不同给药方式治疗ICU糖尿病酮症酸中毒的效果观察及护理
吴腾修 张月娥
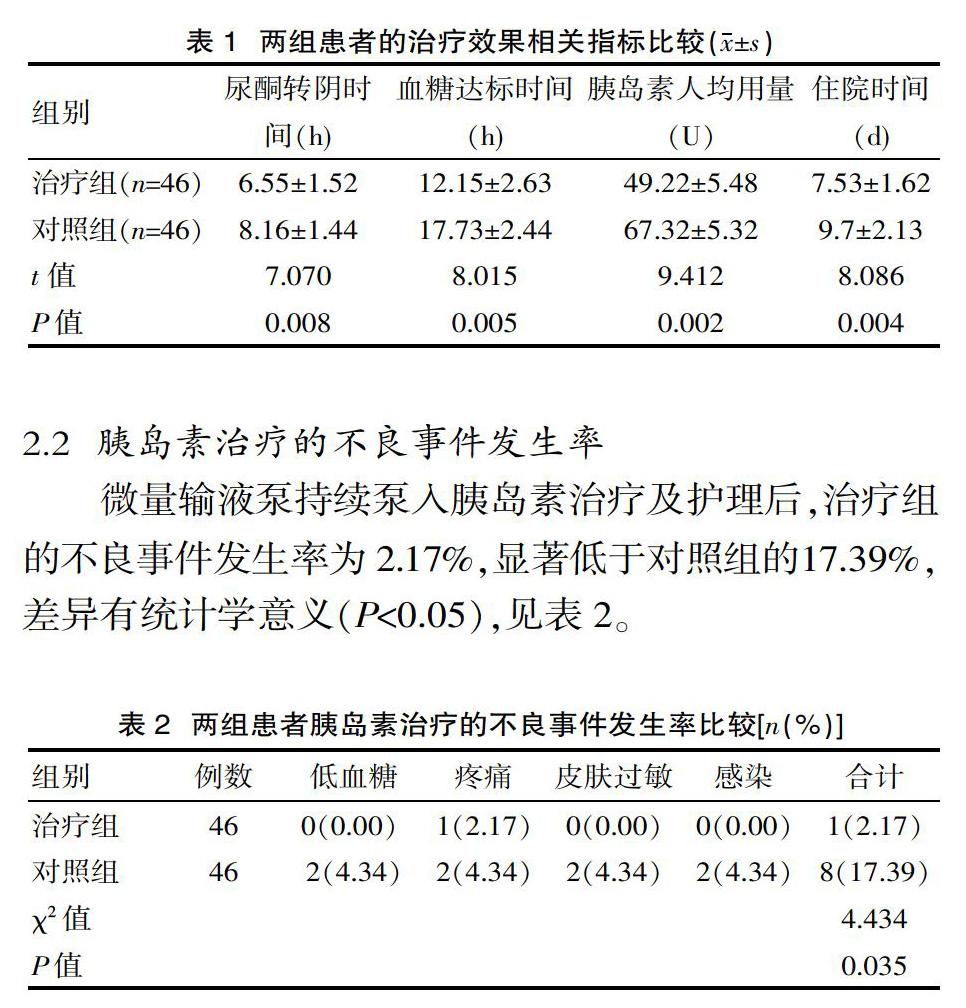
[摘要] 目的 探讨不同给药方式治疗ICU糖尿病酮症酸中毒的效果及护理措施。方法 将该院2017年8月—2019年8月接收的92例糖尿病酮症酸中毒患者根据随机数字表法分为对照组(给予多次静脉滴注小剂量胰岛素治疗及护理)与治疗组(给予微量输液泵持续泵入胰岛素治疗及护理),各46例,比较两组的治疗效果及不良事件发生情况。结果 微量输液泵持续泵入胰岛素治疗及护理后,治疗组的治疗效果相关指标均显著优于对照组(P<0.05);治疗组的不良事件发生率为2.17%,显著低于对照组的17.39%(P<0.05)。结论 微量输液泵持续泵入胰岛素治疗可作为ICU糖尿病酮症酸中毒的首选给药方式,安全性及有效性均较高。
[关键词] 不同给药方式;ICU;糖尿病酮症酸中毒;治疗效果;护理
[中图分类号] R47 [文献标识码] A [文章编号] 1672-4062(2020)09(a)-0006-03
[Abstract] Objective To explore the effects of different administration methods in the treatment of ICU diabetic ketoacidosis and nursing measures. Methods The 92 patients with diabetic ketoacidosis received in the hospital from August 2017 to August 2019 were divided into a control group (with multiple intravenous infusions of low-dose insulin therapy and care) and a treatment group (with micro-infusion pump to continuously pump insulin therapy and nursing) according to the random number table method, 46 cases in each group, compare the treatment effects and adverse events of the two groups. Results After the micro-infusion pump continues to pump insulin treatment and nursing, the treatment effect related indicators of the treatment group were significantly better than those of the control group(P<0.05); the adverse event