularly among FSWs at middle-and low-tier venues.18Unlike the epidemic pattern in 1950s,the current epidemic has affected more groups of population.
Since syphilis returned to China,intensive interventions targeting on changes of risk behaviors by health education and condom promotion have been prioritized in the syphilis control strategies since early 2000s.19However,these behavioral change-based interventions did not achieve the expected effect, showing a rapid increase of national reported incidence of syphilis infection.Facing the continually increasing spread of syphilis in the country,the government has recognized the needs to strengthen the efforts in respond to the epidemic. Specifically, in June 2010, the China’s MOH officially launched the first national program, the National Program for Prevention and Control of Syphilis in China for Years of 2010-2020(National Syphilis Control Program), specially and directly aimed at controlling syphilis.20China is one of a few countries with national programs for syphilis control. This Program includes the national milestone of achieving an explicit decline in the reported incidence of primary and secondary syphilis(reflecting the intensity of recent transmission) and the elimination of congenital syphilis,defined as fewer than 15 per 100,000 live births,by 2020, indicating specific targets for percentages of target populations educated about syphilis, tested and treated for syphilis.
In 2011, the Ministry further released a national program specifically aimed at Preventing Mother-to-Child Transmission (PMTCT) of HIV, syphilis, and hepatitis B.21For implementation of these two parallel programs,the central government has tagged more than$3.2 million specially allocated for syphilis prevention and control and a separate $140 million pool of funding for the triple PMTCT program every year.4,21These commitments have provided a strong foundation for and commitment to syphilis control in the country.
Vaccination is the most efficient way to prevent and eliminate syphilis in communities. However, vaccine for syphilis is still under research and not possible to be available in the near future.22Therefore,a comprehensive program consisting of health education to change risk behaviors,screening of target population,and treatment of infected cases is still the only effective means to curb the epidemic currently. While most components of the comprehensive program remain similar to those introduced in the 1950s,big differences exist.The resurgence of syphilis in China may need to be responded by more novel and responsive public health approaches.Universal access to active screening, reliable diagnosis and effective treatment would have a major impact on the current STD epidemic in China. Based on evidence from many pilot studies and implementation research,23the emphasis in syphilis control in China has been now placed on early detection of infections through enhancing screening program followed by treatment of infected cases. Additional to continuing efforts in health education and condom promotion through integrating with the HIV prevention program and the specific program for preventing mother-to-child transmission of syphilis, the “Three Screenings and Linkage to One Standardized Care (3×1 SLSC)” with strengthening of the surveillance and testing systems have been proposed as core technical strategies to ensure implementation of the National Program for Syphilis Prevention and Control.4,24Expanding syphilis screening is an essential response to China’s syphilis epidemic. Screening for target populations as part of outreach interventions must be considered and there have been promising pilot programs.23Introduction of point-ofcare testing services into high-risk population settings is well accepted by the target populations when it is integrated into currently ongoing outreach services.25
With implementation of the 3×1 SLSC strategies, the uptakes of screening for syphilis among target populations and treatment with benzathine penicillin for syphilis in the infected cases have improved significantly nationwide.Unpublished data from the mid-term evaluation of the National Syphilis Control Program in 2016 indicated that the uptake of active screening for syphilis among patients at potential risk of syphilis in general hospitals was more than 60% and two-thirds of the patients serologically positive for syphilis were treated with benzathine penicillin.Impact of the expanded screening and treatment efforts has been proved by an observed decline in annual incidence of active syphilis over the years. The data from the national surveillance program have indicated a turning point towards decreased incidence of primary and secondary syphilis (usually defined as active syphilis)appeared in 2012 and one year later the turning points for congenital syphilis occurred.26
Future challenges
Despite the progress in control of syphilis in China,a lot of challenges still remain. The key affected populations including MSM and FSWs disproportionately bear the burden of the Chinese syphilis epidemic.Among MSM,a substantial proportion of men with syphilis infection are also positive for HIV,reflecting a facilitation of the disease transmission in this population. However, these populations are usually hard to reached for interventions and marginalized from obtaining needed services. Both homosexual and heterosexual behaviors are common among MSM population in China and a substantial proportion of sexually active men have access to commercial sex.27-28Therefore, the transmission of syphilis from key groups to general population is an important consideration.
Syphilis control program in China continues to face increasing pressures from high demand but low resourceshuman and financial resources. Although the Chinese government has demonstrated its commitment and willingness to take action to control syphilis,multisectoral responses from relevant agencies to the epidemic are not sufficient for translating the program into action.Specifically, active participation of clinic-based health services in syphilis prevention and control is significantly insufficient.Social stigma towards those at risk or infected with syphilis is still recognized as a major barrier to syphilis control,29because it prevents people from seeking services for testing and treatment.
Technically, innovative strategies will be needed to ensure feasibility, accessibility, acceptability, and costeffectiveness of these strategies in the real-world. The current point-of-care tests widely used in China to detect treponemal antibody are unable to differentiate between currently active and historically infected (or treated)infection, which limits the application of these tests alone to guide diagnosis and treatment in persons from high-risk groups, who usually have a high lifetime exposure to syphilis.Although benzathine penicillin is still effective for treatment of syphilis, increasing patients experienced as having penicillin allergy have been reported. In addition,benzathine penicillin was still not available in clinical settings in some areas in China.30Meanwhile along with clinically significant resistance to macrolides,a second-line alternative to penicillin, has emerged with a high prevalence in China. Additionally, clinical diagnosis and management of neurosyphilis particularly among HIVinfected cases can be challenging along with an increasing report of cases with neurological treponemal involvement in recent years.
In summary, there are still many socio-economic,operational,and technical barriers to hamper the successful implementation of syphilis control in China.Although the challenges are still substantial, if we build on the past accomplishments from implementation of the National Syphilis Control Program indicating a decline in the national incidence of primary and secondary syphilis,there is every reason for optimism that the secondary national syphilis control campaign will be as successful as the first one in the foreseeable future, with a similarly dramatic impact in public health and reproductive health in China.
- 国际皮肤性病学杂志的其它文章
- Kidney Stones Are Prevalent in Individuals with Pseudoxanthoma Elasticum, a Genetic Ectopic Mineralization Disorder
- Adverse Skin Reactions to Personal Protective Equipment Among Health-Care Workers During COVID-19 Pandemic: A Multicenter Crosssectional Study in Indonesia
- Complete Draft Genome Sequence of Cutibacterium (Propionibacterium) acnes Type Strain ATCC6919
- The Immune Function of Keratinocytes in Anti-Pathogen Infection in the Skin
- A Case Report of Pemphigoid Nodularis as Masquerader of Neurotic Excoriations
- Co-occurrence of Vitiligo and Psoriasis in an 11-Year-Old Girl: A Case Report

