Role of betaine in liver disease-worth revisiting or has the die been cast?
Sandeep Mukherjee
Abstract Nonalcoholic steatohepatitis (NASH) is an important indication for liver transplantation in many Western countries due to the epidemic of obesity and insulin resistance. Unfortunately, no medication is approved for NASH and risk factor modification is often advised. Over the last decade, several clinical trials on NASH have been conducted with several ongoing and the future looks promising. Although betaine (trimethyl glycine) was evaluated for NASH, results were mixed in the clinical trials in large part due to the quality of the studies. It seems reasonable to re-evaluate betaine in clinical trials for NASH and alcoholic liver disease due to its low cost, tolerability and mechanism of action.
Key Words: Betaine; Obesity; Insulin resistance; Nonalcoholic steatohepatitis; Cirrhosis; S-adenosyl homocysteine; S-adenosyl methionine
INTRODUCTION
Betaine (or trimethy glycine) is a naturally occurring dietary compound which appears to have a beneficial effect in studies on both alcoholic steatohepatitis (ASH) and nonalcoholic steatohepatitis (NASH). It is also synthesized in the liver by the oxidation of dietary choline and common causes of betaine deficiency are often related to malnutrition from conditions such as chronic alcoholism[1]. Although the mechanisms of its actions are complex, betaine is believed to reverse inflammation, hepatic steatosis and fibrosis by several mechanisms: (1) Acting as a methyl donor for the conversion of homocysteine to methionine during alcohol exposure or in the presence of vitamin B12 and folate deficiency, all of which inhibit methionine synthetase activity; (2) Methylating phosphatidylethanolamine to phosphatidylcholineviathe Kennedy pathway (an important route in the synthesis of very low density lipoproteins prior to hepatic export); and (3) Restoration of hepatic mitochondrial glutathione and Sadenosyl methionine (SAM): S-adenosyl homocysteine ratios which reduce hepatic oxidative stress and reverse inflammation, hepatic steatosis and fibrosis in experimental and clinical studies[2,3]. As one of betaine’s principal actions is to act as a methyl donor, a diet which may be rich in carbohydrates but deficient in choline or betaine will lead to hypomethylation of homocysteine and phosphatidylethanolamine resulting in hepatic steatosis and inflammation. This was demonstrated in an elegant case-control study in which betaine levels were significantly decreased in NASH patients in contrast to patients with nonalcoholic fatty liver disease (NAFLD)[4]. In addition, mutations in mitochondrial dimethyglycine dehydrogenase, an enzyme involved in choline metabolism, were significantly associated with patients who had more advanced liver disease.
Despite these encouraging findings in multiple pre-clinical studies, betaine has not been extensively investigated in large randomized studies for the treatment of nonalcoholic or alcoholic liver disease. Since 2000, only four clinical trials have evaluated betaine for the treatment or NASH but due to limitations with study design, definitive conclusions on the impact of betaine on NASH should not be made (Table 1). For example, the first study by Miglioet al[5]did not use histopathology to diagnose NASH and thus no conclusions could be made. The second small case series of ten patients by Abdelmaleket al[6]reported biochemical and histological improvement although three patients did not complete the study. This led to a larger, randomized placebo-controlled trial by the same investigator in which 35 patients were randomized to 20 g of anhydrous betainevsplacebo for 1 year[7]. The primary aim of the study was to assess the impact of betaine on liver function tests and the secondary aim was to determine its effect on hepatic histology according to the Brunt criteria. The investigators reported betaine had no impact on aminotransferases and in addition, no change in hepatic fibrosis was noted during the study. Fewer betaineexposed patientsvsplacebo had an improvement in steatosis by more than 1 point (29%vs61%,P< 0.01). Although these findings were disappointing, there were several limitations in this study, most salient of which was the high drop-out rate which was attributed to side effects. Interestingly, betaine is now available in both anhydrous form (administered in a solution) or capsules and administration of either a lower dose of betaine anhydrous or capsules may have reduced side effects and improved compliance. This study was also only one year in duration and it would seem unlikely that reversing or improving histology in a disease with an insidious onset and which takes years to develop would occur during such a short space of time. This is now reflected by the current state of clinical trials in NASH which are now several years in duration. The most recent study of betaine in NASH was a case series of 35 patients with histologically confirmed NASH of whom the majority of patients showed stability of disease progression or improvement in hepatic histology after one year of treatment[8]. However, this study was limited by the absence of a control arm.
A prospective, unblinded randomized study of betaine is currently in progress in diabetic and non-diabetic patients with a clinical diagnosis of NAFLD (based on risk factors such as obesity and insulin resistance and the exclusion of other liver diseases) and raised liver tests[9]. In this 24-wk study, patients will be prescribed 4 g of betaine per day and after 4 wk will be randomized to either continue the same dose or increase to 8 g per day with the primary aim being comparing liver tests at weeks 12 compared to baseline using the pairedttest. However, potential foreseeable limitations of this study include lack of histological confirmation or use of non-invasive markers of steatosis or fibrosis which have gained popularity in recent clinical trials as an effective substitute for liver biopsies. The duration of this study may also be of insufficient duration to determine any impact of betaine on the primary outcome. Finally, it remains unclear what the ideal dose of oral betaine should be for clinical trials in fattyliver disease as discussed above as previous studies have used significantly larger doses. It therefore remains unclear if the study findings will change management of this disease due to limitations in study design but add to the literature without any meaningful impact.
