Comparing the incidence of major cardiovascular events and severe microvascular complications in patients with type 2 diabetes mellitus: A systematic review and meta-analysis
Ying-Ying Zhu, Zu-Yao Yang, Ping Li, Xin-Ying Huang,Xue-Hong Zhang,Li-Nong Ji, Jin-Ling Tang
Ying-Ying Zhu, Zu-Yao Yang, Ping Li, Xin-Ying Huang, Jin-Ling Tang, Division of Epidemiology, The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, China
Xue-Hong Zhang, Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, MA 02115, United States
Li-Nong Ji, Department of Endocrinology and Metabolism, Peking University People's Hospital, Peking University Diabetes Centre, Beijing 100044, China
Abstract
Key Words: Diabetes mellitus; Diabetic complications; Cardiovascular disease; Diabetic retinopathy; Diagnostic criteria; Anti-diabetic drugs
INTRODUCTION
Since 1980, the number of patients with diabetes mellitus has nearly quadrupled to 422 million in 2014 worldwide[1]. Type 2 diabetes mellitus (T2DM), accounting for over 90% of all diabetes cases, can cause both macrovascular (mainly cardiovascular disease) and microvascular (e.g., retinopathy, neuropathy, diabetic foot) complications[2,3]. Hyperglycemia causes microvascular complications by activating the protein kinase C, resulting in abnormal microvasculature characterized by endothelial dysfunction, smooth muscle cell proliferation, increased vascular permeability and angiogenesis[4,5]. In addition, oxidative stress, advanced glycation end products and chronic low-grade inflammation also play important roles in the pathogenesis[6-8]. Microvascular complications are not limited to those occurring in the retina, kidneys, and nerves, but may also affect other organs[9]. For example, diabetes mellitus can cause coronary microvascular dysfunction, which reduces the coronary flow serve and leads to the failure of a normal functioning microvasculature[10].
Despite the potential damage to multiple organs caused by microvascular complications, they are generally less serious than macrovascular complications in terms of the number of deaths, health care cost and decreased quality of life they cause in T2DM patients[11-13]. However, for some historical reasons, macrovascular complications have been less considered in developing the definition of T2DM (e.g., which glycemic measures and which diagnostic thresholds to use) which is largely dominated by concerns about microvascular complications, in particular retinopathy[14-17].
Moreover, the efficacy of anti-diabetic drugs is also evaluated according to their effects on microvascular complications[18]. Macrovascular complications, if included, are often considered as safety indicators or adverse effects of anti-diabetic drugs[19,20]. However, it is indeed observed that some glucose-lowering drugs which can reduce the risk of microvascular complications increase the risk of macrovascular complications in T2DM patients[21,22]. Consequently, trials based only on microvascular complications could mistakenly endorse drugs that can reduce microvascular complications at the cost of increasing macrovascular complications.
If severe macrovascular complications occur as commonly as or more commonly than severe microvascular complications (SMICs) in patients with T2DM, the diagnostic criteria, evaluation of anti-diabetic drugs and practice guidelines may have to be reviewed by considering more about macrovascular complications. We thus conducted this systematic review and meta-analysis to compare the incidence of major cardiovascular events (MACEs) and SMICs in T2DM patients.
MATERIALS AND METHODS
This systematic review and meta-analysis summarized direct comparisons of the incidence of MACEs with that of SMICs in the same patients with T2DM in cohort studies or clinical trials. The PRISMA guidelines were followed in this review[23]. This review has not been registered.
Literature search
We searched MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials from inception to September 2017, with no language restriction. Terms for cardiovascular disease, microvascular disease, T2DM, and study design (cohort and trials) were used to identify potentially relevant studies. Detailed search strategies are included in Supplementary Tables 1 and 2. We also manually reviewed the reference lists of eligible articles and important reviews on the topic to look for additional studies.
Study selection
After initial scan of titles and abstracts of cohort studies and trials, full-texts of potentially included studies were further reviewed for their eligibility. A study was deemed eligible if its sample size was > 1000, included patients with T2DM aged ≥ 18 years, and reported absolute number of cases or incidence for both MACEs and SMICs. Although one thousand is an arbitrary cutoff, studies with fewer than 1000 participants would have too few microvascular events to allow for reliable estimation of the incidence of SMICs and add little to the included studies. These studies were thus excluded. We also excluded studies conducted in special subgroups of diabetic patients, such as those wholly with cancer or cardiovascular disease and those receiving dialysis at baseline.
