妊娠期糖尿病子代发生低血糖的影响因素分析
钟俊炎
【摘要】 目的:探讨妊娠期糖尿病子代发生低血糖的影响因素。方法:采用病例对照研究设计,收集2018年1月1日-2019年6月1日南方医科大学附属深圳妇幼保健院新生儿科收治的出生胎龄>34周诊断新生儿低血糖且其母亲患有妊娠期糖尿病的患儿共128例为病例组,同期住院的未诊断新生儿低血糖但母亲患有妊娠期糖尿病的新生儿128例为对照组。收集纳入病例与母亲的临床资料、生后24 h内血小板参数。采用秩和检验、字2检验和logistic回归分析各种因素对妊娠期糖尿病子代发生低血糖的影响意义。结果:单因素分析显示,两组双胎妊娠、初产妇、顺产、孕期血糖控制不佳以及妊娠期高血压疾病比例、出生胎龄、出生体重、入院时血气分析pH值、血小板计数、平均血小板体积比较,差异均有统计学意义(P<0.05)。多因素回归分析结果显示,双胎妊娠[OR=5.225,95%CI(1.070,25.527)]、孕期血糖控制不佳[OR=11.751,95%CI(3.775,36.579)]、妊娠期高血壓疾病[OR=8.707,95%CI(1.875,40.439)]、平均血小板体积增高[OR=1.519,95%CI(1.020,2.257)]均是妊娠期糖尿病子代发生低血糖的危险因素,而顺产[OR=0.480,95%CI(0.242,0.953)是其保护因素。结论:双胎妊娠、孕期血糖控制不佳、妊娠期高血压疾病、平均血小板体积增高均是妊娠期糖尿病子代发生低血糖的危险因素,而顺产是其保护因素。
【关键词】 妊娠期糖尿病 子代 低血糖 影响因素
[Abstract] Objective: To explore the influencing factors of hypoglycemia in gestational diabetes mellitus offspring. Method: This was a retrospective case-control study. 128 newborns (gestational age>34 weeks) diagnosed hypoglycemia born to gestational diabetes mellitus mothers were selected as case group, and 128 newborns (gestational age>34 weeks) without hypoglycemia born to gestational diabetes mellitus mothers were selected during the same period as the control group. All the newborns were hospitalized in the Neonatology Department of Shenzhen Maternity and Child Healthcare Hospital from January 1, 2018 to June 1, 2019. The clinical data and the platelet-related parameters within 24 h of admission of the included cases were collected. Mann-Whitney U test, Chi-square and multivariate logistic regression were used to analyze the influencing factors of hypoglycemia in newborns born to gestational diabetes mellitus mothers. Result: Univariate analysis showed: the differences of proportion of twin pregnancy, primipara, and vaginal delivery, poor glycemic control and hypertension during pregnancy of two groups were statistically significant (P<0.05). In addition, the differences of gestational age, birth weight, pH value in blood gas analysis, platelet count and mean platelet volume of two groups were statistically significant (P<0.05). Multivariate regression analysis showed twin pregnancy [OR=5.225, 95%CI (1.070, 25.527)], poor glycemic control during pregnancy [OR=11.751, 95%CI (3.775, 36.579)], hypertension during pregnancy [OR=8.707, 95%CI (1.875, 40.439) and high mean platelet volume (MPV) [OR=1.519, 95%CI (1.020, 2.257)] were independent risks factor for hypoglycemia. Whereas vaginal delivery [OR=0.480, 95%CI (0.242, 0.953)] was a protective factor for hypoglycemia. Conclusion: Twin pregnancy, poor glycemic control during pregnancy, hypertensive disorder complicating pregnancy, high mean platelet volume are independent risk factors for gestational diabetes mellitus offspring, and vaginal delivery is an protective factor.
