Analysis of two cases of patent ductus arteriosus ligation in preterm identical twins and literature review
Xiang Cao, Xiao-Ding Chen, Ling Yang, Ren-Wei Chen, Yan Li, Ze-Lai Mo, Wei Xiang
1.Neonatology Department,Hainan Women and Children’s Medical Center,Children’s Hospital of Hainan Medical University,Haikou,Hainan 570206,China
2.Cardio-Thoracic Surgery Department,Hainan Women and Children’s Medical Center,Children’s Hospital of Hainan Medical University,Haikou,Hainan 570206,China 3.Anesthesiology Department,Hainan Women and Children’s Medical Center,Children’s Hospital of Hainan Medical University, Haikou,Hainan 570206,China 4.Ultrasound Imaging Department,Hainan Women and Children’s Medical Center,Children’s Hospital of Hainan Medical University, Haikou,Hainan 570206,China
5.Key Laboratory of Tropical Translational Medicine, Ministry of Education, Hainan Medical University,Haikou,Hainan 571199,China
Keywords:Identical twins Preterm infant Patent ductus arteriosus ligation
ABSTRACT Objective: To investigate the timing and effect of surgical ligation in the treatment of patent ductus arteriosus(PDA) in preterm identical twins. Methods: Retrospective analysis was made on the treatment of 2 cases of preterm twins with hemodynamic significant PDA(hsPDA) with corresponding clinical manifestation in our neonatology department, and literatures of PDA ligation for preterm twins were retrieved. Results: These 2 cases were naturally conceived monochorionic diamniotic twins, with gestational age 30+2 weeks, birth weight was 1510g and 780g for larger twin and smaller twin, with birth weight discordance 48.3%.They both developed hsPDA with corresponding clinical manifestation, series Echocardiography showed evidence of left to right shunting and cardiac insufficiency which were left atrial and ventricular enlargement, large PDA(2.8~3.5mm), failed two courses of ibuprofen, N-terminal pro-brain natriuretic peptide level increased significantly, finally received surgical ligation with significant clinical improvement and no related complications.12 cases were found from literature search, including our 2 cases, of these,2 died,9 were cured and 1 improved significantly.Among 6 cases whose detailed information were available,4 infants were identical twins,2 unknown. Conclusions: Preterm identical twins have the same genetic basis, the possibility of PDA ligation for both the larger twin and smaller twin should be alerted if the gestaional age is small and birth weight discordance is above 30%.If preterm twins have hsPDA who may fail ibuprofen treatment, surgical ligation should be considered early, and it is safe and effective.
1. Introduction
Patent ductus arteriosus(PDA) is a common morbidity in preterm infants,which can be divided into hemodynamically insignificant PDA and hemodynamically significant PDA(hsPDA) according to hemodynamic status[1]. Prolonged patency is associated with numerous adverse outcomes,including prolongation of assisted ventilation and increased rates of mortality and morbidity,such as bronchopulmonary dysplasia,pulmonary hemorrhage,necrotizing enterocolitis,impaired renal function,intraventricular hemorrhage,periventricular leukomalacia,and cerebral palsy[2,3].PDA is more common in twins than in singletons[4].For those who may fail to drug therapy or if contraindications exist,surgical ligation can effectively decrease mortality and complications rates,improve neurodevelopmental outcome[5,6,7].However,data about risk factors for surgical ligation in preterm twin neonates especially identical twins,whether need surgical intervention and the timing for ligation,is lacking.We present 2 cases of preterm identical twins with hsPDA,and searched case reports about PDA ligation among preterm twin neonates,aim to provide clinical reference for the timing of surgical ligation of preterm twin neonates with hsPDA.