In this systematic review, no matter for the MACEs and SMICs, we included the mainly serious types of macrovascular and microvascular complications respectively. MACEs were generally defined as nonfatal myocardial infarction and stroke, and cardiovascular death. SMICs, for which there was no standardized definition, were defined as serious retinopathy, nephropathy, and foot disorder. The reason for choosing these complications as SMICs was that they represented three serious types of microvascular complications, which have the equal severity with MACEs. Serious retinopathy included severe loss of vision, blindness, or laser therapy for retinopathy[24-26]. Serious nephropathy included renal failure, dialysis, end-stage renal disease or renal death[27]. Serious foot disorder included limb amputation or death from peripheral artery disease[3]. Noticeably, by taking retinopathy which requires laser therapy and amputation as SMICs, we slightly over-estimated the incidence of SMICs, which could lead to a more conservative estimate of the risk of MACEs relative to SMICs.
It takes a long time to have all these complications occur in T2DM patients and some studies may have no event for some complications, particularly for severe microvascular ones. Thus, we also included studies that lacked data on only one type of event just to ensure having enough eligible studies in this review.
Study selection was completed independently by three researchers (Zhu YY, Li P, Huang XY). The disagreements were settled by discussions with a more experienced reviewer (Yang ZY).
Data extraction
The following data were extracted from each eligible study: Bibliographic information (e.g., first author, publication year, study location), baseline characteristics (e.g., number of participants, mean age, sex, and diabetes duration), length of follow-up and outcomes including information on definition of MACEs and SMICs, number of people at risk, number or cumulative incidence of each outcome event).
For multiple reports of the same study, we extracted data from the report with relatively longer follow-up and more complete information. For clinical trials, data in the intervention and control groups were extracted separately and considered as two separate cohorts in the data analysis.
Data extraction was completed by three researchers (Zhu YY, Li P, Huang XY). This process was double-checked by another reviewer (Yang ZY). The disagreements were settled by discussion.
Quality assessment
Methodological quality of included studies was assessed by Zhu YY, using a 5-item scale adapted from the Institute of Health Economics and the Newcastle–Ottawa Quality Assessment Scale (Supplementary Table 3)[28,29]. The scale evaluated each study based on the population (1 items), outcome measurement (1 item), results (2 item), competing interests and source of support (1 item). For each assessed study, 1 point was assigned to each item if the criterion was met, and a score of 3.5 or more suggests high quality.
Data synthesis and analysis
In each study, the incidence was estimated as the number of MACEs and SMICs divided by the number of participants at risk respectively. Because some studies reported different numbers of people at risk for different types of SMICs or MACEs, the smallest number of people at risk for SMICs was used as denominator, and the largest was used for MACEs in order to avoid over-estimation of the macrovascular over microvascular complication ratio. In occasions where data on a particular type of MACEs or SMICs was missing, the average incidence estimated from all other studies was used to make it up in the analyses.
In each study, the relative risk (RR) was the ratio of the incidence of MACEs over that of SMICs. The random effect model was used in meta-analysis to estimate the overall RR and its 95%CI. Heterogeneity was evaluated using Cochran’sQtest andI2statistics[30]. Heterogeneity was judged present if thePvalue ≤ 0.10 for Cochran’sQor anI2statistic ≥ 50%. Begg’s funnel plot and Egger’s test were used to test the potential publication bias[31]. Previous studies have found age, follow-up time, and diabetes duration are associated with macrovascular and microvascular events in patients with T2DM[32]. Besides, different types of study (cohortvstrial) were included in our review. In theory, the drugs tested in trials may affect the incidence of complications, thus affecting the risk ratio (although the result of subgroup analysis showed no significant difference). Therefore, subgroup analyses were conducted according to study design, age at baseline, follow-up period, duration of diabetes to investigate the potential sources of heterogeneity. We planned to do the multivariate meta-regression analysis incorporating all factors mentioned above, but did not actually do it because of the limited number of eligible studies (< 10 times the numbers of factors) as recommended by Cochrane Handbook.
Sensitivity analyses were conducted by excluding studies with missing data on a particular type of SMICs, by excluding those including laser photocoagulation therapy as serious retinopathy, and by combining the data in intervention and control groups from a trial into one cohort rather than taking them as two. A two-tailed significance level of 0.05 was used for all the statistical tests, except forQtests of heterogeneity for which 0.10 was used. Analyses were performed using RevMan 5.3 and STATA 14. The statistical methods of this study were reviewed by Dr. Jean H. Kim from the Chinese University of Hong Kong.
