Multifocal gastrointestinal epithelioid angiosarcomas diagnosed by endoscopic mucosal resection: A case report
You-Wei Chen, Jie Dong, Wan-Yuan Chen, Yi-Ning Dai
Abstract
Key words: Epithelioid angiosarcoma; Gastrointestinal tract; Endoscopic mucosal resection; Polypoid lesion; Immunohistochemistry; Case report
INTRODUCTION
Epithelioid angiosarcoma is a sporadic, highly aggressive malignancy that originates from a variety of locations, most commonly from the skin and soft tissue[1]. This type of tumor occasionally occurs in the liver, spleen, ovary, breast and adrenal gland[2]. Primary gastrointestinal angiosarcoma is extremely rare[3,4]. Here, we present a case of multifocal epithelioid angiosarcomas involved in the gastrointestinal tract.
CASE PRESENTATION
Chief complaints
A previous healthy 77-year-old woman presented with a 3-mo history of melena and dizziness and was admitted to our hospital.
Physical and accessory examinations
The physical examination was unremarkable except for pale conjunctiva. Her hemoglobin level was 65 g/L. The platelet count, coagulation function, and blood biochemistry were within normal limits. The antinuclear antibody titre was 1:1000, while the anti-SSA (Ro60) antibodies were weakly positive. Autoimmune diseases were ruled out by rheumatologists because there were no related symptoms. Abdominal computed tomography angiography revealed nothing remarkable.
Endoscopy and histopathology
Gastroscopy demonstrated a centrally ulcerated haemorrhagic polypoid lesion in the gastric body (Figure 1A). Colonoscopy revealed multiple polypoid lesions with blood clots and hemorrhagic tendency in the ileocecum, ascending colon, transverse colon and sigmoid colon (Figure 1B-D). Routine endoscopic biopsies showed inflammatory infiltration in the gastric mucosa and tubular adenomas with low-grade intraepithelial neoplasia and local eosinophilic changes in the colon. Nevertheless, the pathologic findings did not conform to the endoscopic appearance of the foci. Subsequently, the lesions were resecteden blocby endoscopic mucosal resection for further diagnosis.
Microscopically, hematoxylin and eosin staining showed areas of epithelioid cells with abundant eosinophilic cytoplasm, which was morphologically similar to undifferentiated carcinoma or poorly differentiated adenocarcinoma (Figure 2). Immunohistochemical staining (Figure 3) demonstrated that the tumor cells were positive for pan-cytokeratin (AE1/AE3), CD31, CD34, EMA, vimentin and Ki67 (60% positive) and negative for hepatocytes, S100, CD117, DOG1, CD56, SYN, CgA, LCA, desmin or ALK. The final pathological diagnosis was epithelioid angiosarcoma.
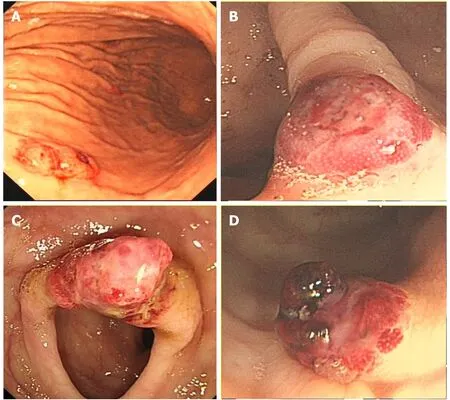
Figure 1 Endoscopy. A: Gastroscopy revealed a 0.5 cm × 0.6 cm centrally ulcerated polypoid lesion in the gastric body; B: A 0.8 cm × 0.8 cm polypoid lesion in the ascending colon; C: A 1.2 cm × 1.0 cm hyperaemic mass in the transverse colon; and D: A 0.8 cm × 0.8 cm polypoid nodule with hemorrhagic tendency and blood clots in the sigmoid colon.
Positron emission tomography/computed tomography
To determine whether distant metastasis occurred, additional F-18 uorodeoxyglucose positron emission tomography/computed tomography (PET/CT) was performed. PET/CT showed tubular hypermetabolic lesions in the colon, suggesting malignancy. Furthermore, numerous hypermetabolic hilar and mediastinal lymph nodes, as well as multiple node-like foci with active F-18 uorodeoxyglucose metabolism in the bones, were observed, revealing lymphatic and osseous metastasis (Figure 4).
FINAL DIAGNOSIS
Multifocal gastrointestinal epithelioid angiosarcomas with lymphatic and osseous metastasis.