[Key words] Gestational diabetes mellitus Offspring Hypoglycemia Influencing factors
First-authors address: Affiliated Shenzhen Maternity & Child Healthcare Hospital, Southern Medical University, Shenzhen 518028, China
doi:10.3969/j.issn.1674-4985.2020.24.012
妊娠期糖尿病(gestational diabetes mellitus,GDM)是妊娠常见合并癥,也是威胁母婴健康的重要疾病,全球发病率高达16.2%[1],国际糖尿病联盟报道2017年有184万新生儿受到母体孕期高血糖的影响,占总新生儿的13.9%[2]。妊娠合并糖尿病后出生的婴儿主要问题之一是低血糖,因为新生儿低血糖有潜在的不良神经发育结果,因此预防、及时识别和治疗新生儿低血糖是非常重要的。本研究探讨妊娠期糖尿病子代发生低血糖的影响因素,寻找发生低血糖的高危因素和预防低血糖的有利因素。现报道如下。
1 资料与方法
1.1 一般资料 选择2018年1月1日-2019年6月1日南方医科大学附属深圳市妇幼保健院新生儿科收治的出生胎龄>34周,诊断新生儿低血糖,且其母亲患有妊娠期糖尿病的患儿,共128例,为病例组。纳入标准:研究时期内本科室收治的出生胎龄>34周,母亲患有妊娠期糖尿病的患儿。排除标准:合并其他先天性代谢异常疾病;合并先天畸形或发育异常;孕期未规律产检,资料不全。随机抽取同期住院的未诊断新生儿低血糖但母亲患有妊娠期糖尿病的新生儿128例,为对照组。该研究已经伦理学委员会批准。
1.2 方法
1.2.1 诊断方法 (1)GDM:根据2014年《妊娠合并糖尿病诊治指南》[3];75 g葡萄糖口服耐量试验(oral glucose tolerance test,OGTT),服糖前,服糖后1、2 h静脉血糖界值分别为5.1、10.0、8.5 mmol/L,有任意一项达到或超过上述值诊断为GDM。(2)新生儿低血糖:不论胎龄和日龄,新生儿出生后任一时点血糖值<2.2 mmol/L诊断为新生儿低血糖,<2.6 mmol/L为临界低血糖[4]。(3)孕期血糖控制不佳:GDM血糖控制的目标为空腹血糖≤5.0 mmol/L、餐后1 h血糖≤7.2~7.8 mmol/L、餐后2 h血糖≤6.7 mmol/L,超出此目标为孕期血糖控制不佳[5]。(4)胰岛素基础分泌高峰期[6]:1 d中,生理性胰岛素分泌第一个高峰自凌晨3时开始增高,5-6时达高峰,7时逐渐下降,第二个高峰自15时开始增高,16-17时达高峰。