RESULTS
We identified a total of 52577 references from the electronic databases. Figure 1 shows the flow chart of selection process. Finally, 12 studies (eight cohort studies[33-40]and four clinical trials[41-45]) were eligible for this review. The incidence of MACEs and that of SMICs in the ACCORD study were extracted from two different papers[42,43].
The characteristics of the included studies are summarized in Table 1. Among fourclinical trials, three (ACCORD[43], ADVANCE[45], and VADT[41]) were conducted to assess the effect of the intensive glucose lowering treatment (vs standard treatment) and Marre et al[44]study for the effect of ramipril (vs placebo) on macrovascular and microvascular complications. Totally, 387376 patients with T2DM (50% males) were included in this review. The patients had a mean age of 61 (range: 51-74) years old, mean duration of diabetes of 6 (range: 0-11.5) years, and mean HbA1c level of 8.4% (range: 7.5%-10.2%). The patients were followed up for a mean duration of 6.6 (range: 1.6-19) years. The details about definitions and numbers of MACEs and SMICs reported in each eligible study are shown in Supplementary Tables 4 and 5 separately. In the 12 eligible studies, two studies (ACCORD[43]and ADVANCE[45]) did not report data on serious diabetic foot and one (Kanayaet al[38]) on serious retinopathy. No missing data were found on MACEs.
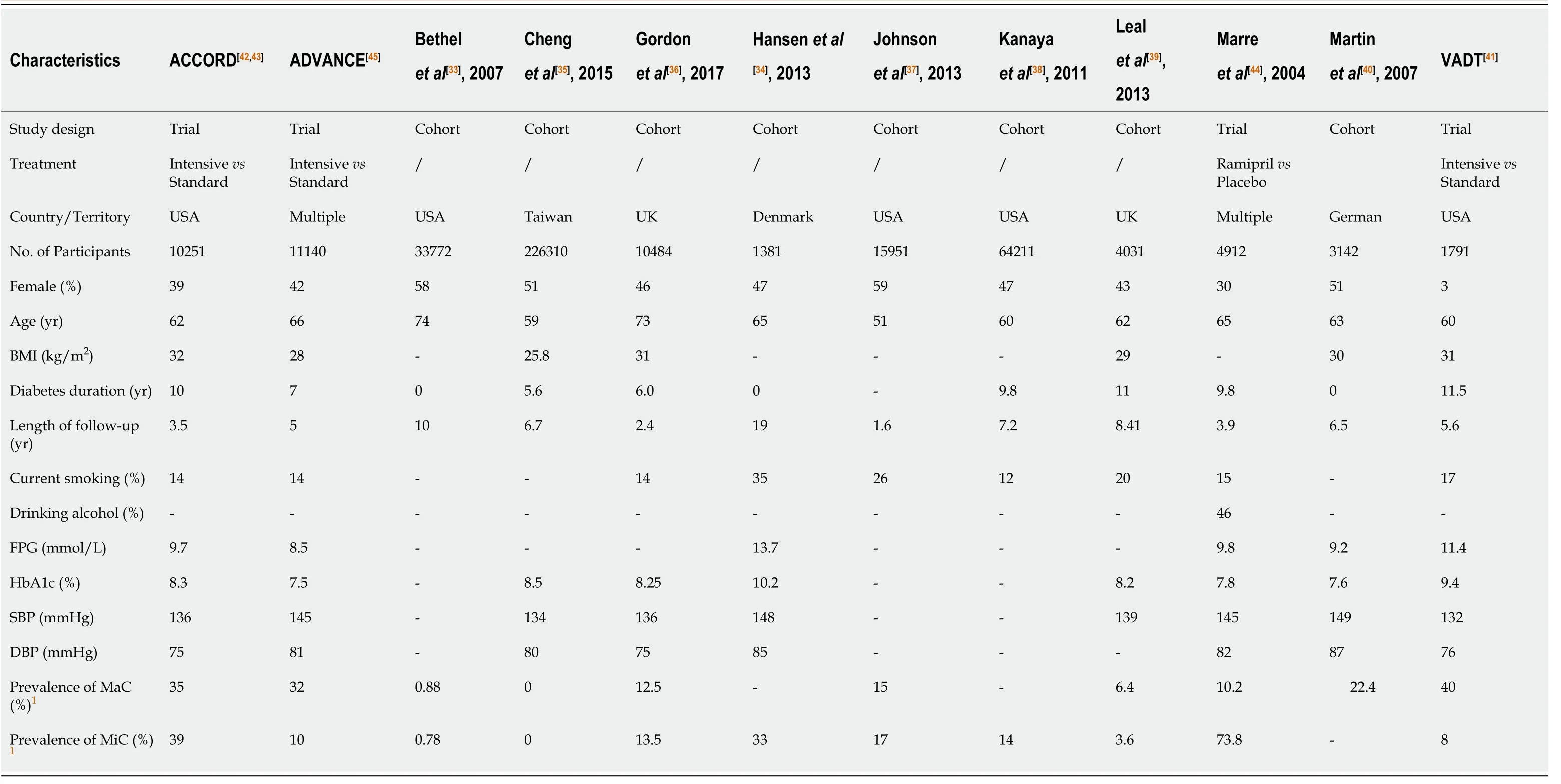
Table 1 Baseline characteristics of eligible studies
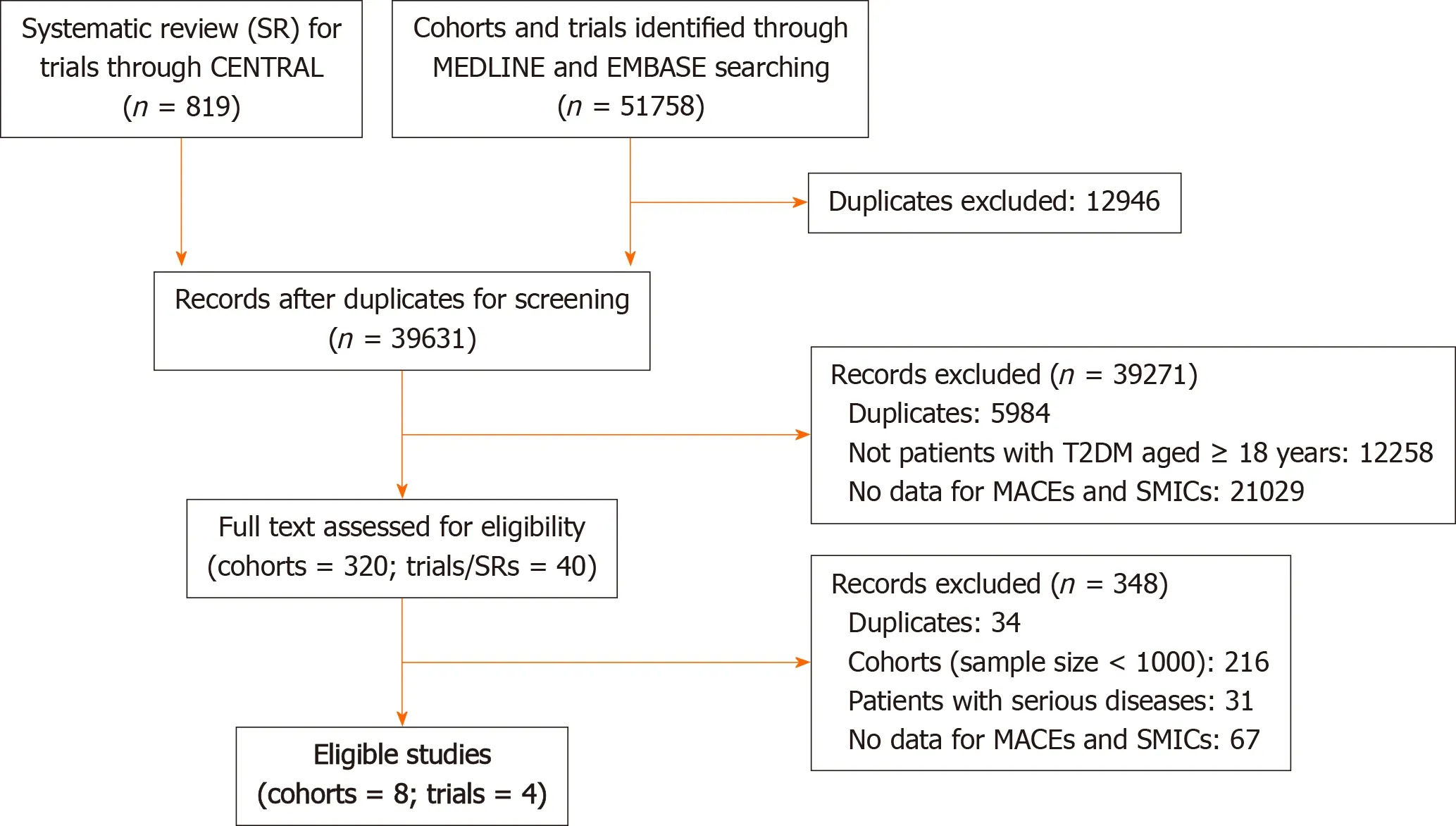
Figure 1 The flow chart of search and selection of eligible studies.