OUTCOME AND FOLLOW-UP
The patient refused chemotherapy and died after three months due to gastrointestinal bleeding.
DISCUSSION
Angiosarcomas may arise in any part of the body, but commonly occur in skin and superficial soft tissues, with its predilection sites in the head and neck[5]. Epithelioid angiosarcoma of the gastrointestinal tract is an extremely rare neoplasm, which is only described in individual case reports and case series[6-9], with a lack of demographic morbidity data. According to literatures, vascular tumors of the stomach constitute only 0.9%-3.3% of all gastric cancers[10], while colorectal angiosarcomas represent less than 0.001% of all colorectal neoplasms[11].

Figure 2 Histopathological findings. Poorly differentiated neoplasms consisting of large cells with pleomorphic nuclei and abundant eosinophilic cytoplasm were observed. A: Haematoxylin and eosin (HE) staining section × 40; B: HE staining section (× 100); C: HE staining section (× 200); and D: HE staining section (× 400).

Figure 3 Immunohistochemical staining. A: Immunostaining for CD31; B: Immunostaining for CD34; and C: Immunostaining for pan-cytokeratin.
Epithelioid angiosarcoma is characterized by an extremely aggressive course, leading to a very poor prognosis[12]. Even for localized disease, patients without any therapy had a 0% survival rate at 2 years[5]. Due to the infiltrative nature of this neoplasm, recurrence and metastasis are frequent after surgical resection, even for localized disease. Cytotoxic chemotherapy can be effective in a subset of patients for a limited period, but metastatic angiosarcomas remain incurable and even fatal[5]. Targeted therapy with tyrosine kinase inhibitors usually resulted in significant responses, but these tumors are prone to developing resistance[5].
In most cases of gastrointestinal angiosarcoma, the symptoms are nonspecific, including abdominal pain, weight loss and anorexia. Overt bleeding with melena or hematochezia is less common. The patient in the present report had positive antinuclear antibody and anti-SSA, which might be secondary to the tumor. Nevertheless, until now, there is no evidence that the positivity of autoimmune antibodies has association with angiosarcomas. Further studies are needed to clarify their relationships.
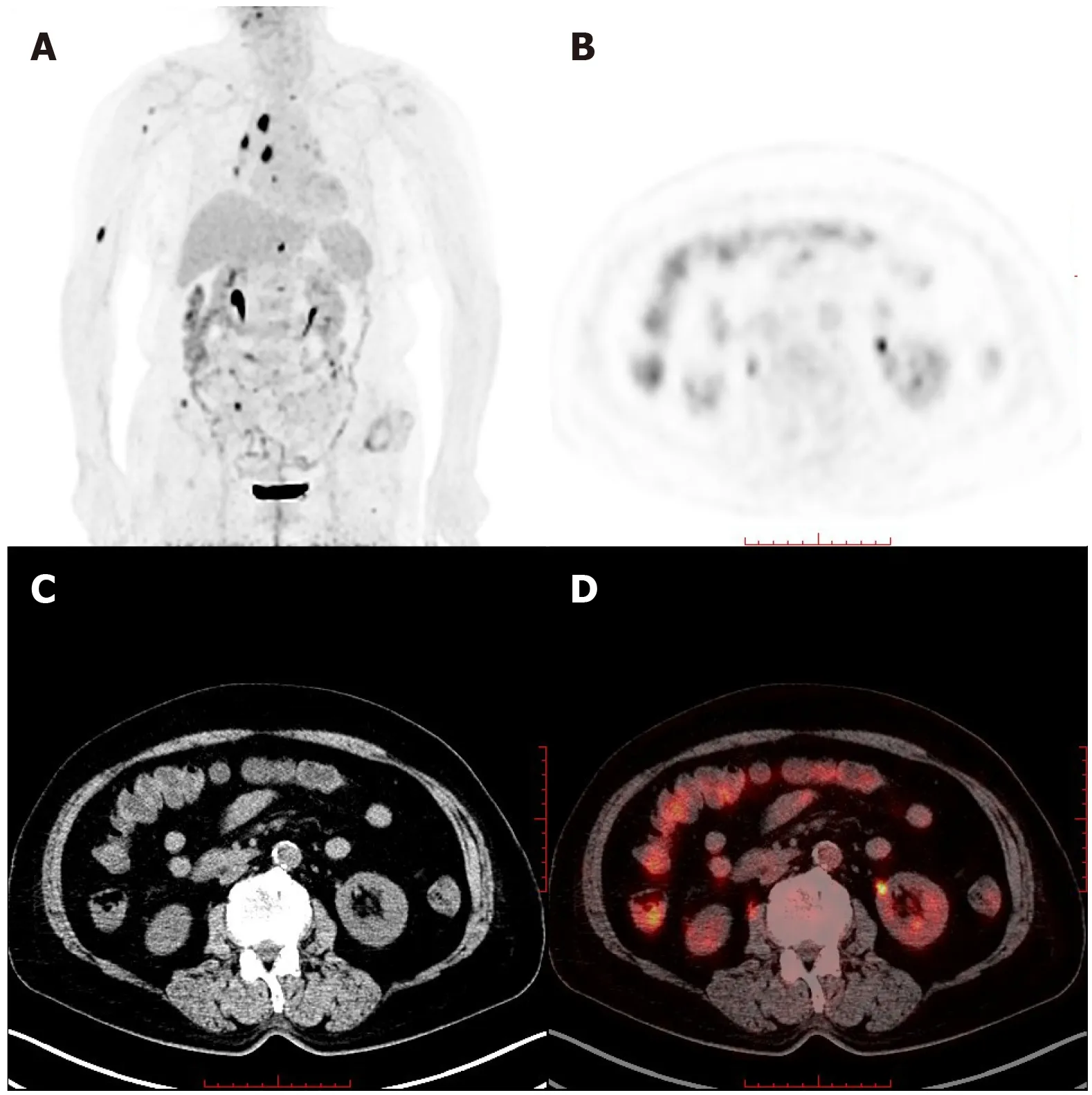
Figure 4 Whole-body maximum intensity projection 18F- fluorodeoxyglucose and positron emission tomography image. A: Remarkably increased fluorodeoxyglucose metabolism in the colon and mediastinal lymph nodes, as well as the right humerus; B: Positron emission tomography; C: Computed tomography; and D: Positron emission tomography/computed tomography in axial projection showed multiple tubular hypermetabolic lesions in the colon.