2. Patient data
2.1 Clinical data
Two infants were both males,with gestational age 30 weeks and 2 days,conceived naturally monochorionic diamnionic twins,delivered by C-section for fetal distress,clear amniotic fluid,no birth asphyxia,birthweight were 780g and 1510g for the smaller twin and larger twin,respectively,with discordance of 48.3%,were admitted to NICU for respiratory distress,both received surfactant and non-invasive ventilation.Echocardiography suggested PDA,with hemodynamically significant clinical manifestations,such as tach ypnea,dyspnea,retractions,need prolonged ventilation support(18 days for smaller twin on non-invasive ventilation from birth until ligation, 38 days for larger twin on non-invasive ventilation from birth until ligation),tachycardia(HR range 170-195bpm),persistent murmur at the second intercostal of left margin sternum, hypotension(particularly diastolic, 75/36mmHg,74/32mmHg,respectively),widened pulse pressure(39mmHg and 42mmHg, >25 mmHg,respectively),larger twin showed severe acidosis(Lac 7.1mmol/L、BE -7.2mmol/L),series Echocardiography showed evidence of left to right shunting and cardiac insufficiency which were left atrial and ventricular enlargement, large PDA(2.8~3.5mm), failed two courses of ibuprofen(the 1st course regimen 10mg/kg followed by 5mg/kg,5mg/kg Q24h, the 2nd course regimen 20mg/kg followed by 10mg/kg,10mg/kg Q24h,smaller twin presented oligouria after the 2nddose of the 2ndcourse,with urine output 1ml/kg/h,urine analysis was normal,serum creatinine 48umol/L,team considered it was associated with side effect of ibuprofen,the 3rddose was discontinued and urine output returned to normal,4.3ml/kg/h),N-terminal pro-brain natriuretic peptide level increased significantly(both above 25000pg/ml,normal range for neonates was 263~5918 pg/ml),finally received surgical ligation with significant clinical improvement and no related complications.Follow up Echocardiography showed ductus arteriosus closed and normal size of the left ventricle and left atrium,repeated NT-proBNP levels 3 days post-ligation decreased significantly(smaller twin 15114pg/ml,larger twin 11641pg/ml).Clinical symptoms improved significantly,smaller twin was extubated to NIPPV at day of life 29,switched to HHHFNC at day of life 58,larger twin was extubated to non-invasive ventilation at day of life 44,off oxygen at day of life 46,discharged home at day of life 71.Series head ultrasound for the twins during hospital stay did not show evidence of intraventricular hemorrhage or periventricular leukomalacia.Mutiple retinopathy of prematurity screens showed negative.
2.2 Literature
A comprehensive literature search was performed using MEDLINE, including in process and other non-indexed citations (1966 to July, 2020), using the search strategy ‘preterm’ AND ‘twins’ OR ‘multiple births’ AND ‘patent ductus arteriosus ligation’,2 articles were retrieved[8,9].One of them was Japanese article which reported an extremely premature triplets who received PDA ligation,only abstract available without detailed information[9].Chinese literature search was performed using CNKI and Wanfang Database,from 1979 to July 2020.Take CNKI for example, using the search strategy ‘preterm’ AND ‘twins’ OR ‘multiple births’ AND ‘patent ductus arteriosus ligation’,no articles were retrieved, using the search strategy ‘preterm’ OR ‘low birthweight infants’ AND ‘patent ductus arteriosus ligation’, ‘preterm’ OR ‘low birthweight infants’ AND ‘patent ductus arteriosus’ AND ‘surgical treatment’,11 articles were retrieved.Two of them were relevant to preterm twin neonates[10,11],1 article reported 19 cases of preterm infants with PDA who received surgical ligation[11],of whom 6 infants were twins with detailed gestational age and birthweight unrecorded.The time of operation was 35 to 55 min,average of (48.0±15.3) min,during the operation there was no transfusion.Postoperation mechanical ventilation treatment was adopted about 1 to 10 days,average of (3.5±2.3) days.All infants off oxygen after extubation in 3 days.After operation the detection of ultrasound showed no residual shunt.Infants were discharged home 7 to 20 days post-operation,average of (11.0±3.0) days.All infants were cured,there was no massive hemorrhage or death occurred during and after the operation.12 cases were found from literature search, including our 2 cases, of these,2 died,9 were cured and 1 improved significantly.Among 6 cases whose detailed information were available,4 infants were identical twins,2 unknown.Case 1 and 2 were from our NICU,case 3 and 4 from Carvalho's report[8],case 5 and 6 from He Lunde's report[10],see Tab 1.