rate of the treatment group was 2.17%, which was significantly lower than the control group's 17.39%(P<0.05). Conclusion Micro-infusion pump continuous infusion of insulin therapy can be used as the first choice for ICU diabetic ketoacidosis, with high safety and effectiveness.
[Key words] Different modes of administration; ICU; Diabetic ketoacidosis; Treatment effect; Nursing
糖尿病酮症酸中毒是一种较为严重的急性糖尿病并发症,临床特征为高血糖、高血酮、酮尿等,若治疗不及时,随着病情进展可并发急性肾衰竭、昏迷,进而威胁患者生命[1-2]。糖尿病酮症酸中毒的发生机制较复杂,临床上针对此病一般在常规对症治疗基础上辅以予胰岛素补充治疗,但其治疗效果除了与胰岛素给药方式有关外,还与患者治疗期间的饮食习惯、行为方式等密切相关[3-4]。因此,选择合适的胰岛素给药方式并辅以有效护理干预至关重要。该次研究选择该院ICU病房2017年8月—2019年8月接收的46例糖尿病酮症酸中毒患者给予微量输液泵持续泵入胰岛素治疗及护理,效果显著,现报道如下。
1 資料与方法
1.1 一般资料
选取该院ICU病房接收的92例糖尿病酮症酸中毒患者。纳入标准:符合糖尿病酮症酸中毒的临床诊断标准[5];首次发病;家属对研究知情同意。排除标准:胰岛素应用禁忌证;合并有传染性疾病、免疫系统缺陷疾病;严重心肝肾功能障碍;精神疾病。将92例患者按照随机数字表达法均分为对照组和治疗组,每组46例。对照组中男24例,女22例;年龄52~86岁,平均(69.34±5.29)岁;糖尿病病程3~17年,平均(8.63±1.25)年;其中Ⅰ型糖尿病22例,2型糖尿病24例。治疗组中男25例,女21例;年龄51~85岁,平均(69.42±5.18)岁;糖尿病病程3~18年,平均(8.61±1.22)年;其中Ⅰ型糖尿病23例,2型糖尿病23例。两组的临床资料相似,差异无统计学意义(P>0.05)。具有可比性。
1.2 方法
所有患者入院后均给予补液、抗炎、扩容及纠正水电解质紊乱等常规对症治疗。对照组在常规对症治疗基础上又给予多次静脉滴注小剂量胰岛素治疗,静脉滴注速度为0.1 U/(kg·h),待患者酸中毒得到有效纠正后再改为三餐前皮下注射短效胰岛素及睡前皮下注射长效胰岛素。治疗组在常规对症治疗基础上又给予微量输液泵持续泵入胰岛素治疗,起始泵入速度为0.05~0.1 U/(kg·h),其中3/5是基础量,2/5是餐前负荷量,待患者酸中毒得到纠正后将用药剂量改为0.6~1.2 U/h继续给药。两组患者采用胰岛素治疗期间均辅以综合护理干预,具体如下。