Almost all reported lesions that occurred in the gastrointestinal tract appeared endoscopically as centrally ulcerated, hemorrhagic, highly erythematous or purpuric nodules/masses[13]. Endoscopy with direct visualization and biopsy is crucial for diagnosis. However, endoscopic biopsy often obtains insufficient specimens and leads to the possibility of a missed diagnosis[14], similar to this case. It is well known that invasive carcinomas are likely to be covered by normal epithelium or intraepithelial neoplasm. Consequently, findings of the biopsy on their surface usually do not reflect the invasive components. Possible efforts to obtain additional histopathological findings must be made. In the present case,en blocendoscopic mucosal resection of the suspected lesions in the colon was satisfactory for the histopathological examination. Due to the confirmation of malignant angiosarcomas, the patient refused to have another large-scale biopsy of the gastric lesion, in which the endoscopic performance was similar and typical.
Epithelioid angiosarcoma mimics carcinoma morphologically and contains numerous vasoformative structures. Because of the high architectural and cytological variability, pathological diagnosis is difficult. Immunoreactivity for endothelial and epithelial cell markers can confirm the diagnosis. This innate characteristic of epithelioid angiosarcoma corresponds to the tendency of gastrointestinal bleeding. PET/CT has been reported to detect primary uterine and pulmonary epithelioid angiosarcoma[15,16]and is of great value in identifying metastases.
CONCLUSION
We report a case of gastrointestinal bleeding that was finally diagnosed as multifocal epithelioid angiosarcomas involved in the gastrointestinal tract. The endoscopic characteristics of the lesions were highlighted and corresponded to the propensity of gastrointestinal bleeding.En blocendoscopic mucosal resection contributed to the final histopathological diagnosis.
 World Journal of Gastroenterology2020年29期
World Journal of Gastroenterology2020年29期
- World Journal of Gastroenterology的其它文章
- Endoscopic management of gastrointestinal leaks and fistulae: What option do we have?
- Watch and wait approach in rectal cancer: Current controversies and future directions
- Evaluation of intrahepatic manifestation and distant extrahepatic disease in alveolar echinococcosis
- Multivariate predictive model for asymptomatic spontaneous bacterial peritonitis in patients with liver cirrhosis
- Clinicopathological characteristics and surgical outcomes of sarcomatoid hepatocellular carcinoma
- Patients' perspectives on smoking and inflammatory bowel disease: An online survey in collaboration with European Federation of Crohn's and Ulcerative Colitis Associations