Among the 12 eligible studies, participants from five studies (Bethelet al[33], Chenget al[35], Hansenet al[34], Kanayaet al[38], and Martinet al[40]) were considered representative of the general patients with T2DM. Except Chenget al[35]’s study, all studies did not exclude those with known macrovascular or microvascular complications at baseline. The studies’ scores ranging from two to five. As a result, six studies[33-35,38,41,43]were considered methodologically as high quality (≥ 3.5). Detailed results are shown in Supplementary Table 6.
Incidence data from the intervention and control arms of clinical trials were considered as two separate cohorts in the data analysis. Therefore, 16 cohorts (eight cohort studies plus eight cohorts from four clinical trials) were finally included in the meta-analyses. Figure 2 summarizes the incidence of MACEs relative to that of SMICs in patients with T2DM in each cohort. The pooled RR for all 16 cohorts is 2.02 (95%CI: 1.46–2.79). Substantial heterogeneity was found (I2= 99%). The funnel plot (Supplementary Figure 1) was visually and statistically symmetrical (Egger’s testt= -1.46,P= 0.167), suggesting no evidence of publication bias in the included studies. Results of subgroup analyses according to age, study design, length of follow-up and duration of diabetes are shown in Table 2. The incidence of MACEs was consistently higher than that of SMICs in all subgroups. However, study design is statistically significantly associated with the RR. The summarized RR is higher in cohort studies than in clinical trials. Study design explained 43.7% of the overall heterogeneity.
The RRs became even larger in all sensitivity analyses. After excluding five cohorts from three studies (Kanayaet al[38], ACCORD[43], and ADVANCE[45]) that had missing data on a particular type of SMICs, the combined RR was even larger and remained statistically significant (RR = 2.66, 95%CI: 1.85-3.81). As anticipated, the RR was also increased considerably (RR = 2.26, 95%CI: 1.67-3.06) after excluding six cohorts from four studies (Chenget al[35], Hansenet al[34], VADT[41], and ADVANCE[45]) that included laser photocoagulation as severe retinopathy. Besides, combining the intervention and control cohorts in each trial[41-45]into one cohort also made the combined RR larger (RR = 2.22, 95%CI: 1.53-3.24).

Table 2 The risk of major cardiovascular events to that of severe microvascular complications: Subgroup analysis

Figure 2 Meta-analysis of the incidence of major cardiovascular events over severe microvascular complications in type 2 diabetes patients.
DISCUSSION
We identified 16 eligible cohorts and the combined result showed that in patients with T2DM, MACEs occurred twice as commonly as SMICs. Qualitatively, the conclusion remained consistent regardless of age, study design, length of follow-up, and duration of diabetes.
Quantitatively, the relative risk differed considerably according to study design. The summarized RR was much lower in the clinical trials than in cohort studies. This may be partly attributed to the use of a much broader definition of SMICs by including laser photocoagulation as serious retinopathy in the two of these four trials (VADT[41]and ADVANCE[45]). T2DM patients with mild-to-moderate retinopathy are recommended laser photocoagulation therapy to relieve the symptoms and delay or prevent vision loss, suggesting majority of patients taking laser therapy in these trials did not have severe retinopathy[46]. In addition, the number of T2DM patients receiving laser therapy in the same trials is 2-3 times more than that in those who developed severe vision loss or blindness[33,39,47]. Therefore, including laser photocoagulation as serious retinopathy in these two trials may partly explain why trials are more likely to report a lower RR.
Meanwhile, clinical trials, like ACCORD and ADVANCE, usually set the follow-up frequency as every 1 or 2 months, while patients in cohort studies were visited every 1 or 2 years, or even longer. Thus, another possible reason for the difference between cohort studies and clinical trials is the intensive follow-up and rigorous examination in clinical trials which may detect more SMICs outcomes in clinical trials than in cohort studies. Noticeably, even though its summarized RR is relatively smaller, the conclusion remains consistent in clinical trials that MACEs occur more often than SMICs in T2DM patients.