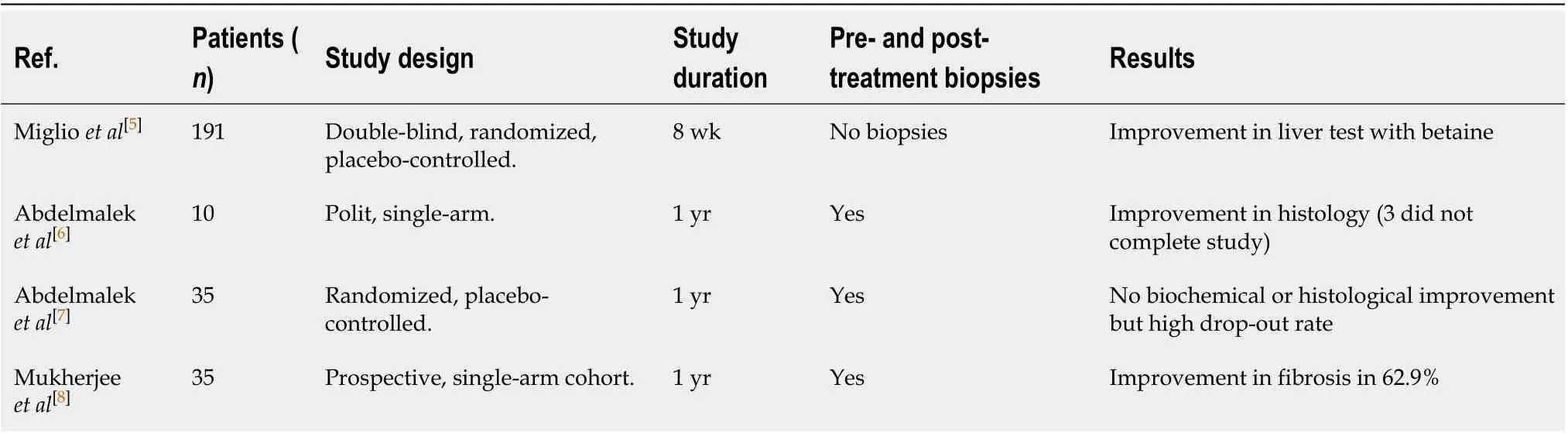
Table 1 Clinical trials of betaine for nonalcoholic steatohepatitis
Although several studies of betaine have been performed in pre-clinical (animal) studies, only SAM has been evaluated in patients with alcoholic liver disease[10,11]. In the first randomized, double-blind, placebo-controlled study, SAM improved survival and/or delayed listing for liver transplantation in 123 patients with alcoholic cirrhosis[12]. This may have been due to elevated levels of hepatic glutathione, an important antioxidant derived from homocysteine metabolism, which neutralizes free radicals and prevents cell injury. Elevated glutathione levels were also was reported in a second study of SAM in patient with alcoholic liver disease[13].
Although ASH and NASH are two different diseases, they share many features which include but are not limited to hepatic steatosis, mitochondrial dysfunction, endoplasmic reticular stress, gene dysregulation in lipid metabolism and excess proinflammatory cytokines[14]. Several of these functional and histological abnormalities are ameliorated with betaine supplementation in animal studies. For example, in well-established animal models of NAFLD, betaine supplementation attenuates the high-fat, diet-induced stress response in adipose tissue and improves both insulin sensitivity and adipokine synthesis as demonstrated by activation of hepatic adenosine monophosphate-activated protein kinase and inhibition ofde novolipogenesis[15]. In alcoholic liver disease where methionine synthetase activity is depressed, methionine and SAM levels are maintained by betaine supplementation which is activated by homocysteine in the presence of betaine homocysteine methionine methytransferase. An additional mechanism for betaine’s protective effects in alcoholic liver disease may be due to nicotinamide adenine nucleotide synthesis by the methylation of norepinephrine to epinephrine by phenylethanolamine N methyl transferase. Although this study has not been performed in human subjects, the author suggested supplementing alcoholic beverages with betaine may prevent alcoholic liver disease[16].
CONCLUSION
The interest in betaine supplementation for ASH and NASH continues to evolve and should be re-evaluated in well-designed studies. Betaine has many properties that render it ideal for clinical trials for both of these conditions which are prevalent in both developed and developing countries where cost is a factor-betaine is naturally occurring, well tolerated and inexpensive. The plethora of clinical trials on NASH should not diminish the potential value of betaine which requires re-evaluation in a large, well-designed randomized trial of adequate duration. However, NASH is also prevalent in patients with human immune deficiency virus (HIV) disease who appear to have more aggressive disease than non-HIV positive patients but are often excluded from clinical trials due to their HIV status or concerns with drug interactions[17]. Betaine should be evaluated in this population of vulnerable patients and in those with alcoholic liver disease in whom histological improvement has even been described after liver transplantation[18].
 World Journal of Gastroenterology2020年38期
World Journal of Gastroenterology2020年38期
- World Journal of Gastroenterology的其它文章
- Management of an endoscopy center during the outbreak of COVID-19: Experience from West China Hospital
- Gastrointestinal complications after kidney transplantation
- Is vitamin D receptor a druggable target for non-alcoholic steatohepatitis?
- Acetyl-11-keto-β-boswellic acid inhibits proliferation and induces apoptosis of gastric cancer cells through the phosphatase and tensin homolog /Akt/ cyclooxygenase-2 signaling pathway
- Endogenous motion of liver correlates to the severity of portal hypertension
- Longitudinal decrease in platelet counts as a surrogate marker of liver fibrosis