1.2.2 分析变量 一般临床资料包括性别、单双胎、分娩方式、初产妇、产妇年龄、血糖控制情况、是否需要药物控制血糖、妊娠期高血压疾病、是否在胰岛素基础分泌高峰期出生、是否母婴早接触早吸吮、生后窒息、出生胎龄、出生体重、巨大儿、早发型败血症、湿肺、入院时血糖、血气分析pH值、红细胞计数、血小板计数、血小板压积、平均血小板体积、血小板分布宽度等。
1.3 统计学处理 采用SPSS 19.0软件对所得数据进行统计分析,非正态分布计量资料以M(P25,P75)表示,组间比较采用Mann-Whitney U检验;计数资料采用频数和率进行描述,组间比较采用字2检验;采用logistic回归模型分析低血糖发生的独立影响因素。以P<0.05为差异有统计学意义。
2 结果
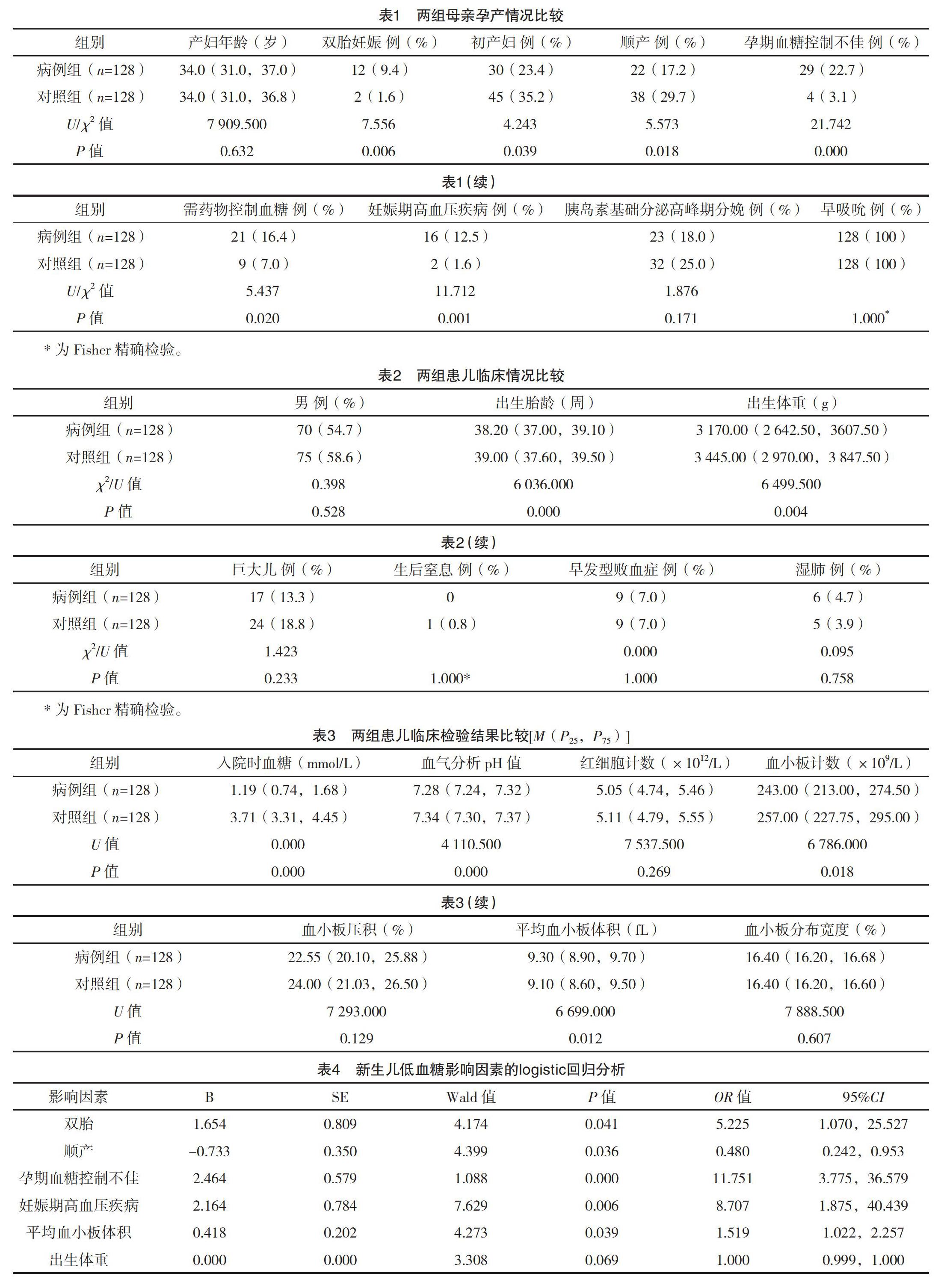
2.1 一般情况比较 两组母亲孕产情况:双胎妊娠、初产妇、顺产、孕期血糖控制不佳、需药物控制血糖、妊娠期高血压疾病比例,差异均有统计学意义(P<0.05),见表1;两组患儿临床情况:出生胎龄、出生体重比较,差异均有统计学意义(P<0.05),见表2;两组患儿入院时临床检验:入院时血气分析pH值、血小板计数、平均血小板体积比较,差异均有统计学意义(P<0.05),见表3。
2.2 多因素logistic回归分析 将单因素分析筛选差异有统计学意义的影响因素作为自变量,以是否发生低血糖作为因变量,构建logistic回归模型。结果显示,双胎妊娠[OR=5.225,95%CI(1.070,25.527)]、孕期血糖控制不佳[OR=11.751,95%CI(3.775,36.579)、妊娠期高血压疾病[OR=8.707,95%CI(1.875,40.439)]、平均血小板体积增高[OR=1.519,95%CI(1.020,2.257)]均是妊娠期糖尿病子代发生低血糖的独立危险因素,而顺产[OR=0.480,95%CI(0.242,0.953)]是其保护因素,见表4。
3 讨论
GDM是怀孕期间最常见的代谢紊乱,发病率有逐渐增高的趋势。低血糖是GDM子代常见的并发症,鉴于持续或反复的低血糖可造成新生儿神经系统不可逆的损害,临床上已采取了一些措施预防和治疗新生儿低血糖。研究发现母婴皮肤早接触可降低新生儿低血糖的发生率[7-8]。本研究中所有新生儿均进行母婴皮肤早接触,但除此之外还有其他因素可影响GDM子代的血糖水平。