Previous meta-analysis has shown that the risk of MACEs was more than doubled in diabetic patients than in non-diabetic people[48]. Meanwhile, our meta-analysis showed that the incidence of MACEs was two times that of SMICs in diabetic patients. Based on these information, it can be inferred that in a given population the absolute number of MACEs attributable to diabetes is greater than that of SMICs, even if the attributable risk for SMICs is 100%. The difference would be bigger if deaths caused by MACEs were compared with those by SMICs.
Therefore, the findings of this study have important implications regarding T2DM by taking the severity and frequency of complications into consideration. First, macrovascular complications should be given a greater weight than microvascular complications in developing or modifying the diagnostic criteria for T2DM. For example, is the relation between blood glycemic measures and the risk of macrovascular complications similar to that for microvascular complications? Do they suggest the same cutoff values for diagnosing diabetes? Further investigations are thus entailed to address these questions.
Second, our findings also suggest that macrovascular complications should be also considered in the evaluation of the efficacy of anti-diabetic drugs in patients with T2DM. Currently, microvascular complications are frequently used in quantifying the effect of glucose-lowering drugs, while macrovascular complications that are more common as shown in this study and more severe than microvascular complications are sometimes not considered. There is even evidence that some anti-diabetic drugs can reduce the risk of microvascular complications but at the same time show no effect or even increase the risk of macrovascular complications[18,21,22]. Our study suggests that it is time to review the current practice in the evaluation of glucose-lowering drugs in which macrovascular complications should be used as the primary outcome for quantifying the benefit of the drugs.
There are some limitations in this systematic review. First, participants in trials and some cohort studies may not fully represent the general population of those with T2DM. But we have not found any good reasons that more representative populations would have a smaller difference between the two types of vascular complications. Second, a fraction of T2DM patients in this review already have microvascular or macrovascular complications at baseline and could not be excluded in analysis, which may bias the comparison but is unlikely to qualitatively reverse the risk ratio between these two types of complications[49,50].
CONCLUSION
Patients with T2DM are much more likely to develop MACEs than SMICs. This suggests by taking more serious consequences and higher incidence into consideration, macrovascular complications deserve more emphasis in developing the diagnostic criteria of type 2 diabetes mellitus and in evaluating the efficacy of antidiabetic drugs.
ARTICLE HIGHLIGHTS
Research background
Type 2 diabetes mellitus (T2DM) causes both macrovascular and microvascular complications. However, currently, selection of glycemic measures and their thresholds to diagnose T2DM, and efficacy outcomes in evaluation of anti-diabetic drugs is predominantly informed by the relation of T2DM to microvascular complications.
Research motivation
We can be severely mistaken by neglecting macrovascular complications in developing the diagnostic criteria of T2DM and in evaluating the efficacy of antidiabetic drugs if they also occur more commonly than microvascular complications.
Research objectives
This study aimed to compare the incidence of major cardiovascular events (MACEs) and severe microvascular complications (SMICs) in the same T2DM patients.
Research methods
The systematic review and meta-analysis with a random-effect model were conducted to combine the relative risk (RR) estimated as the incidence of MACEs divided by that of SMICs in the same T2DM patients of eligible cohort studies or trials.
Research results
Twelve studies with a total of 16 cohorts and 387376 patients were included, and the combined RR was 2.02 (95%CI: 1.46–2.79). The higher incidence of MACEs remained in various subgroup and sensitivity analyses.
Research conclusions
Patients with T2DM are much more likely to develop MACEs than SMICs.
Research perspectives
With their severity and incidence taken into consideration, macrovascular complications deserve more emphasis in developing the diagnostic criteria of T2DM and in evaluating the efficacy of anti-diabetic drugs.
 World Journal of Meta-Analysis2020年5期
World Journal of Meta-Analysis2020年5期
- World Journal of Meta-Analysis的其它文章
- Effects of antithrombotic agents on post-operative bleeding after endoscopic resection of gastrointestinal neoplasms and polyps: A systematic review and meta-analysis
- Implications of COVID-19 for inflammatory bowel disease: Opportunities and challenges amidst the pandemic
- Current trend in the diagnosis and management of malignant pheochromocytoma: Clinical and prognostic factors
- Gastrointestinal and hepatic manifestations of COVID-19 infection: Lessons for practitioners