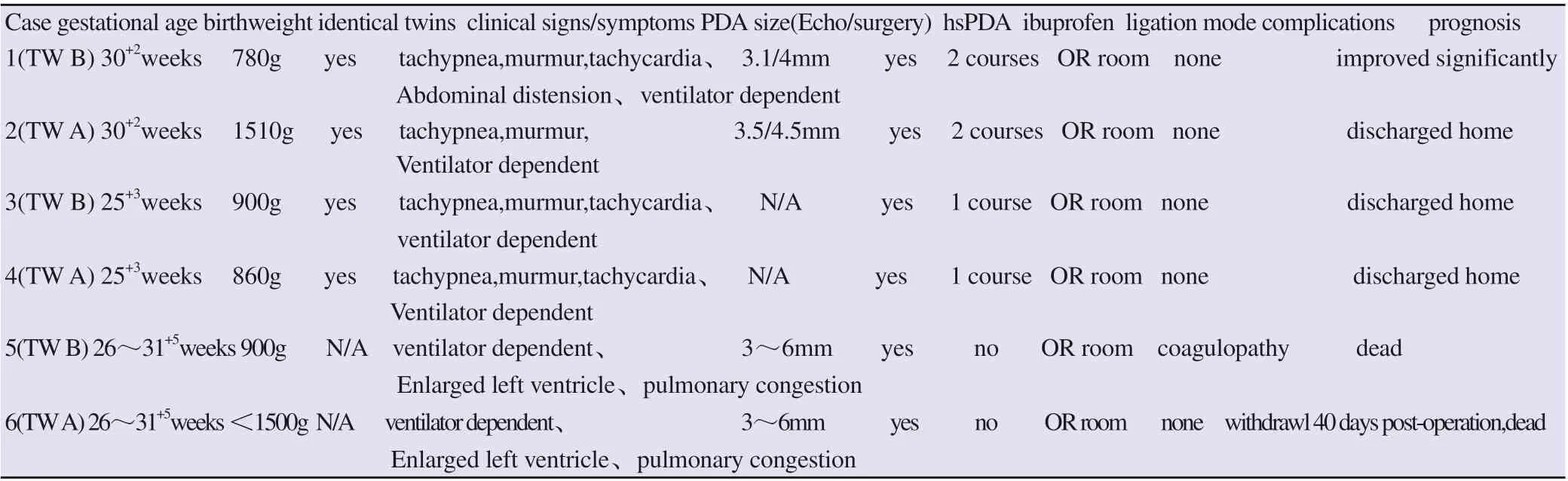
Tab 1 PDA manifestation,Echo,treatment and prognosis of preterm twin neonates
3. Discussion
3.1 Changes in systemic and pulmonary circulation associated with PDA
PDA is a common morbidity in preterm infants, while the ductus remains open, bloodtypically flows left-to-right from the aorta into the pulmonary arteries,this “ductal steal” results in excessive blood flow through the lungs,predisposing to development of pulmonary congestion, pulmonary edema, V/Q mismatch,respiratory failure,escalation of the oxygen and ventilator settings,prolonged mechanical ventilation. Diversion of blood flow from the systemic circulation may exceed capabilities for compensatory increases in total cardiac output,resulting in compromised perfusion of vital organs, including bowel,kidney, and brain[1].
3.2 Definition and clinical manifestation for hsPDA
To date,hsPDA is the hotspot for treatment and research. Despite widespread recognition of the importance of identifying an hsPDA, there remains no consensus on its definition.It normally contains clinical manifestations,echocardiography assessment, defining the population at risk susceptible to PDA,also need to take account of gestational age and postnatal age[12,13]. Wang Chenhong et al[14] concluded that a decreased closure rate of PDA is associated with the lower gestational age,the application of pulmonary surfactant and a larger ductus arteriosus diameter.Some authors proposed to define a hsPDA need to consider: (1) PDA shunt volume and its impact on the systemic and pulmonary circulations; (2) myocardial function evaluation, in particular the relationship between left ventricular (LV) diastolic function in the setting of increased pulmonary blood flow in addition to the contribution of the PDA shunt to coronary ischaemia; and (3) clinical characteristics which can alter the relationship between a PDA and its physiological impact[15,16,17].Diagnosis of hsPDA was made mainly by clinical symptoms,signs and echocardiography,common manifestations include apnea,increased need for oxygen and ventilator settings,metabolic acidosis,tachycardia, increased precordial pulsat ion,hypotension(particularly diastolic),widened pulse pressure(>25 mmHg), persistent murmur at the second intercostal of left margin sternum.Most commonly used echocardiographic parameters to assess hsPDA include ductus arteriosus diameter>1.5 mm,left to right shunting,left atrium to the root of aorta ratio>1.4[18].Other diagnostic criteria include ductus arteriosus diameter>1.5mm,with one of the followings:murmur,tachycardia,tachypnea,widend pulse pressure,hypotension,Corrigan’s pulse,cardiomegaly[19].Our 2 cases both developed hsPDA,series Echocardiography showed evidence of left to right shunting,left atrial and ventricle enlargement, ductus arteriosus diameter>1.5mm,with corresponding clinical manifestation, such as persistent murmur,tachycardia,tachypnea,dyspnea,prolonged ventilation support, hypotension (particularly diastolic,75/36mmHg and 74/32mmHg respectively),widened pulse pressure(39mmHg and 42mmHg,respectively),1 infant present with significant metabolic acidosis(Lac 7.1mmol/L、BE -7.2mmol/L),which were consistent with hsPDA.