本研究结果显示,双胎是其发生低血糖的高危因素,与国外研究报道结果一致[9],考虑原因为双胎的营养需求较单胎大,造成胎儿的糖原储备减少,出生后容易出现低血糖;孕妇血糖控住不佳的情况下,母体异常增高的血糖通过胎盘屏障进入胎儿体内,刺激胎儿胰岛细胞分泌胰岛素,而胎儿出生后不能再得到来自母体的血糖供应,极易引起低血糖[10];GDM可导致全身的血管病变,使小血管内皮增厚,管腔狭窄,而妊娠期高血压疾病的病理生理基础是孕妇全身小血管痉挛,共同作用使得胎盘功能减退,胎儿营养供应受影响,这也是出生后新生儿发生低血糖的高危因素,与国外研究结果一致[11]。
本研究分析提示順产是GDM子代低血糖的保护因素,在单因素分析时也提示对照组初产妇比例高于病例组(P<0.05)。考虑原因为:初产妇往往总产程较长,而分娩对于孕妇和胎儿来说均是一个应激的过程,在此期间皮质激素分泌增高,有利于血糖的维持,相比而言,剖宫产前胎儿在宫内处于高血糖、高胰岛素环境中,术前禁食,若术中未予含糖的溶液维持,并且胎儿突然脱离高血糖环境,也增加了低血糖发生率。
血小板平均体积(MPV)是血小板平均大小和活性的指标。Iyidir等[12]研究了MPV与GDM中代谢参数的相关性,分析了30例GDM妇女和38例体质指数匹配的健康妊娠妇女作为对照,记录妊娠中晚期和产后6~12个月MPV和血小板计数,GDM组孕中晚期MPV显著增高,GDM组产后MPV显著下降。空腹血浆葡萄糖水平和曲线下的葡萄糖面积与妊娠中晚期MPV呈正相关。纳入19项研究的荟萃分析也显示:GDM患者伴有MPV升高,MPV可能是GDM预测指标[13]。同理,胎儿宫内高血糖水平可能提示着高MPV,在相对胰岛素过剩的情况下,出生后血糖供应中断,容易导致新生儿低血糖。
在单因素分析中,病例组入院时血气分析pH值低于对照组(P<0.05),已有研究发现GDM子代血糖值与脐带血pH值在一定程度上呈正相关[14],考虑与机体酸过剩影响糖代谢有关。此外,病例组需药物控制血糖(包括口服降糖药、胰岛素)的比例高于对照组(P<0.05),与既往文献[15-16]研究结果相符,但可能由于样本量的原因未进入回归模型。既往文献[17-18]报道母亲肥胖和体质指数过高被认为是新生儿低血糖的预测指标,此外新生儿体温的维持等也是低血糖应该关注的问题。由于本研究为回顾性研究,期望在以后的研究中增加样本量与完善各相关监测指标进一步明确关于GDM子代发生低血糖的影响因素。
综上所述,双胎妊娠、孕期血糖控制不佳、妊娠期高血压疾病、平均血小板体积增高是妊娠期糖尿病子代发生低血糖的危险因素,顺产则是保护因素。低血糖对新生儿生长发育的负面影响是值得关注的。因此,产儿科临床医师应加强产妇产前健康保健,规避危险因素,控制孕妇血糖波动,以预防新生儿低血糖。
参考文献
[1]钱婷婷,陈丹青.妊娠期糖尿病高危因素的研究进展[J].国际妇产科学杂志,2019,46(10):494-498.