3.3 Biomarkers for PDA assessment
Biomarkers have been used to assess hsPDA, urinary excretion of NT-pro B type natriuretic peptide, is also significantly higher in infants with medium to-large PDA compared to those with small PDA[20].NT-pro BNP levels will increase significantly when there is large shunting via ductus arteriosus[21],and there was significant difference with the level of NT-pro BNP in children with heart failure caused by other diseases[22],therefore,it is suitable for monitoring the perioperative period of hsPDA infants.Our 2 cases showed NT-pro BNP levels increased significantly,after ligation,the level dropped significantly,which was consistent with the literature.It imply that NT-pro BNP level may be a promising biomarker for hsPDA assessment and ligation treatment efficacy estimation.
3.4 hsPDA treatment
Treatment of hsPDA is generally divided into drug therapy and surgical ligation. Cyclooxygenase(COX) inhibitors can reduce prostaglandin synthesis.Indomethacin and ibuprofen are commonly used,they are equally effective,however,ibuprofen is more preferred because of its lower incidence of renal impairment, oliguria,gastrointestinal reactions,NEC and other adverse reactions[23].One meta-analysis showed that high dose ibuprofen regimen(1stdose 15-20mg/kg,2ndand 3rddose 7.5-10mg/kg) can increase hsPDA closure rate,compared with standard dosage regimen(1stdose 10mg/kg,2ndand 3rddose 5mg/kg)[24].Olgun H et al found that the second course of ibuprofen in hsPDA preterm infants resulted in a significant increase in the closure rate without increased side effect incidence,thus,surgical ligation should be considered after failed the second course or drug contraindications exist,especially in infants with signs of severe heart failure[25].Retrospective studies showed surgical ligation increase neonatal and neurological morbidity,such as BPD,ROP,cerebral palsy,cognitive delay,visual and hearing impairment[26,27],but Weisz DE et al analysed 754 preterm infants with hsPDA whose gestational age were below 28 weeks, 184 (24%) underwent ligation,compared with drug therapy group,there were no difference in the composite outcome of death or neurodevelopmental impairment at corrected gestational age 18 to 24 months,no differences in chronic lung disease and retinopathy of prematurity[7]. Our 2 cases received series head ultrasound screen,no evidence of IVH or PVL,series ROP screen showed negative,but long term outcome need to be followed up.
3.5 Risk factors for PDA ligation among preterm twin neonates
Congenital heart defect is more common in preterm twins than in preterm singletons,PDA occurred 3.9 times as often in twins as in singletons[4].Being a VLBW monochorionic diamnionic twin is an independent risk factor for symptomatic PDA[28].Birthweight discordance in twins was associated with increased mortality and morbidity, discordance > 30% was associated with higher mortality in the smaller twin and higher morbidities among the smaller and larger twins[29],such as PDA and neurodevelopmental impairment.Our 2 cases were monochorionic diamnionic twins,with birthweight 780g and 1510g,birthweight discordance 48.3%,present with hsPDA symptoms,which was consistent with the above findings.Preterm identical twins have the same genetic basis, the possibility of PDA ligation for both the larger twin and smaller twin should be alerted if the gestaional age is small and birth weight discordance is above 30%.If preterm twins have hsPDA who may fail ibuprofen treatment, surgical ligation should be considered early, and it is safe and effective.
 Journal of Hainan Medical College2020年17期
Journal of Hainan Medical College2020年17期
- Journal of Hainan Medical College的其它文章
- Study of the AQP4 expression in traumatic brain edema and multimodal MRI imaging
- Role of 18F-FDG SPECT / CT imaging in the diagnosis and initial staging of lymphoma
- The value of real-time three-dimensional echocardiography in evaluating left ventricular function for different degrees of heart failure
- Association between polymorphism of MC4R rs489693 gene and disorder of glucose and lipid metabolism in schizophrenia patients treated with olanzapine
- Target prediction and mechanism of Shiyangning in treatment of perianal eczema
- Meta-analysis of traditional Chinese medicine and western medicine in treating retinal vein occlusion complicated by macular edema