[2] Cho N H,Shaw J E,Karuranga S,et al.IDF Diabetes Atlas:Global estimates of diabetes prevalence for 2017 and projections for 2045[J].Diabetes Research and Clinical Practice,2018,138:271-281.
[3]杨慧霞.妊娠合并糖尿病诊治指南(2014版)[C].中华医学会杂志社指南与进展巡讲(产科)暨第四届两江母胎医学论坛,2014.
[4] Persson M,Shah P S,Rusconi F,et al.Association of Maternal Diabetes With Neonatal Outcomes of Very Preterm and Very Low-Birth-Weight Infants:An International Cohort Study[J].JAMA pediatrics,2018,172(9):867-875.
[5] Berger H,Gagnon R,Sermer M,et al.Diabetes in Pregnancy[J].Journal of Obstetrics and Gynaecology,2016,38(7):667-679.
[6] Matteucci E,Giampietro O,Covolan V,et al.Insulin administration:present strategies and future directions for a noninvasive(possibly more physiological) delivery[J].Drug Design,Development and Therapy,2015,9:3109-3118.
[7]林蓉金,金调芬,孙欣悦.母婴皮肤早接触对妊娠期糖尿病产妇新生儿血糖的影响[J].中国妇幼保健,2019,34(11):2507-2509.
[8] Dalsgaard B T,Rodrigo-Domingo M,Kronborg H,et al.Breastfeeding and skin-to-skin contact as non-pharmacological prevention of neonatal hypoglycemia in infants born to women with gestational diabetes;a Danish quasi-experimental study[J].Sexual & Reproductive Healthcare,2019,19:1-8.
[9] Sheehan A C M,Umstad M P,Cole S,et al.Does Gestational Diabetes Cause Additional Risk in Twin Pregnancy?[J].Twin Research and Human Genetics,2019,22(1):62-69.
[10] Yamamoto J M,Donovan L E,Mohammad K,et al.Severe neonatal hypoglycaemia and intrapartum glycaemic control in pregnancies complicated by type 1,type 2 and gestational diabetes[J].Diabetic Medicine,2020,37(1):138-146.
[11] Dassios T,Greenough A,Leontiadi S,et al.Admissions for hypoglycaemia after 35 weeks of gestation: perinatal predictors of cost of stay[J].The Journal of Maternal-fetal & Neonatal Medicine,2019,32(3):448-454.
[12] Iyidir O T,Degertekin C K,Yilmaz B A,et al.Elevated mean platelet volume is associated with gestational diabetes mellitus[J].Gynecological Endocrinology,2014,30(9):640-643.
[13] Zhou Z,Chen H,Sun M,et al.Mean Platelet Volume and Gestational Diabetes Mellitus:A Systematic Review and Meta-Analysis[J].Journal of Diabetes Research,2018:1985026.
[14] Flores-le Roux J A,Sagarra E,Benaiges D,et al.A prospective evaluation of neonatal hypoglycaemia ininfants of women with gestational diabetes mellitus[J].Diabetes Research and Clinical Practice,2012,97(2):217-222.
[15] Maayan-Metzger A,Lubin D,Kuint J.Hypoglycemia rates in the first days of life among term infants born to diabetic mothers[J].Neonatology,2009,96(2):80-85.
[16] Ramos G A,Hanley A A,Aguayo J,et al.Neonatal chemical hypoglycemia in newborns from pregnancies complicated by type 2 and gestational diabetes mellitus-the importance of neonatal ponderal index[J].The Journal of Maternal-fetal & Neonatal Medicine,2012,25(3):267-271.
[17] Cremona A,Saunders J,Cotter A,et al.Maternal obesity and degree of glucose intolerance on neonatal hypoglycaemia and birth weight:a retrospective observational cohort study in women with gestational diabetes mellitus[J].European Journal of Pediatric,2019,179:653-660.
[18] Garcia-Patterson A,Aulinas A,Maria M A,et al.Maternal body mass index is a predictor of neonatal hypoglycemia in gestational diabetes mellitus[J].The Journal of Clinical Endocrinology and Metabolism,2012,97(5):1623-1628.
(收稿日期:2020-05-14) (本文編辑:程旭然)

